Abstract
Background
Ceramides are the main lipid component of the stratum corneum and are a structurally heterogeneous and complex group of sphingolipids of which sphingoid bases are the basic structural constituents. Altered levels of sphingoid bases have been reported in skin conditions that involve dryness and barrier disruption, including atopic dermatitis.
Objective
The purpose of this study was to investigate the altered levels of sphingoid bases in psoriatic epidermis and their relationship with the clinical severity of the psoriasis.
Methods
Samples from the lesional and non-lesional epidermis were obtained from eight psoriasis patients. Levels of sphingosine and sphinganine were analyzed by high-performance liquid chromatography. The expression of ceramide synthase and ceramidase proteins, which are related to sphingosine and sphinganine metabolism, were measured using Western blot analysis.
Results
Levels of sphingosine and sphinganine in the lesional epidermis were significantly higher than those in the non-lesional epidermis. Although there was no altered ceramide synthase and ceramidase, there was a highly significant positive correlation between the % change of ceramidase, the degradative enzyme of ceramide into sphingosine, and the Psoriasis Area Severity Index (PASI) score.
Ceramides are the primary lipids in the stratum corneum1 and their depletion is thought to be one of the etiological factors of barrier disruption in various skin conditions. Marked depletion of ceramides in the stratum corneum has been reported in such conditions, particularly in patients with psoriasis and atopic dermatitis (AD)2-4. In our previous study, we found that the decreased levels of ceramide in psoriatic skin lesions caused epidermal hyperplasia via downregulation of apoptotic signal cascades such as protein kinase C-alpha (PKC-α) and c-jun N-terminal kinase (JNK)5,6.
In the de novo synthesis of ceramide, sphinganine (Sa) is generated by enzymatic condensation of serine and phalmitoyl-Co A by serine palmitoyltransferase, and Sa is further acylated into ceramides. The newly synthesized ceramide is promptly metabolized to glucosylceramide or sphingomyelin and is ultimately degraded into sphingosine (So) and fatty acids by cermidase. Ceramides are a structurally heterogeneous and complex group of sphingolipids, of which sphingoid bases are basic structural constituents7-9. So and Sa exhibit anti-microbial activity and prevent the adherence of bacteria to cells10,11, but their functions remain otherwise largely unknown. Changes in the levels of sphingoid bases have been described in skin conditions involving dryness and barrier disruption, including AD.12,13 However, only limited information is available on alterations in sphingoid bases in psoriasis. Therefore, the aim of this study was to examine the levels of sphingoid bases in the epidermis of psoriasis patients and to assesses their relationship with psoriasis severity.
Eight Korean patients with psoriasis (two women, six men) ranging in age from 21 to 58 years gave informed consent and participated in this study. All subjects had psoriasis vulgaris as identified through clinical and histologic assessment and had not been treated either systemically or topically for at least one month before punch biopsies were obtained. Using a 4-mm punch, biopsies were taken from lesional and non-lesional skin on the lower extremities, back, or arms. The epidermis was separated as described previously14. Specifically, the epidermis was separated from whole-skin biopsies by overnight incubation at 4℃ in a 1:1 (v/v) mixture of Dispase solution (Roche Molecular Biochemicals, Manheim, Germany) and Hank's balanced salt solution (HBSS; Gibco BRL, Life Technologies, Rockville, MD, USA).
