Abstract
Background
Recently, photodynamic therapy (PDT) has been shown to be an effective first-line treatment for actinic keratosis (AK). However, a major limitation of PDT is the long incubation time required to allow penetration of the photosensitizer.
Objective
The aim of this study was to assess if pretreatment with an ablative carbon dioxide (CO2) fractional laser can reduce the incubation time of the photosensitizer.
Methods
Initially, 29 patients with a total of 34 AK lesions were treated with an ablative CO2 fractional laser at Ajou University Hospital between January and December 2010. Immediately after the laser treatment, topical 20% 5-aminolevulinic acid or methyl-aminolevulinate was applied to the AK lesions and incubated for 70 to 90 minutes. Then, the treated areas were illuminated with a red light source. Improvement was clinically or histologically assessed eight weeks after the treatment.
Results
In spite of the short incubation time, 24 lesions (70.6%) showed a complete response (CR) within three sessions of PDT (10 lesions a clinical CR and 14 lesions a clinical/histological CR). There were no significant side effects associated with the combination of ablative CO2 fractional laser and PDT.
Actinic keratosis (AK) is the most common cutaneous, pre-cancerous lesion consisting of proliferations of cytologically aberrant epidermal keratinocytes1. The risk for progression of AK to squamous cell carcinoma reported in the literature varies from less than 1 percent to 20 percent2. Because of the high incidence of AK, and because the lesions often are located in cosmetically sensitive areas such as the face, it is imperative to use efficacious therapies that give the best cosmetic results; thereby providing the highest patient satisfaction3. During recent years, several therapeutic modalities have been available for the treatment of superficial skin cancer. One of those is photodynamic therapy (PDT), which involves the activation of a photosensitizer using visible light4. Currently, two photosensitizers for topical PDT of AK have received 20% 5-aminolevulinic acid (ALA) and the methyl ester of ALA, methyl-5-amino-4 oxopentanoate (MAL)5,6. The major drawback of AK treatment using PDT is the long incubation time (3 to 4 hours) of the photosensitizer.
Ablative fractional resurfacing (AFR) is a new therapeutic concept that creates microscopic vertical holes of ablated tissue, each surrounded by a thin layer of coagulated tissue, that constitute microscopic treatment zones. Theoretically, AFR may also facilitate the penetration and distribution of topically applied drugs, since the ablated laser holes extend into the dermis, thereby possibly acting as channels for drug uptake7.
The aim of the present study was to evaluate the efficacy and safety of the use of PDT, with a short incubation period for the photosensitizer, for the treatment of AK, after ablative CO2 fractional laser pretreatment.
Twenty-nine Korean patients (7 males and 22 females, mean age 68.4±11.1 [mean±standard deviation, years]) with a total of 34 AK lesions, which had been diagnosed histologically, were enrolled between January and December 2010 at Ajou University Hospital, Suwon, Korea. Exclusion criteria were as follows: pregnancy or lactation; history of photosensitive disorder; known allergy to components of the photosensitizer; history of arsenic exposure, previous use of the following treatments on the face within six months prior to study initiation: ablative laser procedures, dermabrasion, chemical peel, cryotherapy, curettage, surgical excision, or chemodestruction. The patients who had participated in any other investigational study during the treatment period or were likely to be poorly compliant were also excluded. Concomitant treatments with any other immunosuppressive medication were prohibited.
This study was approved by the institutional review board (IRB number: AJIRB-MED-MDB-10-194) of Ajou University Hospital. A summary of baseline characteristics can be found in Table 1.
Initially, the stratum corneum was removed using a surgical blade in the case of hyperkeratotic AK lesions. Just prior to applying the topical photosensitizer, all AK lesions were treated with a single pass of ablative CO2 fractional laser (eCO2®; Lutronic Inc., Seoul, Korea). Single-pulse treatment parameters were as follows: a pulse energy of 50 mJ, a spot density of 100 spots/cm2, a power of 30 W and a 120 µm of beam size. The ablative CO2 fractional laser was applied on the entire area of the AK lesions. Immediately after each fractional laser treatment, 17 lesions were treated with ALA solution (Levulan®; DUSA Pharmaceuticals, Wilmington, MA, USA), with an incubation period of 90 minutes, and an occlusive polyurethane dressing (Tegaderm®; 3M, Minneapolis, MN, USA) was applied to the AK lesion. Also, MAL cream was applied to 17 lesions (Metvix®; Galderma S.A., Paris, France), with an incubation period of 70 minutes, by the same method (Table 1).
Before illumination, the fluorescence of the lesion treated with the photosensitizer was documented with an ultraviolet light emitting device (Janus®; PSI Inc., Suwon, Korea) (Fig. 1). Then, the lesions were illuminated with a red light (600 to 720 nm) using the Waldmann PDT 1200L® (Waldmann-Medizin-Technik, Villingen-Schwenningen, Germany) with ALA, at a light dose of 100 J/cm2 and a fluence rate of 100 mW/cm2, or the Aktilite® CL 128 (Galderma S.A.) with MAL, at a light dose 37 J/cm2. Irradiation was performed with a single pass.
Eight weeks after the treatment, the effect of the PDT was evaluated. Two investigators evaluated the clinical improvement as a complete response (CR: complete removal of the lesion), a partial response (PR: 25% to 99% reduction in lesion) or no response (NR: 0% to 24% reduction in lesion). Histological improvement was evaluated as a CR (complete disappearance of atypical keratinocytes) or a non-CR incomplete disappearance of atypical keratinocytes). If a lesion showed a clinical CR, a skin biopsy was performed to confirm whether the AK had been resolved. If the patient refused the skin biopsy, we observed the status of the AK lesion eight weeks later. Whether the follow up biopsy was performed depended exclusively on the patients' consent. When a residual AK lesion was observed clinically or a skin biopsy proved that the lesion remained, we conducted the next PDT. If the next PDT had no effect, the therapy mentioned above was repeated. Each treatment was performed at intervals of 8 weeks (Fig. 2). One year after the last treatment, one of the dermatologists who participated in the initial assessment telephoned the patients who had shown clinical or histological CR to ask about recurrence.
Adverse events, including pain, phototoxic reactions (e.g., erythema, crusting, and ulceration), and pigmentary changes that occurred during therapy were recorded.
There were a total of 34 AK lesions (25 patients with a solitary AK, 3 patients with two AK lesions, and a patient with three lesions). Twenty-two lesions were located on the cheek, 6 lesions on the nose or perinasal area, 4 lesions on the forehead, and 2 lesions on the back or leg. The treatment results were as follows. Twenty-four lesions (70.6%) showed a CR within three sessions of PDT (10 lesions showed a clinical CR and 14 lesions showed a clinical/histological CR) (Fig. 3, 4). After a single treatment, 10 lesions achieved a clinical CR. In 13 lesions, a CR was observed after two treatment sessions (6 lesions a clinical CR and 7 lesions a clinical/histological CR). One lesion in case 22 showed a clinical and histological CR after three treatment sessions. The average number of treatments to a CR was 1.68±0.63. Six lesions showed a clinical or histopathological PR in spite of two or three PDT sessions. One lesion in case 28 and 29 showed a clinical and histopathological NR despite 2 and 4 sessions of PDT, respectively. The patients who showed a PR or NR were treated by cryosurgery. These results have been summarized in Table 1.
