Abstract
Background
Although ablative fractional resurfacing is known to be effective against photoaging and acne scars, studies on its efficacy, safety and changes in the skin characteristics of Asians are limited.
Objective
The aim of this study is to assess the efficacy and safety of carbon dioxide fractional laser (CO2FL) in Koreans treated for wrinkles and acne scars, and to define the changes in skin characteristics during recovery period.
Methods
We administered one session of CO2FL on 10 acne scar patients and 14 wrinkles patients with skin types IV and V. The surveillance of efficacy and side effects along with the measurement of biophysical properties was carried out before 1 day, 1 week, 1 month and 3 months after treatment.
Results
Using a non-invasive method, skin barrier damage, erythema and bronzing of skin during the recovery period were assessed, and all of the items eventually returned to the pre-treatment level. Skin elasticity was measured in the wrinkle group, and the statistically significant effect was sustained throughout the next three months. The outcome of treatment was found to be better than 'moderate improvement' in both the acne scar and wrinkle groups. Further, there were no serious side effects three months post-procedure.
Conventional carbon dioxide (CO2) and erbium: yttrium-aluminum-garnet (Er:YAG) lasers were considered as the gold standard for skin laser resurfacing1. Despite superior clinical outcomes, this particular modality has been associated with lengthy recovery time and high risk of side effects and complications, particularly in patients with darker skin types2.
The newly developed ablative fractional photothermolysis laser (FL) was designed to minimize these shortcomings of ablative laser while maintaining its clinical efficacy3. Ablative FL results in a microscopic pattern with spatial separation of normal tissues by thermally-affected epidermal and dermal columns. Immunohistochemical studies have revealed that during this peculiar process of wound healing, the induction of epidermal heat-shock protein and collagen remodeling occurs, lasting up to 3 months post-ablative FL treatment in vivo4. This effect may be exploited to treat photoaging, skin tightening, acne scars, non-acne atrophic scars and burn scars5-7. Various adverse effects, however, such as HSV outbreak, bacterial infection, acneiform eruption, erosion, and postinflammatory hyperpigmentation (PIH) are being reported after ablative FL treatment8. Also, earlier studies on ablative FL treatment have found that the ideal candidates for laser interventions by FL are mainly Fitzpatrick skin type I~III individuals, and that the side effects tend to develop more readily in individuals with darker skin types9. PIH, in particular, is a relatively common adverse outcome after ablative FL, and is more likely to occur in darker skin types. Although there are ongoing studies on the efficacy and adverse effects of ablative FL on Asian patients with darker skin types, there is no set standard for optimal treatment frequency, interval and treatment parameters.
Ablative FL can be achieved with an Er:YAG, yttrium-scandium-gallium-garnet (YSGG) or CO2 laser, with the wavelengths exhibited by these lasers being highly absorbed by water10. While various types of ablative FL, on the basis of maximum power, energy and penetration depth, are currently available, a 10,600 nm CO2FL device, which uses pulse energy from 5 to 70 mJ covering 10% to 70% of the treated area in increments of 5%, was used in this study.
The authors were prompted to take on a study that assesses the skin surface characteristics after CO2FL treatment, and investigated its efficacy and safety for moderate to severe acne scars and wrinkles in Korean patients with Fitzpatrick skin types IV and V.
This study included ten patients (all females) with acne scars and another fourteen (2 males and 12 females) with wrinkles who visited the Department of Dermatology at Konkuk University (Seoul, Korea). The age range of the acne scar group was 19 to 44 years (mean age, 31.1), whereas that of the wrinkle group was 35 to 62 years (mean age, 52.9). The subjects' Fitzpatrick skin types fell into either type IV or V. The grade of acne scars and wrinkles in the enrolled patients was each evaluated by a qualitative grading system and a wrinkle severity rating scale, respectively11,12. The grade of the acne scar group was 2 to 3 and that of the wrinkle group was 2 to 4. Informed consent was obtained from all patients before the initiation of treatment. The exclusion criteria included known photosensitivity, pregnancy or lactation, history of hypertrophic or keloid scarring and use of isotretinoin or acne treatments by extraction within the past 6 months. This study was approved by the Institutional Review Board of Ethics Committee of Konkuk University Medical Center (KUH1120008).