The clinical severity was assessed using the Psoriasis Area Severity Index (PASI) score, which is calculated as follows: PASI=0.1 (Eh+Ih+Dh) Ah+0.2 (Eu+Iu+Du) Au+0.3 (Et+It+Dt) At+0.4 (El+Il+Dl) Al, where E=erythema, I=infiltration, D=desquamation, A=area, h=head, u=upper extremities, t=trunk, and l=lower extremities. A numerical value is given to the extent of the lesions in each area as follows: 1≤10%, 2=10~30%, 3=30~50%, 4=50~70%, 5=70~90%, and 6=90~100%. E, I, and D are scored on a five-point scale (0=no symptoms, 1=slight, 2=moderate, 3=marked, and 4=very marked) to obtain a final PASI score between 0 and 72. The PASI scores of the patients who took part in this study ranged between 1.8 and 23.7; this range corresponds to mild and moderate psoriasis. Only patients with PASI scores <25 were enrolled in this study in order to determine whether alterations in the levels of ceramides and ceramide-related apoptotic signaling molecules are closely correlated to the clinical severity of mild to moderate psoriasis.
Epidermal tissue isolated from each 4 mm punch biopsy was homogenized with a Polytron homogenizer in 500 µl of ice-cold phosphate-buffered saline. After centrifugation at 240×g for 5 min, aliquots (50 µl of supernatant) of the epidermal homogenates were collected for protein determination by a modified Lowry method using bovine serum albumin as the standard15. Sphingoid bases were extracted by adding 350 µl of MeOH, 150 µl of 1 M NaCl and 300 µl of CHCl3 to the prepared homogenates. A 35 µg aliquot of 3N NaOH was also added to adjust the pH to 10~11 in order to facilitate the separation of sphingoid bases in the upper phase. As an internal standard, 100 pmol of the non-naturally occurring species15,16 C17 So and C17 S1P was added followed by vigorous vortexing for 1 h. After centrifugation at 240×g for 3 min, the lower phase was evaporated under N2 gas and then dissolved in 500 µl of 0.15 M methanolic KOH with vortexing for 20 min at 37℃. Then, 500 µl of CHCl3, 100 µl of 2 N-NH4OH and 400 µl of alkaline water were added and the mixture was vortexed for an additional hour. After centrifugation at 240×g for 3 min, the lower phase was washed twice with 800 µl of alkaline water and the CHCl3 was evaporated using a SpeedVac concentrator16.
The extracted lipid fraction was resolved in 120 µl of MeOH. A 20 µl volume of o-phthalaldehyde (OPA) derivatization reagent (Sigma, St. Louis, MO, USA; 50 mg ortho-phthal-dialdehyde, 1 ml ethanol, 100 µl 2-mercaptoethanol, and 50 ml 3% (w/v) boric acid solution) was added and the mixture was allowed to stand for 30 min at room temperature17,18. OPA reacts with the primary amine group of the sphingoid bases and becomes highly fluorescent at an excitation wavelength of 340 nm and an emission wavelength of 455 nm17,18. The derivatives were analyzed using a Jasco (Tokyo, Japan) PU-980 pump, an AS-1559 autosampler, and a Jasco FP-920 fluorescence detector. The isocratic eluent comprised of methanol: deionized distilled water (92:8 v/v) with 0.1% triethylamine was flowed at the rate of 1 ml/min. A 70 µl aliquot of the derivatives was injected then separated on an C18 column (Waters, Sunfire 4.6×1.5 mm internal diameter) kept at room temperature, and the fluorescence was measured at an emission wavelength of 455 nm and an excitation wavelength of 340 nm17. C17 So (8.5 min), C18 So (10.5 min), C18 Sa (14.2 min) were detected.
Isolated epidermis was added to 200 µl of Folch solution (CHCl3:MeOH, 2:1, v/v mixture) and homogenized using a Polytron homogenizer, and 200 µl of 0.1 M KCl was subsequently added. The mixture was centrifuged at 2,000 rpm for 5 min, and the upper phase containing the extracted proteins was separated. This process was repeated a total of two times. The protein concentration was determined by BCA protein assay (Pierce, Rockford, MD, USA) according to the manufacturer's protocol. Fifty micrograms of protein was fractionated via 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to a nitrocellulose membrane. The membranes were blocked with 5% non-fat dry milk for 1 h at room temperature and incubated with antibodies against ceramide synthase (CerS) and ceramidase (CDase) (Labfrontier, Seoul, Korea) at a 1:250 dilution with Tris-buffered saline containing 0.05% Tween-20 (TSB-T) at 4℃ overnight. After washing with TBS-T for 1 h, the membranes were reacted with horseradish peroxidase-conjugated anti-rabbit IgG antibody (Amersham Biosciences, Buckinghamshire, UK) that had been diluted 1:250 with TBS-T, for 1 h at room temperature. After washing the membranes with TBS-T for 2 h, protein expression was detected using an ECL chemiluminescence kit (Amersham Bioscience).
