Dear Editor:
Molluscum contagiosum (MC) is a common benign skin disease caused by the pox virus and usually affects young children. Most MC in adults occurs in people with an immunosuppressive status, but it can also appear in immunocompetent adults who have experienced friction or scrubbing. We herein report a case of MC that presents multiple pinhead-sized eruptive skin-coloured papules covering the whole face and neck in a patient without a history of epidermal trauma.
A 60-year-old Korean woman with a history of recent onset diabetes presented to our clinic with sudden eruptive papules on her face and neck, which had been persistent for the past 6 months. She had been treated with topical hydrocortisone in the local clinic, but no improvements were observed. Even though she was mostly asymptomatic, the patient complained of occasional mild pruritus. She had no history of towel scrubbing or massage. Upon physical examination, multiple 2 to 3-mm-sized skin-coloured papules were observed on her face and neck (Fig. 1).
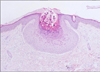
Keratin-like material was observed after extractions of some lesions, resulting in the performance of punch biopsy under the initial impression of milium. Histopathologic examination revealed epidermal cells bearing large eosinophilic cytoplasmic inclusion bodies, typical of the molluscum body, and the lesion was diagnosed as MC (Fig. 2). Due to diffuse distributions across the face and neck, imiquimod cream, oral gamma linolenic acid 360 mg and oral cimetidine 2,000 mg were used daily for 3 months, until all the lesions were resolved. We believe that the immunomodulating effects from imiquimod cream and oral cimetidine could have contributed to the resolution.
There have been several reports of disseminated molluscum contagiosum in patients with hematologic malignancies, human immunodeficiency (HIV) infection, or in patients taking immunosuppresants such as methotrexate or azathioprine1,2. Cases associated with traumas and contacts have also been reported, such as molluscum folliculitis after shaving or molluscum developed after use of a nylon towel at a public spa3,4.
In this case, the patient was a healthy woman without any evidence of systemic diseases other than diabetes and was not taking any medicine that could impair cellular immunity. Lab data including complete blood counts and routine chemistry were within normal values and venereal disease research laboratory (VDRL) was non-reactive. Anti-HIV antibodies were also negative. In addition, she had no history of shaving, friction or massage, which might cause the inoculation of pox virus from epidermal trauma. However, an incidental MC infection could have spread to her whole face and neck due to the application of hydrocortisone cream after a misdiagnosis.
In conclusion, our case suggests that dermatologists should perceive various clinical features of MCs in order to avoid misdiagnosis due to unusual clinical features. Additionally, the diagnosis of mollosum contagiosum should not be excluded, even if the patient is a healthy person without immunodeficiency.
Figures and Tables
References
1. Madan V, August PJ. Facial molluscum contagiosum in a patient with rheumatoid arthritis taking methotrexate. Clin Exp Dermatol. 2008; 33:347.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download