Abstract
Background
Diabetes is characterized by chronic hyperglycemia, and hyperglycemia can increase reactive oxygen species (ROS) production from the mitochondrial electron transport chain. The formation of ROS in cells induces oxidative stress and activates oxidative damage-inducing genes. There is no research on the protein levels of oxidative damage-related genes AKR1C3 in human diabetic skin. We explored the expression of AKR1C3 in diabetic skin compared with normal skin tissue.
Methods
AKR1C3 expression was evaluated by western blotting in 6 diabetic skin tissue samples and 6 normal skin samples. Immunohistochemical staining was carried out to analyze AKR1C3 expression in the 6 diabetic skin tissue samples (July 2009 to December 2011; Department of Plastic and Reconstructive Surgery at Soonchunhyang University Seoul Hospital, Seoul, Korea).
Diabetes is a serious disease posing a burden on the entire world population. Its damage stems from a number of pathologic mechanisms including oxidative stress. Oxidative stress is closely related to the pathogenesis and complications of diabetes. Oxidative stress is caused by a cascade of reactive oxygen species (ROS) released from the mitochondria, a process which is related to type 1 diabetes (caused by apoptosis of pancreatic beta-cells), and type 2 diabetes, (caused by insulin resistance)1. Since hyperglycemia may increase oxidative stress, the pathologic mechanisms involved in the natural history of diabetes are complex2.
While cells have a range of defense mechanisms against free radicals, free radicals which bypass the defense system attack and modify sub-cellular components, including proteins, lipids and nucleic acids3. Proteins are a prominent target of oxygen free radicals and other reactive species. Metals which have been catalyzed via protein oxidation add carbonyl groups (aldehydes and ketones) in a site-specific manner at lysine, arginine, proline or threonine residues4-7. An increase in reactive carbonyls, caused by both oxidative and nonoxidative reactions (defined as carbonyl stress), promotes chemical modification of proteins and induces oxidative stress and tissue damage as its final step.
The carbonyl compound level is reduced via the simultaneous action of multiple sets of carbonyl reducing enzymes, such as aldo-keto reductases (AKR). While the physiological functions of AKR1Cs have yet to be confirmed, it is thought that they play an important role in maintaining steroid homeostasis in steroid target tissues, and they are known to catalyze the reductive detoxification of reactive aldehydes and ketones, the products of oxidative stress8.
The aim of this study was to investigate the expression of AKR1C3 in vivo. We hypothesized that AKR1C3 protein expression will be less in diabetic skin tissue than in normal skin tissue. We studied the expression of AKR1C3 in normal skin tissues and diabetic skin tissues to describe the relationship between AKR1C3 and diabetic skin tissue, by using western blot and immunochemistry. This study demonstrated that AKR1C3 was found to be less expressed in diabetic skin tissue, by western blot and immunohistochemistry.
The Institutional Review Board (IRB) of Soonchunhyang University Seoul Hospital reviewed and approved this research protocol involving the use of tissue samples. A total of 6 normal skin tissue samples and 6 diabetic skin samples were obtained from patients who underwent surgery between July 2009 and December 2011 in the Department of Plastic and Reconstructive Surgery at Soonchunhyang University Seoul Hospital in Korea. Informed consent was obtained from the patients before surgery. The normal skin tissues were collected from the back of 6 women who had breast reconstruction with a latissimus dorsi flap. Diabetic skin samples were obtained from patients undergoing amputation surgery. A portion of the specimens were frozen in liquid nitrogen immediately after resection for western blot analysis, and stored at -80℃ degrees. For the immunohistochemical studies, the stored formalin-fixed and paraffin-embedded samples, including 6 diabetic skin samples and 6 normal skin tissue samples were used.
Tissue samples were homogenized in whole cell extract lysis buffer (25 mM HEPES [pH 7.7], 0.3 M NaCl, 1.5 mM MgCl2, 0.2 mM ethylenediamine tetraacetic acid, 0.1% Triton X-100, 0.5 mM dithiothreitol, 20 mM-glycerolphosphate, 0.1 mM Na3VO4, 2 g/ml leupeptin, 2 g/ml aprotinin, 1 mM phenylmethylsulfonyl fluoride, and a protease inhibitor cocktail tablet [Boehringer Mannheim, Mannheim, Germany]). The tissue suspension was rotated at 4℃ for 10 minutes, and the supernatants were collected, kept at -70℃ and used for western blotting. Proteins from the tissue were separated by sodium dodecyl sulfate polyacrylamide gel electrophoresis using NuPAGE 4% to 12% bis-Tris gels (NP0335Box; Invitrogen, Carlsbad, CA, USA) and then transferred to an Immobilon-P membrane. The membrane was blocked using 5% BSA in TBS-T (20 mM Tris, pH 7.6, 130 mM NaCl, and 0.1% Tween 20) solution. It was reacted with the primary antibodydiluted to 1:1,000 concentration at 4℃ for 16 hours, and with washing buffer and TBST buffer (10 mM Tris-Cl, pH 8.0, 150 mM NaCl, 0.05% Tween 20), washed well 4 times for 10 minutes, 10 minutes, 15 minutes and 15 minutes and reacted with anti-mouse immunoglobulin G (SC-2005; Santa Cruz, Santa Cruz, CA, USA)-horseradish peroxidase-linked species-specific whole antibody diluted to 1:10,000 for 1 hour. After the reaction with the secondary antibody, it was washed well 4 times for 10 minutes, 10 minutes, 15 minutes and 15 minutes. Proteins on the membrane were detected using the enhanced chemiluminescence solution kit (Amersham Pharmacia Biotech UK Limited, Little Chalfont, UK). The membranes were stripped and reblotted with anti-actin antibody (catalog number Sigma A5441). Primary antibody AKR1C3 (catalog number Sigma A6229-clone NP6.G6.A6) was purchased from Sigma-Aldrich Corporation (St. Louis, MO, USA).
Paraffin sections (4 µm) were deparaffinized in xylene, rehydrated in 10 mM citrate buffer (pH 6.0), and heated in a microwave oven for 15 minutes to restore antigens. To suppress endogenous peroxidase within the tissues, the samples were treated with 3% peroxide for 5 minutes, then with a blocking solution for 30 minutes. The slides were incubated with the primary antibody in a humidity chamber for 60 minutes. Tissue staining was visualized with a 3,3'-diaminobenzidine (DAB) (ScyTek, Logan, UT, USA) substrate chromogen solution.