Before treatment, the face was cleansed with a mild nonabrasive detergent and gauze soaked in 70% isopropyl alcohol. A topical anesthetic cream (EMLA; AstraZeneca, Wilmington, DE, USA) was applied under occlusive dressing for 30 minutes before being washed off. Additionally, regional nerve block (supraorbital, infraorbital, mental, and infratrochlear) was given with the preparation made from a combination of 1% lidocaine hydrochloride and 1:100,000 epinephrine. Each patient received one full-face treatment with 10,600 nm CO2 fractional laser (CO2FL, Fraxel Repair®; Reliant Technologies Inc., San Diego, CA, USA). Treatment parameter was adjusted according to the severity of acne scars and wrinkles and tolerability of each patient. The treatment parameters for acne scar and wrinkle groups are shown in Table 1. During treatment, the pain level of patients was assessed using a 10-point pain scale (0=no pain, 5=moderate pain, 10=severe pain)13.
The patients were followed-up on 1 day, 1 week, 1 month and 3 months after treatment. Therapeutic outcome was assessed through the patient's self-assessment, study investigators and independent investigators using a global improvement scale three months after treatment (grade 0, no change; grade 1, 1% to 25%=minimal improvement; grade 2, 26% to 50%=moderate improvement; grade 3, 51% to 75%=marked improvement; and grade 4, more than 75%=near total improvement). Standardized digital facial photographs (EOS 400D; Canon Inc., Tokyo, Japan) were taken before treatment and during each follow-up visit using an identical camera setting. Commonly encountered adverse effects, including erythema, edema, pin-point bleeding, oozing and crusting, were graded as 0 to 3 (0, absent; 1, mild; 2, moderate; 3, severe). The presence of hyper/hypo-pigmentation, erosion and infection were recorded as well.
For assessing the changes in the biophysical characteristics, the following devices were used as non-invasive methods prior to treatment and during each follow-up visit: Tewameter, which measures transepidermal water loss (TEWL); Mexameter, which assesses melanin index and erythema index using 16 light emitting diodes reflected by the skin; Sebumeter, which measures sebum excretion; and Reviscometer, which is useful in evaluating the elastic properties and the direction of skin tension lines (MPA5®; Courage & Khazaka Electronic GmbH, Cologne, Germany). For acne scar patients, Tewameter, Mexameter and Sebumeter measurements were taken in the forehead and cheeks. Meanwhile, the forehead, periorbital and perioral regions were chosen in the wrinkle group for Tewameter, Mexameter and Reviscometer measurements. These measurements were conducted in a room with relative humidity of 45%±3% and a temperature of 22℃. All patients were allowed to assimilate to the above setting at least 15 minutes before starting the measurements.
All 24 patients completed the study and showed up for the follow-up visits.
Fig. 1 and Fig. 2 each represent the measured values in the acne scar group and wrinkle group, respectively. TEWL increased sharply on day 1 post-treatment in both groups, before decreasing steadily. Erythema index also increased drastically in both groups one day after treatment, before dwindling steadily. However, in the wrinkle group, a statistically significant increase was sustained up to one month after the treatment, and the value returned to the pre-treatment level three month after treatment. Melanin index tended to elevate one day post-procedurally and level off thereafter, although no statistically significant difference was seen in the acne scar group. The wrinkle group showed a significant increase one day after the procedure, before returning to the normal level one week after, only to show a statistically significant increase again one month after the procedure. Sebum excretion rate measured in the acne scar group increased significantly one day after treatment, and continuously increased thereafter, before returning to the pre-treatment level one month post-treatment. In the wrinkle group, the reviscometer value, which reflects the elasticity of the skin, began to show a statistically significant decrease starting on one day after treatment, and was the lowest one week post-procedure; the trend persisted up to three months.