A paired t-test was used to compare the levels of So and Sa between the lesional and non-lesional samples collected from psoriasis patients. The relationship between the CDase levels and PASI scores was assessed using Pearson's correlation analysis. p<0.05 were considered statistically significant.
The high-performance liquid chromatography analysis results of C18 So and C18 Sa in the lesional and non-lesional epidermis samples from psoriasis patients are shown in Fig. 1. The level of So in the lesional epidermis was significantly higher (23.5±10.9; range, 14.66~32.34 nmol/µg protein) than that in the non-lesional epidermis (10.9±4.08; range, 6.82~14.98 nmol/µg protein) (p<0.05). Likewise, the level of Sa in the lesional epidermis was significantly higher (11.4±4.20; range, 7.2~15.6 nmol/µg protein) than that in the non-lesional epidermis (1.3±0.70; range, 0.6~2.06 nmol/µg protein) (p<0.05). The mean % of lesional So to non-lesional So and that of Sa were 215% and 857%, respectively.
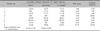
The CDase and CerS expression levels in the lesional and non-lesional epidermis of psoriasis patients, PASI scores, and disease durations are listed in Table 1 and 2. The absolute level of CDase and CerS varied from patient to patient. The protein expression of CDase and CerS in the lesional epidermis was not altered compared to that in the non-lesional epidermis. A highly significant positive correlation was observed between the % change in CDase and the PASI score (r=0.752, p<0.05), as shown in Fig. 2, but there was no correlation between the % change in CerS and the PASI score. These results indicate that an increase of CDase is significantly correlated with the PASI score in mild to severe psoriasis, suggesting that increased levels of So are likely caused by the increased expression of CDase.
The fundamental function of the epidermis is to serve as an efficient barrier against water loss through the skin1. The epidermal barrier is comprised of the extracellular lipid-enriched membranes of the stratum corneum and is organized into membranous multi-layers with a repetitive lamellar structure. The intercellular lipid lamellae are composed predominantly of ceramides, cholesterol, and fatty acids that originate from polar lipid precursors provided by cells in the basal layer of the epidermis19,20.
Ceramides are the primary lipids in the stratum corneum. During keratinization, almost all of the epidermal phospholipids found abundantly in the basal layer disappear and ceramides, which are synthesized de novo from phospholipid intermediates, remain within the stratum corneum21. Ceramide-rich intercellular lipid lamellae are thought to be of particular importance in maintaining the structural integrity of the epidermal barrier22,23. Depletion of ceramides in the stratum corneum has been suggested as an etiological factor of dryness and barrier disruption in skin conditions such as AD and essential fatty acid deficiency2-4. Ceramides are a structurally heterogeneous and complex group of sphingolipids containing derivatives of So bases joined by an amide linkage to a variety of fatty acids. Differences in chain length, type and the extent of hydroxylation and saturation are responsible for the heterogeneity of epidermal sphingolipids24.
