Abstract
Background
There are various histological prognostic parameters of cutaneous malignant melanoma, including tumor thickness and ulceration. Tumor-infiltrating lymphocytes (TIL) are among these parameters and can be further classified into three categories: 'absent', 'non-brisk' and 'brisk'. Brisk TIL usually indicates better clinical prognosis. Microscopic satellite (Ms) is defined as a nest of tumor cells that is greater than 0.05 mm in diameter and definitely separated from the main tumor. Even though the incidence of Ms varies according to Breslow thickness, the presence of Ms generally indicates poor prognosis.
Objective
Clinical significance of both TIL and Ms has been extensively studied in western populations but much less so in Asian countries, including Korea, where acral melanoma is the most common subtype.
Methods
We reviewed 90 patients with acral melanoma diagnosed at Kyungpook National University Hospital in Korea. Tissue specimens were examined using hematoxylin-eosin and HMB45 immunohistochemical staining. They were also evaluated by the presence and categorization of TIL (absent, non-brisk and brisk) and the presence of Ms. We further evaluated their impact on survival events (recurrence, distant metastasis and death).
Results
The number of survival events by TIL type was 22 in the absent category (22/64, 34.4%), 3 in the non-brisk category (3/25, 12.0%) and 0 in the brisk category. For Ms, survival events were present in 7 patients in Ms-present group (7/11, 63.6%) and 21 patients in Ms-absent group (21/79, 26.6%).
The histological prognostic parameters of cutaneous malignant melanoma, including acral melanoma, have been the subject of numerous studies undertaken in western populations. Multivariate analyses have demonstrated that tumor thickness is the most powerful predictor of the clinical outcomes of cutaneous melanoma as measured by recurrence, disease-free survival, and overall survival. Other factors such as the Clark level, atypia, mitotic rate, neurotropism or regression are known to be implicated as probable prognostic indicators1. However, even in the West, the role of tumor-infiltrating lymphocytes (TIL) and microscopic satellites (Ms) as prognostic indicators has not been extensively studied, probably because of a lack of consensus surrounding some of their key definitional issues.
Considering the use of TIL, primary cutaneous melanoma is frequently associated with variable degrees of chronic inflammatory cell infiltrates, composed predominantly of lymphocytes. Furthermore this morphologic observation provides an opportunity not only to study what may be the local immunologic attack to the tumor but also to examine the correlation between its presence and survival2,3. The evidence of necrotic tumor cells being associated with lymphocytic infiltration suggests that melanoma cells are being killed by lymphocytes, but this hypothesis is not without controversy4.
Ms are generally defined as discrete tumor nests that are greater than 0.05 mm in diameter and separated from the main body of the tumor by normal reticular dermal collagen or subcutaneous fat, although there is some dispute as to this definition5-7. Only a few studies have evaluated the role of Ms as a prognostic factor in cutaneous melanoma. These studies showed contradictory results5-7.
Acral melanoma has relatively recently been defined as a melanoma of glabrous skin, which is the non-hair-bearing skin characteristic of the palmar, plantar and subungual regions and especially the dorsal area of the hand and the foot8,9. This is the most common subtype of cutaneous malignant melanoma in Asians, and this subtype of melanoma comprises a larger proportion in Asians in comparison to non-Asians. The clinical impact of TIL and Ms on acral melanoma has thus far been rarely evaluated, despite its relatively high prevalence in Asians, including Koreans. Therefore, the purpose of the current study is to evaluate the clinical outcomes of acral melanoma in Koreans according to the presence and category of TIL and the presence of Ms in pathological specimens.
There were one hundred and forty nine cases of cutaneous malignant melanoma in patients visiting Kyungpook National University Hospital (KNUH) between 1993 and 2008. Because the only patients selected were those for whom adequate histology and immunohistochemical study for analysis was available, 90 acral melanomas, which were all located on the hand dorsum, foot dorsum and palmoplantar skin regardless of their clinical staging, formed the basis of the study.
TILs were classified into three categories, i.e. absent, non-brisk, and brisk, according to the criteria suggested by Clark et al.10 and Elder et al.11 as follows: absent TIL indicated there was no lymphocytes or no infiltration of the melanoma; non-brisk TIL indicated that lymphocytes were present in one or more foci of the tumor, either scattered throughout or situated focally in the periphery and finally, brisk TIL was defined as the lymphocytes being present or infiltrating the entire base of the tumor cells10,11.