The primary antibody AKR1C3 (Catalog number Sigma A6229-clone NP6.G6.A6) was purchased from Sigma-Aldrich Corporation.
Relative levels of expression of each protein were analyzed by Phosphor-Imager software (TINA; Raytest, Straubenhardt, Germany).
The measured amounts of expression of the diabetic skin tissues and normal skin were compared.
The data from the Raytest TINA software were analyzed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA) and the statistical significance was set at a p-value less than 0.05. Data are presented as median (interquartile range). For a comparison of non-normally distributed variables we used the Mann-Whitney U test.
The results of the western blot analysis showed that AKR1C3 was less expressed in diabetic skin tissues compared with normal human skin tissues (Fig. 1).
The median of normal skin tissues was 0.935 (interquartile range, 0.911 to 0.973), and the median of diabetic skin tissues was 0.698 (interquartile range, 0.671 to 0.781).
There were significant differences in protein expression between normal skin and diabetic skin (Mann-Whitney U test; p<0.05).
The amount of expression in western blotting shown graphically depicts less expression in diabetic skin tissues compared with normal human skin tissues (Fig. 2).
The immunohistochemical study showed that the AKR1C3 protein was expressed in normal skin tissue with moderate-to-strong positivity. It was expressed in diabetic skin with weak positivity.
The immunohistochemical study further supported the results of the western blot analysis by showing that AKR1C3 expression was decreased in diabetic skin compared with normal skin tissue (Fig. 3).
Strong evidence points to the important role of oxidative stress in tissue damage related to diabetes9. Increased insulin resistance and the reduced insulin secretory response lead to impaired glucose tolerance, leading to oxidative stress by producing higher levels of mitochondrial ROS10, nonenzymatic glycation of proteins11,12, and glucose autoxidation9,13.
ROS plays a crucial role in the activation of stress sensitive signaling pathways regulating the expression of genes responsible for cellular damage14,15. It is hypothesized that ROS and the resulting oxidative damage are involved in the pathogenesis and complications of diabetes2,16.
Proteins are significant targets for oxidative challenge. ROS are able to modify the arginine, lysine, threonine and proline residues of carbonyl groups. Free radicals and other reactive species attack proteins. Oxidative modification of proteins modifies methionine, histidine, and tyrosine residues and forms cysteine disulfide bonds4,17-19. Metals which catalyze protein oxidation add carbonyl groups (aldehydes and ketones) at lysine, arginine, proline or threonine residues in a site-specific manner4-7. Carbonyl groups of proteins are proposed as reliable markers of oxidative stress and are used for marking oxidative modification of proteins20. Elevated protein carbonyl levels were detected in type-1, type-2 and experimental diabetes21-25, and protein carbonyl content is closely related to complications associated with diabetes26. In the results of oxidative stress, the main mechanisms of endogenous reactive carbonyl production include lipid oxidation, lipid peroxidation, glycation product oxidation or glycoxidation. In vivo, DNA and protein damage is oftentimes more important than lipid damage in relation to oxidative stress27. Cells typically eliminate oxidized proteins by proteolysis since oxidized proteins become inactive, and their unfolding makes them more susceptible to proteinases.
A range of NADPH-dependent enzymes from several oxidoreductase families reduce carbonyl groups. AKRs form a large family of monomeric or dimeric NADP(H)-ependent enzymes which includes steroids, eicosanoids, polyols and xenobiotics28. It should be noted that these enzymes exhibit two different types of xenobiotic activities: the activation of NADP+-dependent trans-dihydrodiol dehydrogenase in relation to dihydrodiols derived from activated polyaromatic hydrocarbons29 and the activation of NADPH-dependent xenobiotic carbonyl reductase, in relation to a number of pharmacologically and toxicologically relevant substances30.
It is well-known that diabetes increases oxidative stress in both animal models and patients with diabetes2,16. A number of clinical experiments support the possibility that oxidative stress alters the intracellular signaling pathway which induces insulin resistance, and show that insulin sensitivity in insulin-resistant individuals can be improved with treatment using acetyl-L-cysteine31, vitamin E, vitamin C and glutathione32,33.
AKR are a large family of NADPH-dependent enzymes, which are crucial in reducing aldehydes to alcohols34. This superfamily includes more than 100 members, and in humans, 10 enzymes are divided into the subfamilies of AKR1A, AKR1B, AKR1C, AKR1D and AKR7A35.
They are expressed in a wide range of tissues, including the liver, brain and kidneys36. AKR are involved in the metabolism of sugars, steroids, prostaglandins, and other metabolites, and they also metabolize the aldehydes produced as a result of oxidative stress. In humans, AKR1C enzymes are able to oxidize polycyclic aromatic hydrocarbon trans-dihydrodiol, which is close to a carcinogen, and these enzymes are known as hydroxysteroid dehydrogenases, which can reduce toxic aldehydes36,37. In this study, AKR1C3 was measured in diabetic skin tissue and normal tissue with western blot and immunohistologic methods, as an indicator of oxidative stress. To our knowledge, AKR1C3 in diabetic skin tissue and normal tissue has not yet been studied. We show that the AKR1C3 protein level is less expressed in diabetic skin tissue compared with normal skin tissue.
The immunohistochemical method further supported the results of AKR1C3 expression as measured by western blot analysis.
We believe that diabetic skin tissue contains a relatively small amount of AKR1C3 enzymes and these cannot protect against oxidative stress.
Figures and Tables
Fig. 1
AKR1C3 protein was expressed on normal skin tissue, diabetic skin tissue by western blot analysis. Beta actin used as a loading control in western blot analysis.
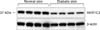
Fig. 2
The median of normal skin tissues was 0.935 (interquartile range, 0.911 to 0.973), and the median of diabetic skin tissues was 0.698 (interquartile range, 0.671 to 0.781). There were significant differences AKR1C3 protein expression between normal skin and diabetic skin(Mann-Whitney U test, p<0.05).

