Abstract
Background
Treatments including intralesional corticosteroid injection, pressure therapy, cryotherapy, and various laser therapies have had limited success for keloids and hypertrophic scars.
Objective
This trial evaluated the efficacy of a combination of 578 nm copper bromide laser and the more traditional intralesional corticosteroid injection for the treatment of keloids and hypertrophic scars with respect to scar color.
Methods
Keloids or hypertrophic scars of 12 Korean patients were treated five times by the combined treatment at 4-week intervals. Clinical improvement was assessed by the physicians' global assessment (PGA) comparing pre- and post-treatment photographs, as well as 4 weeks after the last treatment. Erythema intensity was quantified using a mexameter.
Results
Most scars showed significant clinical improvement in PGA and decreased erythema intensity after 5 treatments. All patients showed improvements in symptoms like pruritus.
Conclusion
The combined treatment is effective for keloids and hypertrophic scars, especially when the telangiectatic portion of the scars is prominent. The adjunctive use of 578 nm copper bromide laser decreased the telangiectatic side effects of an intralesional corticosteroid injection by reducing the vascular components of scars.
Keloids and hypertrophic scars are abnormal wound responses in predisposed individuals and represent a connective tissue response to trauma, inflammation, surgery, or burns1. Hypertrophic scars are firm, red or pink, raised scars characterized by an increased expression of collagen. These scars develop as a result of overzealous collagen synthesis coupled with limited collagenolysis during the matrix remodeling phase of wound healing2,3. Keloids are raised, reddish-purple, nodular scars that are firmer than hypertrophic scars. An inherited metabolic alteration in collagen results in a prolonged proliferative phase of healing2,3. The result is thick, hyalinized collagen bundles similar to those produced with hypertrophic scars. However, keloids extend beyond the margins of the original wound and do not regress over time. Histologically they are indistinguishable from one another, since both show formation of whorls and nodules, which persist in keloids, but ultimately flatten out in hypertrophic scars. The diagnosis must therefore be made on a clinical basis4.
A wide variety of treatments have been advocated for keloids and hypertrophic scars. These include topical and intralesional corticosteroid injections, interferon, surgical excision and/or grafting, cryosurgery, radiation, pressure therapy, retinoic acid, and silicone gel sheeting. Unfortunately, the high recurrence rates for keloids and hypertrophic scars, as well as significant side effects that include dyspigmentation and atrophy, have limited the benefits of many of these modalities5.
Many different lasers also have been utilized with varying degrees of success in the treatment of hypertrophic scars and keloids including CO2 and Er:YAG lasers, fractional ablative and non-ablative resurfacing lasers, and pulsed dye laser (PDL)5,6,7. Over the past decade, the vascularspecific 585 nm PDL has been shown to provide long-standing improvement of hypertrophic scars and keloids, as evidenced by significant reduction of scar erythema, height, symptoms, and rigidity2,8. However, PDL is limited by side effects, most commonly postoperative purpura, which often persists for several days9, and produces inconsistent results with poor patient satisfaction10. Intralesional corticosteroid injection in the treatment of hypertrophic scars and keloids has been established for many years. Intralesional corticosteroid injections act by suppressing the inflammatory response, diminishing collagen synthesis, decreasing mucinous ground substance production, and inhibiting collagenase inhibitors that prevent the degradation of collagen11. Adverse effects of corticosteroid injections include telangiectasia, atrophy of skin, and hypopigmentation12.
In this study, we focused on the fact that the vascular component of the scar can improve by therapy targeting microvessels on the lesion. Based on this, adjunctive use of 578 nm copper bromide laser may not only improve telangiectasia caused by intralesional corticosteroid injection but may also lead to improvement of proliferative scars. The purpose of this pilot study was to improve the appearance and symptoms of keloids and hypertrophic scars through thermal action generated by a 578 nm copper bromide laser on the wound healing process. This specific wavelength choice ensured minimal epidermal damage as blood and water cannot absorb this wavelength.