One lesion in case 10 recurred 6 months after the PDT. Other cases were not recurrences of those AK lesions that had achieved clinical CR after 6 months.
The treatment was generally well tolerated, although 5 patients experienced tolerable pain during the procedure. The pain resolved after the treatment without analgesics. No complications such as pigmentary changes or scarring were observed.
Many therapies for AK exist; however, physicians and patients reported dissatisfaction with these modalities. The first category of AK therapies is ablative, including techniques such as curettage and electrodessication and cryotherapy. Disadvantages of this approach include hypopigmentation, scarring, and limitation in the body surface area treated. The second category of AK therapies is topical chemotherapy, the prototype being topical fluorouracil, with the additions of topical imiquimod and diclofenac. Disadvantages of this approach include the need for high patient compliance, marked erythema and crusting, a long recovery period, and high treatment failure rate due to noncompliance3,4. Recently, PDT using a topically applied photosensitizer has been shown to be a highly effective first-line treatment, with excellent cosmesis8. However, the recommended treatment regimen requires a relatively long incubation time with ALA (4 hours) and MAL (3 hours) before illumination3,5. In the present study, after the use of an ablative CO2 therapeutic laser, incubation times of only 90 minutes for ALA were required (37.5% of recommended 4 hours). To match the ratio of the recommended regimen, we set up the MAL-PDT with 70 minutes (38.9% of recommended 3 hours) of incubation time.
With the topical application of the photosensitizer, only two basic factors remain that limit its application within dermato-oncology: 1) Sufficient concentration of the photosensitizer in the tumor, and 2) sufficient light penetration through the whole depth of the tumor9. Previous attempts to improve the bioavailability of the photosensitizer at deeper skin layers include biomodulation of drugs and the stratum corneum (e.g., drug-vehicle optimization, iontophoresis and electroporation), as well as physical modulation techniques such as microneedling or topical keratolytic agents mediated intradermal delivery of the photosensitizer10-13. In addition, traditional CO2 lasers (10,600 nm) and erbium YAG lasers (Er:YAG laser, 2,940 nm) have been used to increase the uptake of the photosensitizer by the tumor cells11-14.
AFR damages a fraction of the skin while leaving microscopic intervening areas of unexposed skin that are capable of remodeling the skin without scarring15. It has been suggested that ablative or fractional laser pretreatment is a useful method of enhancing skin penetration and the fluorescence induction of photosensitizers for PDT in clinical practice. Recently, Haedersdal et al.7 evaluated drug delivery by ablative fractional CO2 laser using MAL, a porphyrin precursor, as a test drug; they suggested that AFR appears to be a clinically practical means for enhancing the uptake of MAL and, presumably, many other topical skin medications. Yoo et al.16 reported enhanced efficacy of PDT with MAL in recalcitrant periungual warts after ablative CO2 fractional laser application, in a pilot study. They demonstrated that ablative CO2 fractional laser treatment is effective for the absorption of MAL and ALA because of their greater depth of penetration, the large diameter of the laser spot, and the drying or coagulation character, which enhances the absorption of MAL or ALA without bleeding. Furthermore, ablative CO2 fractional laser treatment does not form an epidermal necrotic zone. We propose that a combination of CO2 fractional laser pretreatment and PDT might be also effective for the treatment of AK and to reduce the incubation time of the photosensitizer.
In several open studies of ALA-PDT on face or scalp AK in Caucasians, clearance rates were reported to have been 68% to 100% after a single treatment17. A Japanese study, which reported on the efficacy of ALA-PDT for AK, reported a 66% clearance rate for facial lesions, which required three to four treatment sessions to achieve this18. The fact that multiple treatment sessions were required to achieve a higher clearance rate implies some ethnic differences in terms of the response to topical PDT, owing to skin color differences17. However, despite the short incubation time of the photosensitizer, in the present study of Korean patients, 24 of 34 AK lesions (70.6%) showed a CR within three sessions of PDT. This suggested that the combination of ablative CO2 laser application and PDT retains efficacy but reduces the number of required treatment sessions and the incubation time of the photosensitizer.
In our study, the treatment efficacy between ALA-PDT and MAL-PDT was different. The efficacy of ALA-PDT (88.2%) was better than MAL-PDT (52.9%). However, because of the small sample size, the study results are not sufficient to determine that ALA is a better photosensitizer than MAL. A larger study is needed to compare the efficacy of ALA- and MAL-PDT with ablative CO2 fractional laser in the future. Before treatment, we removed the stratum corneum in hyperkeratotic AK lesions to reduce the bias between hyperkeratotic and non-hyperkeratotic lesions. Although there were only a few hyperkeratotic AKs in our study, this procedure might have had an impact on the results. Because AFR can induce sufficient penetration of the photosensitizer in thick lesions, a further study of AFR with PDT in hyperkeratotic AKs without removing the stratum corneum is required.
The limitations of this study include the small sample size and the fixed conditions and the setting of the ablative fractional CO2 laser and PDT treatment (incubation time of photosensitizer, light source and exposure time). Although we tried to match the incubation time to the ratio of the recommended regimen, sequential assessment to determine the optimal incubation time and treatment protocol of ablative CO2 fractional laser should be investigated in the future. In addition, because ablative laser therapy itself is one of the effective treatments for AKs, it is necessary to compare PDT after fractional ablative laser and repeated fractional ablative laser. Although PDT after ablative CO2 fractional laser could decrease the incubation time, we did not enrol a control group without fractional CO2 laser during the study period. Double-blind randomized trials or large controlled studies will be necessary to confirm the results of this study.
In conclusion, PDT after ablative CO2 fractional laser application with a short photosensitizer incubation time provided a relatively good response, with no side effects, in the treatment of AK. Therefore, ablative CO2 fractional laser application may be considered as an additional treatment option for reducing the incubation time of the photosensitizer in PDT. This treatment regimen may offer practical advantages in routine practice.
Figures and Tables
Fig. 1
Patient 8. Fluorescence assessment. Before red light illumination, the fluorescence of the lesion applied with photosensitizer was evaluated with an ultraviolet light emitting device. (A) Before photosensitizer application. (B) After photosensitizer application. Arrowhead: lesion.
Fig. 2
Scheme of efficacy evaluation. PDT: photodynamic therapy, CR: complete response, PR: partial response, NR: no response.