Ms was defined as the presence of a nest(s) of tumor cells, greater than 0.05 mm in diameter, in the reticular dermis or vessels beneath the principal invasive tumor5,7. The nest(s) had to be separated from the main tumor mass by normal tissue in the section in which the Breslow measurement was made5,7. This differs from angiotropism, which is defined as melanoma cells cuffing the external surface of vessels12. It has been suggested that it is not viable to clearly differentiate between intravascular and perivascular tumor invasion using the currently admitted standard of the presence of vascular structure12,13. However, we assumed that this concept is not at present generally accepted in the dermatopathological field, so we excluded cases showing the definite intravascular presence of tumor cells from the 'Ms' group, whilst being aware of the controversy surrounding this issue.
The formalin-fixed, paraffin-embedded tissue blocks of 90 acral melanomas were reviewed. These were obtained from the Department of Pathology, KNUH. The basic hematoxylin-eosin and immunohistochemistry of HMB45 was highlighted red by 3,3'-diaminobenzidine-amino-9-ethylcarbazole and were evaluated respectively. The slides were reviewed to record the presence and categorization of TIL (absent, non-brisk and brisk) and the presence of Ms. The results were derived from independent histopathological review by one dermatologist and one pathologist on separate occasions. Diagnostic differences between the two examiners' assessments were resolved by consensus. Histological review was performed without knowledge of the clinical outcomes of the included patients.
Clinical outcomes were estimated by survival rates. To better estimate the survival rates, we considered various factors: not only death, but locoregional recurrence and distant metastasis. We used the concept of 'survival events' to represent all the above poor prognostic events that were neal fatal to obtain the survival curve. Survival rates were calculated by the Kaplan-Meier method. Differences between survival curves were computed with the log-rank test. Statistical significance was defined as a p-value of less than 0.05. The relationships between TIL/Ms and the more commonly-used prognostic factor of Breslow thickness were also evaluated from our data. Findings were compared with those from previous reports. A survival event was defined as representing all poor prognostic events that were near fatal.
Of the series of 90 acral melanoma patients, 43 were male and 47 were female. Their ages ranged from 10 to 87 years (median 61.3 year). The most common site was the sole of the foot (30/90, 33.3%), followed by the finger (21/90, 23.3%). The period of follow-up observation ranged from 3~180 months (median 42.9 months).
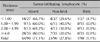
In terms of the clinical outcomes of the 90 acral melanomas, there were 64 cases in the absent category (64/90, 71.1%), 25 in the non-brisk category (25/90, 27.8%) and 1 in the brisk category (1/90, 1.1%) (Table 1).
A significant statistical association was observed between the categories of TIL and the clinical outcome for acral melanoma. Survival events, including locoregional recurrence, distant metastasis and death, developed in 22 patients in the absent category (22/64, 34.4%), 3 in the non-brisk category (3/25, 12.0%) and none in the brisk category (0/1, 0%) (Table 1). The clinical outcomes in the non-brisk category showed a statistically significant better prognosis than was true for the absent category (p=0.037) (Fig. 3A). As for the relationship between Breslow thickness and the incidence of each category of TIL, our data seemed to show that thick melanomas occurred at a rate in the absent category (Table 2).
Of the 90 sampled patients, 11 were in the Ms-present group (11/90, 12.2%) and 79 in the Ms-absent group (79/90, 87.8%) (Table 1).
A significant statistical association was observed between the presence of Ms and clinical outcomes. Survival events developed in 7 cases in the Ms-present group (7/11, 63.6%), compared to 21 cases in the Ms-absent group (21/79, 26.6%) (Table 1). As such, acral melanoma showed a significantly better prognosis in the Ms-absent group than in the Ms-present group (p=0.001) (Fig. 3B).
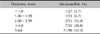
For the relationship between Breslow thickness and the incidence of Ms, our data seemed to show that the incidence of Ms in acral melanoma increased as the thickness increased (Table 3).
The clinical significance of histopathological parameters has not often been studied in relation to the acral sub-type of cutaneous malignant melanoma. However, this sub-type is particularly common in Asian countries, including Korea. Among the parameters, the clinical significance of TIL and Ms have been particularly neglected, probably due to difficulties and ambiguities in their definition and categorization. However, TIL and Ms could be less valuable prognostic factor than Breslow thickess, the Clark level and the mitotic rate, all of which are well known, but it was still regarded as a promising candidate as newly focused prognostic factors.