Twelve Korean patients (ages 21~63 years, mean age 34.5 years) with keloids or hypertrophic scars (Table 1) were included in this study. Eleven subjects exhibited telangiectatic erythema within the scars on physical examination before treatment. The cause of the scarring was surgery in five patients and trauma in four patients, with no obvious predisposing cause in three patients. The length of time that the scars had been present varied between 2 and 11 years (mean duration 8.5 years). Patients under 18 years of age and patients with a history of malignant tumor skin disease, bacterial or viral infectious skin disease, immunosuppression, and long-term corticosteroid treatment were excluded. None had received any scar treatments within 6 months of entering the study. All 12 patients were troubled by the raised and erythematous nature of the scars, and six of them suffered from itching. The study was performed in accordance with the Declaration of Helsinki (1975) and was approved by the Institutional Review Board of Chung-Ang University Hospital. Before enrollment, patients were informed of the study procedures, risks, benefits, and complications and gave written informed consent.
All patients were treated with a combination of copper bromide laser at a wavelength of 578 nm (Plus Yellow™; Norseld, Adelaide, SA, Australia) followed by injections using high-dose corticosteroid (triamcinolone acetonide 10 mg/ml). Each patient received the combined treatment six times at 4 week intervals. A contact ice roller was used for epidermal cooling after a chilled, colorless ultrasonic gel was applied directly to the skin. No topical or local anesthetic was used in any of the patients. Treatment fluences ranged from 50 J/cm2 (high power energy), with an emission time (on time) of 300 ms, and an off time of 75 ms. A spot size of 1.0 mm hand piece in contact with the lesion was used in every treatment. General end point was slight bleaching of the visible superficial vessels. After about 5 minutes following laser treatment, they were injected with triamcinolone acetonide at a dose of 10 mg/ml using a 31-gauge needle into the upper dermis of a hypertrophic scar. The injected amount varied between 0.1 ml and 2 ml, depending on the size and number of individual scars. The amount used produced significant blanching under pressure.
The clinical assessment consisted of the physician's global assessment (PGA), intensity of erythema, and patient self-assessment of the scar at each visit. PGA based on photographic documentation were made before each treatment and one month after the final treatment by two independent assessors blinded to the study protocol using a standard quartile grading scale (0: <25%, 1: 25%~50%, 2: 51%~75%, and 3: >75% improvement). For a more objective assessment of the intensity of erythema, each scar of the 12 patients was evaluated by a skin reflectance with a Chromameter CR-400, tristimulus color analyzer (Minolta, Osaka, Japan) before each treatment and one month after the last treatment. This skin color measuring device expressed skin color with the L*a*b* system. This allowed colors to be quantified according to three axes: white-black or lightness (L*), red-green or chrome (a*), and yellow-blue or hue (b*). Of these, the a* parameter measures erythema index. Patient satisfaction resting on related symptoms like itching or burning (0=unsatisfied, 1=slightly satisfied, 2=satisfied, and 3=very satisfied) were also recorded. Patients were queried at each visit concerning treatment-related adverse effects.
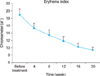
All 12 patients completed the full course of the study. Representative cases that exhibited a marked response are shown in Fig. 1, 2. On PGA, one (8%) patient reported '≤25% improvement' with the treatment, two (17%) reported being '25% to 50% improvement', four (33%) reported being '51% to 75% improvement', and five (42%) patients reported being '≥75% improvement'. The mean score for PGA was 2.17±1.0. The a* values decreased according to the treatments. Quantification of a* at the telangiectatic erythema of the scars revealed a substantial decrease from 18.9 before treatment to 15.3 after one treatment, 13.4 after two treatments, 11.8 after three treatments, 10.2 after four treatments, and 9.4 after five treatments at the 4-week follow-up visit (p<0.01, Fig. 3). Patients' subjective self-assessment score based on the related symptoms was 2.08±0.7 at one month after the final treatment. The results of the PGA and the patients' self-assessment are summarized in Table 1. The most common reported side effects were mild to moderate pain during treatment, and transient erythema and edema after treatment. Only one patient (case 10) showed mild hyperpigmentation of the treated lesion.
Treatment of keloids and hypertrophic scars using a combination of copper bromide laser at a wavelength of 578 nm followed by injections of triamcinolone acetonide produced significant clinical improvement in all study patients. There were no differences between baseline patient characteristics and clinical outcomes, although presternal area is an area of the body with a predilection for formation of poor scars4. Three of our patients had scars located in the presternal area and got satisfying results. Intralesional corticosteroid injections have become a mainstay in the treatment of hypertrophic scar and keloids, alone or in combination with other therapeutic procedures13. Corticosteroid injection can soften and flatten keloids, but cannot narrow hypertrophic scars or eliminate them3. Intralesional corticosteroid injection decreases fibroblast proliferation, collagen synthesis, and glycosaminoglycan synthesis and suppresses pro-inflammatory mediators14.