Fig. 3
(A, B) Patient 2. (C, D) Patient 13. Clinical clearance of the actinic keratosis lesion after treatment with the combination of ablative CO2 fractional laser pretreatment and photodynamic therapy. (A, C) Before treatment. (B, D) After treatment. Arrowhead: lesion.

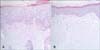
Fig. 4
Patient 13. Histological clearance of the actinic keratosis lesion after treatment with the combination of ablative CO2 fractional laser application and photodynamic therapy (H&E, ×200). (A) Before treatment. (B) After treatment.
ACKNOWLEDGMENT
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRK), funded by grant 2010-0022412 from the Ministry of Education, Science, and Technology (Dr Kim).
References
1. Ericson MB, Wennberg AM, Larkö O. Review of photodynamic therapy in actinic keratosis and basal cell carcinoma. Ther Clin Risk Manag. 2008; 4:1–9.
2. Martin G. The impact of the current United States guidelines on the management of actinic keratosis: is it time for an update? J Clin Aesthet Dermatol. 2010; 3:20–25.
3. Klein A, Babilas P, Karrer S, Landthaler M, Szeimies RM. Photodynamic therapy in dermatology--an update 2008. J Dtsch Dermatol Ges. 2008; 6:839–845.
4. Szeimies RM, Karrer S, Radakovic-Fijan S, Tanew A, Calzavara-Pinton PG, Zane C, et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: a prospective, randomized study. J Am Acad Dermatol. 2002; 47:258–262.