Sphingoid (long-chain) bases are the basic structural constituents of sphingolipids, which are thought to be synthesized by the acylation of sphingoid bases to form a ceramide, with subsequent glycosylation and other modifications leading to the formation of complex sphingolipids such as neutral glycosylsphingolipids, and phosphosphingolipids (e.g., sphingomyelin)25. So and Sa, which are free sphingolipids of the stratum corneum, have been shown to strongly inhibit both bacteria and fungi in vitro10. Furthermore, So was found to be significantly downregulated in the skin of patients with AD compared with healthy controls12. Alterations in the ratio of So to Sa due to a ceramide metabolic abnormality in the stratum corneum can affect membrane integrity in AD13. Additionally, as lipid second messengers, they mediate antiproliferative and apoptotic effects via activation of several signal transduction molecules such as PKC-α and JNK5-7. However, there are only a few studies that have examined the relationship between sphingoid bases and psoriasis.
In this study, we measured the levels of the precursor and degradation products of two ceramides, Sa and So, in both psoriatic and non-lesional skin. The levels of both proteins were significantly higher in psoriatic skin compared to in the non-lesional epidermis, indicating that in psoriatic skin, ceramide synthesis is decreased and the degradation of these proteins is increased. These results suggest that ceramide levels, which are regulated by a balance in the activity of ceramide generating enzymes such as CerS in the de novo synthesis pathway and degradative enzymes such as CDase, are not well-controlled in the epidermis of psoriasis patients.
We measured the expression of CerS and CDase in both the psoriatic epidermis and non-lesional epidermis. CerS is one of the enzymes related to the synthesis of ceramide, and CDase is a catalytic enzyme that is related to a decrease in ceramide levels. The results of this experiment showed that the levels of CerS were decreased in psoriatic skin, whereas the levels of CDase were increased. However, there was no significant difference in the levels of CerS and CDase between psoriatic epidermis and non-lesional epidermis. We also evaluated the relationship between the PASI score and increased levels of CDase to determine the relationship between CDase and psoriasis severity. The percent change in the ratio of lesional/non-lesional epidermis and the PASI score showed a significant and direct correlation. These findings confirm those of our previous study26, namely that decreased levels of ceramide in psoriatic skin are responsible for increased levels of CDase in psoriatic skin lesions and that, furthermore, increased levels of this protein are highly correlated with the clinical severity of psoriasis. These results are also consistent with those found in a previous study of CDase activity in AD11.
However, there are some limitations to our study. First, we could not show the relation between psoriasis patients and healthy volunteers. Of course, it is well known that the ceramide level of healthy skin is decreased compared with that of psoriasis and AD patients, based on the results of previous study. However, earlier studies have not directly compared between healthy volunteers and psoriasis patients in terms of the levels of Sa and So. In addition, our study also had a relatively small sample size. Therefore, further studies should include more patients, as well as comparison with healthy volunteers.
In conclusion, we demonstrated that So and Sa levels are significantly increased in psoriatic epidermis and that increased expression of CDase is positively correlated with the clinical severity of psoriasis. Given that psoriasis is an inflammatory skin disease, several cytokines or growth factors secreted by keratinocytes, Langerhans cells, or T-cells in psoriatic skin lesions may affect the regulation of ceramide synthesis and expression of CDase. However, in light of the study limitations as given above, further study is required to confirm this hypothesis.
Figures and Tables
Fig. 1
(A, B) Sphingoid bases in lesional and non-lesional skin. Values are presented as mean±standard error of measurement. *p<0.05 by paired t-test.