Copper bromide laser produces two wavelengths that can be emitted separately or together: 511 nm (green) wavelength for the treatment of pigmented lesions and 578 nm (yellow) wavelength for the treatment of various vascular lesions15. It emits light with a short pulse duration of 24 ns. The pulse repetition rate is in the range of 12,000 Hz. This repetition rate is high enough that the beam appears to be continuous to the human eye, that is, quasi-continuous. The individual pulse cannot supply sufficient thermal energy to coagulate the vessels being treated. The summation of thermal energy from numerous pulses will coagulate the vessels16. Favorable results for the reduction of vascular erythema by 578 nm copper bromide laser have already been reported when treating vascular lesions like telangiectasia, port wine stains, spider nevi, and hemangioma10,17,18,19,20,21,22. The 578 nm copper bromide laser is used primarily to reduce erythema, but there is no universal consensus concerning how the 578 nm copper bromide laser works. It likely mediates its effects through selective photothermolysis in which energy emitted from laser is absorbed by oxyhemoglobin at its β-absorption peak, generating heat and leading to thermal injury to the scar microvasculature, leading to ischemia and reducing collagen within a scar23. The very strong hemoglobin absorption at this wavelength and the high energy fluencies can contribute to the excellent results seen in our study22. Telangiectasia (small ectatic blood vessels visible through the skin) can be easily photocoagulated using the 578 nm copper bromide light. However, the authors noted that very large and very small vessels were harder to eradicate20. The main benefits gained from pre-treatment with 578 nm copper bromide laser was the reduction of telangiectasia, which was easily induced by the repetitive intralesional corticosteroid injections, and therefore resulted in a more cosmetically acceptable appearance of the scar4. The side effects evaluated during this study were only mild and transient erythema and edema. Non-purpuric skin changes immediately after radiation are characteristic findings comparing to PDL, in which the end points are purpuric changes at treated sites. The disappearance of the vessel without residual epidermal whitening is the ideal and optimum end point of a vascular lesion and this correlates well with the low reported incidence of post-treatment side effects20.
The results of this pilot study have proven promising, and suggest that the 578 nm copper bromide laser combined with intralesional corticosteroid injection is a good treatment option for the treatment of keloids and hypertrophic scars, especially those accompanied by pronounced telangiectasia, regardless of whether it is due to the effect of intralesional corticosteroid injection or not4. This study is limited by the absence of placebo control and direct comparison with the single modalities. Nevertheless, data on the efficacy of monotherapy with either intralesional corticosteroid injection or lasers for targeting hemoglobin are already published, and our results can be used to design further controlled trials of combination therapies. The other limitation of the study is that evaluation of treatment efficacy at one month after the final treatment seems to be in some degree inappropriate in considering the nature of hypertrophic scars and keloids. Long term follow up more than 3 months after the last treatment should be conducted to assess the worsening.
The 578 nm copper bromide laser combined with intralesional corticosteroid injection can be an effective and safe non-surgical treatment option for patients with keloids and hypertrophic scars. Further studies with a larger sample size and comparing combined intralesional corticosteroid injection and 578 nm copper bromide laser treatment directly with intralesional corticosteroid injection or 578 nm copper bromide laser monotherapies are warranted.
Figures and Tables
 | Fig. 1Keloid on the presturnal area in a 63-year-old man (case 3). (A) Before the initiation of treatment; (B) at 4 weeks after the final treatment. |
 | Fig. 2Hypertrophic scar on the right wrist in a 23-year-old woman (case 12). (A) Before the initiation of treatment; (B) at 4 weeks after final treatment. |
ACKNOWLEDGMENT
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0008687).
References
2. Khatri KA, Mahoney DL, McCartney MJ. Laser scar revision: A review. J Cosmet Laser Ther. 2011; 13:54–62.