CO2FL engendered improvement in all types of acne scars, shown through the softening scar contours and decrease in scar depth (Fig. 3). Although less effective in deep lines, the general improvement in skin texture, laxity and fine wrinkles was evident in all wrinkle group patients (Fig. 4). Treatment efficacy was evaluated by a self-assessment of treatment outcome, study investigators and independent investigators three months from the endpoint of treatment. The level of satisfaction in the mean score of the overall degree of improvement by the patients themselves, study investigators and independent investigators were 3.2, 2.9 and 2.9, respectively, in the acne scar group and 3.1, 2.9 and 2.9, respectively, in the wrinkle group (Fig. 5). Overall, the average level of satisfaction was 'moderate improvement' in both the acne scar and wrinkle groups.
The average pain score over the course of treatment was 7.7 and 7.2 in the acne scar and wrinkle groups, respectively, and there was no significant difference between the two groups (p>0.05). Despite the application of local anesthetic cream and facial nerve block, the average pain score was 7.42 (standard deviation [SD] 2.50), which falls into 'severe pain'. However in most patients, discomfort occurred only during the active intervention procedure and resolved immediately after procedure.
Pin-point bleeding, edema and erythema were experienced by all patients immediately after treatment, and oozing, crusting and edema became more severe one day after the treatment. However, these fairly predictable adverse effects improved conspicuously after one week and resolved almost completely within a maximum of three months (Table 2). Time to return to normal life (such as going outdoors and working) varied from four to 100 days, with the average being 14.6 days (SD 15.60) in the acne scar group and 17.0 days (SD 24.69) in the wrinkle group. In two of the 24 patients, both females in their thirties, post-inflammatory hyperpigmentation (PIH) developed one month after treatment, which faded out three months post-treatment. No hypopigmentation, bacterial or viral infection, acneiform eruption, and scarring were observed during the follow-up visits for up to 3 months post-treatment.
This study demonstrates that ablative 10,600 nm CO2FL is an effective treatment modality for acne scars and wrinkles in Asian patients. Moderate improvement was seen in all patients, and near-total improvement was reported in 40% of the acne scar group and 21.4% of the wrinkle group.
CO2FL was developed in an effort to overcome the shortcomings of the traditional ablative lasers and nonablative FL. Its histologic and clinical effect in vivo had first been reported by Hantash et al.4 in 2007. The clinical results are superior to those of non-ablative FL, due to its ability to achieve deep dermal ablation and coagulation. With CO2FL, healing is facilitated by the increase in substances that are known to be involved in wound remodeling, such as heat shock protein, procollagen and dermal elastin, which accumulate around the coagulation column after the formation of ablative microlesions14,15. Early clinical studies using CO2FL primarily involved individuals with lighter skin types16,17. However, now that positive clinical outcomes and safety profiles are being accumulated, a number of studies are also underway to investigate whether similar results may be achieved in Asian patients with darker skin types18-20. Table 33,17-24 reviews previous literatures that involved treating acne scar and wrinkle or photoaging with CO2FL. Compared to other studies with lasers, in this study, the satisfactory outcomes were attained despite the fact that only one treatment session, with relatively low pulse energy, was administered.
The authors measured several biophysical properties using a non-invasive method in order to assess the changes in skin characteristics after CO2FL treatment. In both the acne scar and wrinkle groups, a statistically significant increase of TEWL was seen on one day after treatment, and the value returned to the pre-treatment level roughly one week after treatment. This suggests that the skin barrier remains breached up to one week after treatment and thus, one should be cautious for possible infection; further, application of skin regenerative agents and moisturizer is called for. The transient elevation of erythema and melanin indices after CO2FL treatment may be histologically explained by the elimination of microscopic epidermal necrotic debris (MEND). MEND may typically be observed in the stratum corneum after treatment using fractional resurfacing. It is eliminated transepidermally by keratinocytes, and its migration upward and through the stratum corneum is facilitated by subepidermal clefting, followed by re-epithelialization of the epidermis. All these changes clinically manifest as bronzing and erythema of the skin4,25. During the course of wound healing after CO2FL, various heat shock proteins promote dermal remodeling, with increased collagen synthesis by procollagen