There have been controversies about the clinical prognostic significance of TIL. For example, as was originally proposed by Clark et al.10, it has been persistently found that the prognosis for patients whose melanoma is involved with the so-called brisk lymphocytic infiltrate was significantly better than for patients whose tumors had little or no inflammation. This work also categorized TIL into three categories, absent, non-brisk and brisk, which were adopted in the current study. Some research has suggested that TILs indicate a good prognosis14. However, others have argued for no clinical significance15. Despite this controversy about the relationship between TIL and melanoma prognosis, the fact that presence of TIL means a better prognostic factor been also reported in bladder16, kidney17, and breast18 carcinomas. In this study, the survival event rate for acral melanomas was 34.4% in the absent category, 12.0% in the non-brisk category and 0.0% in the brisk category. As brisk TIL patients did not show any survival events, they were excluded from the survival curve calculation. The absent TIL category showed a worse prognosis than did the non-brisk category. Therefore this study showed a similar trend as was found in melanoma studies carried out in Western populations.
Of the various prognostic factors of acral melanoma, Ms has not been much studied. To the best of our knowledge, the first study in this area showed that the presence of Ms was associated with a worse prognosis19. This work noted that the 5-year disease-free survival rate was 36.0% for patients with Ms in contrast to 89.0% for patients without Ms. It also demonstrated that the presence or absence of Ms was comparable with histological ulceration in its additive prognostic effect on tumor thickness. Another study found that the presence of Ms was correlated with a greater frequency of local recurrences than occurred in patients without Ms (14.0% vs. 3.0%) in a large series of 3445 patients in Australia with clinical stage I melanoma20. However, in spite of these results, the role of microsatellites as an independent predictor of outcomes remains a point of dispute, an issue that is linked with definitional issues surrounding Ms. For example, Harrist et al.5 included in their analysis of microsatellites not only dermal satellites but also tumor emboli within vascular space as well as tumor islands potentially contiguous with the main body of the tumor. This can potentially explain the higher incidence of microsatellites in this work than was observed in Day et al.19 Different from Harrist et al.5, we excluded definite intravascular tumor cells from the Ms-present group because it was important to differentiate intravascular tumor cells from another important prognostic factor, vascular invasion. In this study, the Ms-present group showed a statistically worse prognosis in acral melanoma, compared to those without Ms. Furthermore locoregional metastasis developed in 3 (27.3%) of the 11 patients in the Ms-present group compared with 7 (8.9%) of 79 patients in the Ms-absent group. Distant metastases also occurred more frequently in 3 (27.3%) of 11 patients in the Ms-present group compared with 5 (6.3%) of 79 in the Ms-absent group. Therefore, the presence of Ms in the matched cohort comparison might appear to be associated with an increase in locoregional and distant metastasis of the disease. In malignant melanoma, locoregional recurrence and distant metastasis are generally known to lead to a catastrophic end result, so not only death but these recurrences and metastasis were included as survival events when calculating the survival curve1,2. Moreover, as the tumor thickness increased, the incidence of Ms also increased. Based on this correlation, our result may be another sign that Ms could, like tumor thickness, also be a potential prognostic indicator. This is in spite of some study limitations, specifically the relatively small number of patients and the retrospective nature of the study.
This report examined a series of 90 Korean acral melanoma patients, investigating the significance of prognostic factors on clinical outcomes. Due to the absence of large-scale studies into the function of TIL and Ms as prognostic factors, these cannot be included in melanoma staging at present. However, after accumulating a stronger theoretical basis through related studies, TIL and Ms could ultimately comprise a part of melanoma staging as is true for mitotic rates in melanoma T staging. In conclusion, this paper suggests the possibility of TIL and Ms being influencing indicators in the prognosis of acral melanomas in the Korean population.
Figures and Tables
Fig. 1
Tumor-infiltrating lymphocytes. (A) Absent group: no lymphocytes are present. (B) Non-brisk group: sparse and isolated groups of lymphocytes are present between melanoma cells. (C) Brisk tumor-infiltrating lymphocytes (TIL) group: lymphocytes diffusely interposed between melanoma cells in the entire vertical growth phase (A~C: H&E, ×100).