Fig. 2
Correlation between % change in ceramidase protein expression and the Psoriasis Area Severity Index (PASI) score (r=0.752, p<0.05).

References
1. Elias PM, Menon G. Structural and lipid biochemical correlates of the epidermal permeability barrier. In : Elias PM, editor. Skin lipid. Advances in lipid research. San Diego: Academic Press;1999. p. 24–26.
2. Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin? J Invest Dermatol. 1991; 96:523–526.

3. Matsumoto M, Umemoto N, Sugiura H, Uehara M. Difference in ceramide composition between "dry" and "normal" skin in patients with atopic dermatitis. Acta Derm Venereol. 1999; 79:246–247.

4. Chung S, Kong S, Seong K, Cho Y. Gamma-linolenic acid in borage oil reverses epidermal hyperproliferation in guinea pigs. J Nutr. 2002; 132:3090–3097.

5. Cho Y, Lew BL, Seong K, Kim NI. An inverse relationship between ceramide synthesis and clinical severity in patients with psoriasis. J Korean Med Sci. 2004; 19:859–863.

6. Lew BL, Cho Y, Kim J, Sim WY, Kim NI. Ceramides and cell signaling molecules in psoriatic epidermis: reduced levels of ceramides, PKC-alpha, and JNK. J Korean Med Sci. 2006; 21:95–99.

7. Aschrafi A, Franzen R, Shabahang S, Fabbro D, Pfeilschifter J, Huwiler A. Ceramide induces translocation of protein kinase C-alpha to the Golgi compartment of human embryonic kidney cells by interacting with the C2 domain. Biochim Biophys Acta. 2003; 1634:30–39.

8. Huwiler A, Fabbro D, Pfeilschifter J. Selective ceramide binding to protein kinase C-alpha and -delta isoenzymes in renal mesangial cells. Biochemistry. 1998; 37:14556–14562.

9. Ruvolo PP. Ceramide regulates cellular homeostasis via diverse stress signaling pathways. Leukemia. 2001; 15:1153–1160.

10. Bibel DJ, Aly R, Shinefield HR. Topical sphingolipids in antisepsis and antifungal therapy. Clin Exp Dermatol. 1995; 20:395–400.

11. Ohnishi Y, Okino N, Ito M, Imayama S. Ceramidase activity in bacterial skin flora as a possible cause of ceramide deficiency in atopic dermatitis. Clin Diagn Lab Immunol. 1999; 6:101–104.

12. Arikawa J, Ishibashi M, Kawashima M, Takagi Y, Ichikawa Y, Imokawa G. Decreased levels of sphingosine, a natural antimicrobial agent, may be associated with vulnerability of the stratum corneum from patients with atopic dermatitis to colonization by Staphylococcus aureus. J Invest Dermatol. 2002; 119:433–439.

13. Aburai K, Yoshino S, Sakai K, Sakai H, Abe M, Loiseau N, et al. Physicochemical analysis of liposome membranes consisting of model lipids in the stratum corneum. J Oleo Sci. 2011; 60:197–202.

14. Macheleidt O, Kaiser HW, Sandhoff K. Deficiency of epidermal protein-bound omega-hydroxyceramides in atopic dermatitis. J Invest Dermatol. 2002; 119:166–173.

15. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951; 193:265–275.

16. Ruwisch L, Schäfer-Korting M, Kleuser B. An improved high-performance liquid chromatographic method for the determination of sphingosine-1-phosphate in complex biological materials. Naunyn Schmiedebergs Arch Pharmacol. 2001; 363:358–363.

17. Min JK, Yoo HS, Lee EY, Lee WJ, Lee YM. Simultaneous quantitative analysis of sphingoid base 1-phosphates in biological samples by o-phthalaldehyde precolumn derivatization after dephosphorylation with alkaline phosphatase. Anal Biochem. 2002; 303:167–175.

18. Yoon HT, Yoo HS, Shin BK, Lee WJ, Kim HM, Hong SP, et al. Improved fluorescent determination method of cellular sphingoid bases in high-performance liquid chromatography. Arch Pharm Res. 1999; 22:294–299.

19. Rogers J, Harding C, Mayo A, Banks J, Rawlings A. Stratum corneum lipids: the effect of ageing and the seasons. Arch Dermatol Res. 1996; 288:765–770.

20. Gray GM, White RJ, Williams RH, Yardley HJ. Lipid composition of the superficial stratum corneum cells of pig epidermis. Br J Dermatol. 1982; 106:59–63.

21. Hedberg CL, Wertz PW, Downing DT. The time course of lipid biosynthesis in pig epidermis. J Invest Dermatol. 1988; 91:169–174.

22. Grubauer G, Feingold KR, Harris RM, Elias PM. Lipid content and lipid type as determinants of the epidermal permeability barrier. J Lipid Res. 1989; 30:89–96.

23. Wertz PW, Cho ES, Downing DT. Effect of essential fatty acid deficiency on the epidermal sphingolipids of the rat. Biochim Biophys Acta. 1983; 753:350–355.

24. Coderch L, López O, de la Maza A, Parra JL. Ceramides and skin function. Am J Clin Dermatol. 2003; 4:107–129.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download