chaperone, and activation of fibroblasts. Previous studies have shown that heat shock protein begins to increase several hours after treatment and peaks between 2 and 7 days post-treatment; it remains elevated up to 3 months post-treatment4,26. This finding was in agreement with the results of this study, evidenced by the reviscometer value which gradually decreased and reached the minimum at one week post-treatment in the wrinkle group. Sebum excretion, measured in the acne scar group, gradually increased up to one week post-treatment. Because sebum excretion may cause folliculitis and exacerbate pre-existing acne, meticulous management of sebum excretion through application of topical antibiotics or oral medication may be prudent during this period.
The safety of CO2FL was assessed through a careful observation of any potential adverse effects for up to three month after treatment. Predictable adverse effects of CO2FL treatment, i.e., erythema, edema, pin-point bleeding and oozing, had subsided conspicuously within one week of treatment. However, time to return to normal daily activities, such as going outdoors and working after ablative FL, were 14.6 days and 19.8 days in the acne scar group and wrinkle group, respectively, which were longer than the values stated in previous literatures17,18. Kono et al.27 once have reported that 'obligatory' adverse effects, such as pain, erythema, edema and oozing, have more to do with an increase in density, rather than the energy level. The longer down time in some subjects may also be explained by the relatively large density in these individuals, although a lower energy level was used. Further, PIH, which is known to occur more readily in darker skin type patients, was observed in 8.3% of patients (2 of 24) for up to one month after treatment, although it tended to disappear within three months. Studies on the risk factors of PIH during fractional resurfacing depend largely on treatment parameters, particularly treatment density, and emphasized the role of cooling in order to avoid bulk tissue heating28. Optimal adjustment of the parameters and application aggressive cooling may be helpful in minimizing the incidence of PIH.
In conclusion, we have indicated that CO2FL can be one of the safe and effective treatment options in acne scar and wrinkle patients with darker skin types. Moreover, we have found that the frequency of adverse effects can be minimized through a quantitative measurement of changes in skin characteristics during the recovery period using non-invasive methods, and by administering the appropriate adjuvant treatment. However, future studies exploring the possible combination treatment with other available modalities as well as establishing the standard for optimal treatment parameters and long term clinical data may be valuable.
Figures and Tables
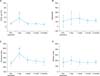 | Fig. 1The changes in skin characteristics measured in the cheek before after and up to three months after being treated with 10,600 nm CO2 fractional laser system in acne scar patients. (A) TEWL, (B) sebum excretion (C) erythema (D) melanin. TEWL: transepidermal water loss, Sebumeter: measurement of sebum excretion rate. *p<0.05; **p<0.01. |
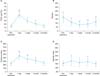 | Fig. 2The changes in skin characteristics measured in the perioral region before, after and up to three months after being treated with 10,600 nm CO2 fractional laser system in 21 wrinkle patients. (A) TEWL, (B) elasticity, (C) erythema, (D) melanin. TEWL: transepidermal water loss, Revisco: Reviscometer, measurement of elasticity. *p<0.05; **p<0.01. |
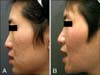 | Fig. 3(A) Acne scars in both cheeks before treatment. (B) Follow-up 3 months after treatment at a pulse energy 20 mJ and density 1,000 microthermal treatment zone/cm2. Both the investigator and the patient reported roughly 60% improvement ('marked improvement'). |
 | Fig. 4(A) Wrinkle severity rating scale grade 3 before treatment. (B) Follow-up 3 months after treatment at a pulse energy 20 mJ and density 1,000 microthermal treatment zone/cm2. Both the investigator and the patient report a more than 75% improvement. |
 | Fig. 5(A) Acne scar group. (B) Wrinkle group. Patients and investigators assessment of clinical improvement 3 month post-treatment using global improvement scale (0, no change; 1, 1%~25%=minimal improvement; 2, 26%~50%=moderate improvement; 3, 51%~75%=marked improvement; 4, more than 75%=near total improvement). |
Table 1
Average energy, total density, and pain score of treatment in both acne scar group and wrinkle group
References
1. Jih MH, Kimyai-Asadi A. Fractional photothermolysis: a review and update. Semin Cutan Med Surg. 2008; 27:63–71.