5. MacCormack MA. Photodynamic therapy in dermatology: an update on applications and outcomes. Semin Cutan Med Surg. 2008; 27:52–62.

7. Haedersdal M, Sakamoto FH, Farinelli WA, Doukas AG, Tam J, Anderson RR. Fractional CO(2) laser-assisted drug delivery. Lasers Surg Med. 2010; 42:113–122.

8. Ortiz-Policarpio B, Lui H. Methyl aminolevulinate-PDT for actinic keratoses and superficial nonmelanoma skin cancers. Skin Therapy Lett. 2009; 14:1–3.
9. Smucler R, Vlk M. Combination of Er:YAG laser and photodynamic therapy in the treatment of nodular basal cell carcinoma. Lasers Surg Med. 2008; 40:153–158.

10. Fang YP, Wu PC, Tsai YH, Huang YB. Physicochemical and safety evaluation of 5-aminolevulinic acid in novel liposomes as carrier for skin delivery. J Liposome Res. 2008; 18:31–45.

11. Fang JY, Lee WR, Shen SC, Fang YP, Hu CH. Enhancement of topical 5-aminolaevulinic acid delivery by erbium:YAG laser and microdermabrasion: a comparison with iontophoresis and electroporation. Br J Dermatol. 2004; 151:132–140.

12. de Leeuw J, van der Beek N, Bjerring P, Neumann HA. Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid 0.5% liposomal spray and intense pulsed light in combination with topical keratolytic agents. J Eur Acad Dermatol Venereol. 2010; 24:460–469.

13. Clementoni MT, B-Roscher M, Munavalli GS. Photodynamic photorejuvenation of the face with a combination of microneedling, red light, and broadband pulsed light. Lasers Surg Med. 2010; 42:150–159.

14. Fukui T, Watanabe D, Tamada Y, Matsumoto Y. Photodynamic therapy following carbon dioxide laser enhances efficacy in the treatment of extramammary Paget's disease. Acta Derm Venereol. 2009; 89:150–154.
15. Bogdan Allemann I, Kaufman J. Fractional photothermolysis-an update. Lasers Med Sci. 2010; 25:137–144.

16. Yoo KH, Kim BJ, Kim MN. Enhanced efficacy of photodynamic therapy with methyl 5-aminolevulinic acid in recalcitrant periungual warts after ablative carbon dioxide fractional laser: a pilot study. Dermatol Surg. 2009; 35:1927–1932.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download