References
1. Bonnefont-Rousselot D, Bastard JP, Jaudon MC, Delattre J. Consequences of the diabetic status on the oxidant/antioxidant balance. Diabetes Metab. 2000; 26:163–176.
3. Chance B, Sies H, Boveris A. Hydroperoxide metabolism in mammalian organs. Physiol Rev. 1979; 59:527–605.

4. Stadtman ER. Oxidation of free amino acids and amino acid residues in proteins by radiolysis and by metal-catalyzed reactions. Annu Rev Biochem. 1993; 62:797–821.

5. Farber JM, Levine RL. Sequence of a peptide susceptible to mixed-function oxidation. Probable cation binding site in glutamine synthetase. J Biol Chem. 1986; 261:4574–4578.

6. Climent I, Tsai L, Levine RL. Derivatization of gamma-lutamyl semialdehyde residues in oxidized proteins by fluoresceinamine. Anal Biochem. 1989; 182:226–232.

7. Levine RL. Oxidative modification of glutamine synthetase. I. Inactivation is due to loss of one histidine residue. J Biol Chem. 1983; 258:11823–11827.

8. Ellis EM. Reactive carbonyls and oxidative stress: potential for therapeutic intervention. Pharmacol Ther. 2007; 115:13–24.

9. Wolff SP, Dean RT. Glucose autoxidation and protein modification. The potential role of 'autoxidative glycosylation' in diabetes. Biochem J. 1987; 245:243–250.

10. Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001; 414:813–820.

11. Brownlee M, Cerami A. The biochemistry of the complications of diabetes mellitus. Annu Rev Biochem. 1981; 50:385–432.