3. Wolfram D, Tzankov A, Pülzl P, Piza-Katzer H. Hypertrophic scars and keloids--a review of their pathophysiology, risk factors, and therapeutic management. Dermatol Surg. 2009; 35:171–181.

4. Connell PG, Harland CC. Treatment of keloid scars with pulsed dye laser and intralesional steroid. J Cutan Laser Ther. 2000; 2:147–150.

7. Alster T. Laser scar revision: comparison study of 585-nm pulsed dye laser with and without intralesional corticosteroids. Dermatol Surg. 2003; 29:25–29.

8. Wittenberg GP, Fabian BG, Bogomilsky JL, Schultz LR, Rudner EJ, Chaffins ML, et al. Prospective, single-blind, randomized, controlled study to assess the efficacy of the 585-nm flashlamp-pumped pulsed-dye laser and silicone gel sheeting in hypertrophic scar treatment. Arch Dermatol. 1999; 135:1049–1055.

10. Sadick NS, Weiss R. The utilization of a new yellow light laser (578 nm) for the treatment of class I red telangiectasia of the lower extremities. Dermatol Surg. 2002; 28:21–25.

11. Kiil J. Keloids treated with topical injections of triamcinolone acetonide (kenalog). Immediate and long-term results. Scand J Plast Reconstr Surg. 1977; 11:169–172.

12. Donkor P. Head and neck keloid: treatment by core excision and delayed intralesional injection of steroid. J Oral Maxillofac Surg. 2007; 65:1292–1296.

13. Golladay ES. Treatment of keloids by single intraoperative perilesional injection of repository steroid. South Med J. 1988; 81:736–738.

14. Urioste SS, Arndt KA, Dover JS. Keloids and hypertrophic scars: review and treatment strategies. Semin Cutan Med Surg. 1999; 18:159–171.

15. Dinehart SM, Waner M, Flock S. The copper vapor laser for treatment of cutaneous vascular and pigmented lesions. J Dermatol Surg Oncol. 1993; 19:370–375.

16. Lee HI, Lim YY, Kim BJ, Kim MN, Min HJ, Hwang JH, et al. Clinicopathologic efficacy of copper bromide plus/yellow laser (578 nm with 511 nm) for treatment of melasma in Asian patients. Dermatol Surg. 2010; 36:885–893.

17. Jonell R, Larkö O. Clinical effect of the copper vapour laser compared to previously used argon laser on cutaneous vascular lesions. Acta Derm Venereol. 1994; 74:210–211.
18. van Gemert MJ, Welch AJ, Pickering JW, Tan OT, Gijsbers GH. Wavelengths for laser treatment of port wine stains and telangiectasia. Lasers Surg Med. 1995; 16:147–155.

19. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983; 220:524–527.

20. McCoy SE. Copper bromide laser treatment of facial telangiectasia: results of patients treated over five years. Lasers Surg Med. 1997; 21:329–340.

21. Sheehan-Dare RA, Cotterill JA. Copper vapour laser (578 nm) and flashlamp-pumped pulsed tunable dye laser (585 nm) treatment of port wine stains: results of a comparative study using test sites. Br J Dermatol. 1994; 130:478–482.

22. Yoo KH, Kim BJ, Kim MN. Efficacy of high-energy copper bromide laser (511 and 578 nm) with for deep infantile haemangioma. Clin Exp Dermatol. 2009; 34:e451–e452.
23. Elsaie ML, Choudhary S. Lasers for scars: a review and evidence-based appraisal. J Drugs Dermatol. 2010; 9:1355–1362.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download