Fig. 2
Microscopic satellites (Ms): a discrete tumor nest (red arrowhead) greater than 0.05 mm that is separated from the main body of the tumor by normal reticular dermal collagen (A: H&E, ×100; B: H&E, ×200).

Fig. 3
Survival curve for acral melanomas according to the presence of (A) TIL and (B) Ms tumor-infiltrating lymphocytes and (B) Ms (Kaplan-Meier method) (p<0.05). Brisk TIL patients were not included in survival event analysis because there were no such events for this group. TIL: tumor-infiltrating lymphocytes, Ms: microscopic satellites.
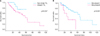
Table 1
Distribution of survival event in acral melanomas by tumor-infiltrating lymphocyte and microscopic satellites in each category

*Survival event included locoregional recurrence, distant metastasis and death. †Categorization of tumor-infiltrating lymphocyte by Clark et al.10
References
1. Nagore E, Oliver V, Botella-Estrada R, Moreno-Picot S, Insa A, Fortea JM. Prognostic factors in localized invasive cutaneous melanoma: high value of mitotic rate, vascular invasion and microscopic satellitosis. Melanoma Res. 2005. 15:169–177.

2. Homsi J, Kashani-Sabet M, Messina JL, Daud A. Cutaneous melanoma: prognostic factors. Cancer Control. 2005. 12:223–229.

3. Mihm MC Jr, Clemente CG, Cascinelli N. Tumor infiltrating lymphocytes in lymph node melanoma metastases: a histopathologic prognostic indicator and an expression of local immune response. Lab Invest. 1996. 74:43–47.
4. Busam KJ, Antonescu CR, Marghoob AA, Nehal KS, Sachs DL, Shia J, et al. Histologic classification of tumor-infiltrating lymphocytes in primary cutaneous malignant melanoma. A study of interobserver agreement. Am J Clin Pathol. 2001. 115:856–860.

5. Harrist TJ, Rigel DS, Day CL Jr, Sober AJ, Lew RA, Rhodes AR, et al. "Microscopic satellites" are more highly associated with regional lymph node metastases than is primary melanoma thickness. Cancer. 1984. 53:2183–2187.

6. León P, Daly JM, Synnestvedt M, Schultz DJ, Elder DE, Clark WH Jr. The prognostic implications of microscopic satellites in patients with clinical stage I melanoma. Arch Surg. 1991. 126:1461–1468.

7. Shaikh L, Sagebiel RW, Ferreira CM, Nosrati M, Miller JR 3rd, Kashani-Sabet M. The role of microsatellites as a prognostic factor in primary malignant melanoma. Arch Dermatol. 2005. 141:739–742.

8. Cunnon B, May JW Jr. Flynn JE, editor. Skin contractures of the hand. Hand surgery. 1982. 2nd ed. Baltimore: Williams and Wilkins;776–777.
10. Clark WH Jr, Elder DE, Guerry D 4th, Braitman LE, Trock BJ, Schultz D, et al. Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst. 1989. 81:1893–1904.

11. Elder DE, Guerry D 4th, VanHorn M, Hurwitz S, Zehngebot L, Goldman LI, et al. The role of lymph node dissection for clinical stage I malignant melanoma of intermediate thickness (1.51-3.99 mm). Cancer. 1985. 56:413–418.

12. Lugassy C, Barnhill RL. Angiotropic melanoma and extravascular migratory metastasis: a review. Adv Anat Pathol. 2007. 14:195–201.
13. Van Es SL, Colman M, Thompson JF, McCarthy SW, Scolyer RA. Angiotropism is an independent predictor of local recurrence and in-transit metastasis in primary cutaneous melanoma. Am J Surg Pathol. 2008. 32:1396–1403.

14. Sober AJ, Chuang TY, Duvic M, Farmer ER, Grichnik JM, Halpern AC, et al. Guidelines of care for primary cutaneous melanoma. J Am Acad Dermatol. 2001. 45:579–586.

15. Barnhill RL. Barnhill RL, editor. Prognostic factors in cutaneous melanoma. Pathology of melanocytic nevi and malignant melanoma. 1995. Boston, MA: Butterworth-Heinemann;269–284.
16. Lipponen PK, Eskelinen MJ, Jauhiainen K, Harju E, Terho R. Tumour infiltrating lymphocytes as an independent prognostic factor in transitional cell bladder cancer. Eur J Cancer. 1992. 29A:69–75.

17. Balch CM, Riley LB, Bae YJ, Salmeron MA, Platsoucas CD, von Eschenbach A, et al. Patterns of human tumor-infiltrating lymphocytes in 120 human cancers. Arch Surg. 1990. 125:200–205.

18. Rilke F, Colnaghi MI, Cascinelli N, Andreola S, Baldini MT, Bufalino R, et al. Prognostic significance of HER-2/neu expression in breast cancer and its relationship to other prognostic factors. Int J Cancer. 1991. 49:44–49.
19. Day CL Jr, Harrist TJ, Gorstein F, Sober AJ, Lew RA, Friedman RJ, et al. Malignant melanoma. Prognostic significance of "microscopic satellites" in the reticular dermis and subcutaneous fat. Ann Surg. 1981. 194:108–112.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download