13. Wolff SP, Jiang ZY, Hunt JV. Protein glycation and oxidative stress in diabetes mellitus and ageing. Free Radic Biol Med. 1991; 10:339–352.

14. Dröge W. Free radicals in the physiological control of cell function. Physiol Rev. 2002; 82:47–95.

15. Allen RG, Tresini M. Oxidative stress and gene regulation. Free Radic Biol Med. 2000; 28:463–499.

16. Baynes JW. Role of oxidative stress in development of complications in diabetes. Diabetes. 1991; 40:405–412.

17. Davies KJ, Delsignore ME, Lin SW. Protein damage and degradation by oxygen radicals. II. Modification of amino acids. J Biol Chem. 1987; 262:9902–9907.

18. Uchida K, Kawakishi S. Site-specific oxidation of angiotensin I by copper(II) and L-ascorbate: conversion of histidine residues to 2-imidazolones. Arch Biochem Biophys. 1990; 283:20–26.

19. Heinecke JW, Li W, Daehnke HL 3rd, Goldstein JA. Dityrosine, a specific marker of oxidation, is synthesized by the myeloperoxidase-hydrogen peroxide system of human neutrophils and macrophages. J Biol Chem. 1993; 268:4069–4077.

20. Chevion M, Berenshtein E, Stadtman ER. Human studies related to protein oxidation: protein carbonyl content as a marker of damage. Free Radic Res. 2000; 33:Suppl. S99–S108.
21. Domínguez C, Ruiz E, Gussinye M, Carrascosa A. Oxidative stress at onset and in early stages of type 1 diabetes in children and adolescents. Diabetes Care. 1998; 21:1736–1742.

22. Cakatay U, Telci A, Salman S, Satman L, Sivas A. Oxidative protein damage in type I diabetic patients with and without complications. Endocr Res. 2000; 26:365–379.

23. Telci A, Cakatay U, Salman S, Satman I, Sivas A. Oxidative protein damage in early stage Type 1 diabetic patients. Diabetes Res Clin Pract. 2000; 50:213–223.

24. Jang YY, Song JH, Shin YK, Han ES, Lee CS. Protective effect of boldine on oxidative mitochondrial damage in streptozotocin-induced diabetic rats. Pharmacol Res. 2000; 42:361–371.

25. Cederberg J, Basu S, Eriksson UJ. Increased rate of lipid peroxidation and protein carbonylation in experimental diabetic pregnancy. Diabetologia. 2001; 44:766–774.

26. Altomare E, Grattagliano I, Vendemaile G, Micelli-Ferrari T, Signorile A, Cardia L. Oxidative protein damage in human diabetic eye: evidence of a retinal participation. Eur J Clin Invest. 1997; 27:141–147.

27. Dean RT, Fu S, Stocker R, Davies MJ. Biochemistry and pathology of radical-mediated protein oxidation. Biochem J. 1997; 324:1–18.

28. Jez JM, Bennett MJ, Schlegel BP, Lewis M, Penning TM. Comparative anatomy of the aldo-keto reductase superfamily. Biochem J. 1997; 326:625–636.

29. Palackal NT, Lee SH, Harvey RG, Blair IA, Penning TM. Activation of polycyclic aromatic hydrocarbon trans-dihydrodiol proximate carcinogens by human aldo-keto reductase (AKR1C) enzymes and their functional overexpression in human lung carcinoma (A549) cells. J Biol Chem. 2002; 277:24799–24808.

30. Matsunaga T, Shintani S, Hara A. Multiplicity of mammalian reductases for xenobiotic carbonyl compounds. Drug Metab Pharmacokinet. 2006; 21:1–18.

31. Haber CA, Lam TK, Yu Z, Gupta N, Goh T, Bogdanovic E, et al. N-acetylcysteine and taurine prevent hyperglycemia-induced insulin resistance in vivo: possible role of oxidative stress. Am J Physiol Endocrinol Metab. 2003; 285:E744–E753.

32. Paolisso G, Giugliano D. Oxidative stress and insulin action: is there a relationship? Diabetologia. 1996; 39:357–363.

34. Jin Y, Penning TM. Aldo-keto reductases and bioactivation/etoxication. Annu Rev Pharmacol Toxicol. 2007; 47:263–292.
35. Hyndman D, Bauman DR, Heredia VV, Penning TM. The aldo-keto reductase superfamily homepage. Chem Biol Interact. 2003; 143-144:621–631.

36. O'connor T, Ireland LS, Harrison DJ, Hayes JD. Major differences exist in the function and tissue-specific expression of human aflatoxin B1 aldehyde reductase and the principal human aldo-keto reductase AKR1 family members. Biochem J. 1999; 343:487–504.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download