2. Sriprachya-anunt S, Marchell NL, Fitzpatrick RE, Goldman MP, Rostan EF. Facial resurfacing in patients with Fitzpatrick skin type IV. Lasers Surg Med. 2002; 30:86–92.

3. Chapas AM, Brightman L, Sukal S, Hale E, Daniel D, Bernstein LJ, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008; 40:381–386.

4. Hantash BM, Bedi VP, Kapadia B, Rahman Z, Jiang K, Tanner H, et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007; 39:96–107.

5. Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg Med. 2006; 38:169–176.

6. Tierney EP, Eisen RF, Hanke CW. Fractionated CO2 laser skin rejuvenation. Dermatol Ther. 2011; 24:41–53.

7. Weiss ET, Chapas A, Brightman L, Hunzeker C, Hale EK, Karen JK, et al. Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: quantitative volumetric scar improvement. Arch Dermatol. 2010; 146:133–140.
8. Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008; 58:719–737.

9. Bogdan Allemann I, Kaufman J. Fractional photothermolysis-an update. Lasers Med Sci. 2010; 25:137–144.

10. Brightman LA, Brauer JA, Anolik R, Weiss E, Karen J, Chapas A, et al. Ablative and fractional ablative lasers. Dermatol Clin. 2009; 27:479–489.

11. Goodman GJ, Baron JA. Postacne scarring-a quantitative global scarring grading system. J Cosmet Dermatol. 2006; 5:48–52.
12. Day DJ, Littler CM, Swift RW, Gottlieb S. The wrinkle severity rating scale: a validation study. Am J Clin Dermatol. 2004; 5:49–52.
13. Morgan GE, Mikhail MS, Murray MJ, Kleinman W, Nitti GJ, Nitti JT, et al. Clinical anesthesiology. 4th ed. New York: McGraw-Hill;2006.
14. Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004; 34:426–438.

15. Sasaki GH, Travis HM, Tucker B. Fractional CO2 laser resurfacing of photoaged facial and non-facial skin: histologic and clinical results and side effects. J Cosmet Laser Ther. 2009; 11:190–201.

16. Clementoni MT, Gilardino P, Muti GF, Beretta D, Schianchi R. Non-sequential fractional ultrapulsed CO2 resurfacing of photoaged facial skin: preliminary clinical report. J Cosmet Laser Ther. 2007; 9:218–225.

17. Berlin AL, Hussain M, Phelps R, Goldberg DJ. A prospective study of fractional scanned nonsequential carbon dioxide laser resurfacing: a clinical and histopathologic evaluation. Dermatol Surg. 2009; 35:222–228.

18. Cho SB, Lee SJ, Kang JM, Kim YK, Chung WS, Oh SH. The efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patients. Dermatol Surg. 2009; 35:1955–1961.

19. Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010; 63:274–283.

20. Chan NP, Ho SG, Yeung CK, Shek SY, Chan HH. Fractional ablative carbon dioxide laser resurfacing for skin rejuvenation and acne scars in Asians. Lasers Surg Med. 2010; 42:615–623.

21. Walgrave SE, Ortiz AE, MacFalls HT, Elkeeb L, Truitt AK, Tournas JA, et al. Evaluation of a novel fractional resurfacing device for treatment of acne scarring. Lasers Surg Med. 2009; 41:122–127.

22. Rahman Z, MacFalls H, Jiang K, Chan KF, Kelly K, Tournas J, et al. Fractional deep dermal ablation induces tissue tightening. Lasers Surg Med. 2009; 41:78–86.

23. Tierney EP, Hanke CW, Petersen J, Bartley T, Eckert JR, McCutchen C. Clinical and echographic analysis of ablative fractionated carbon dioxide laser in the treatment of photodamaged facial skin. Dermatol Surg. 2010; 36:2009–2021.

24. Katz B. Efficacy of a new fractional CO2 laser in the treatment of photodamage and acne scarring. Dermatol Ther. 2010; 23:403–406.

25. Laubach HJ, Tannous Z, Anderson RR, Manstein D. Skin responses to fractional photothermolysis. Lasers Surg Med. 2006; 38:142–149.

26. Keagle JN, Welch WJ, Young DM. Expression of heat shock proteins in a linear rodent wound. Wound Repair Regen. 2001; 9:378–385.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download