Dear Editor:
Epoprostenol is a synthetic prostacycline that remains the first line treatment for patients with severe pulmonary hypertension (PH)1-3. Herein, we present a case of severe erythroderma associated with the initiation of therapy with intravenous epoprostenol.
A 50-year-old woman with PH secondary to CREST syndrome (Calcinosis, Raynaud, Esophageal dysmotility, Sclerodactyly, Telangiectasia), gastroesophageal reflux disease, and chronic obstructive pulmonary disease treated with acenocoumarol, furosemide, spironolactone, tiotropium inhaled, budesonide/formoterol inhaled, azathioprine, omeprazole and oxygen for the 5 years prior presented to our clinic.
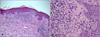
Because of the severity of her symptoms secondary to PH, 12 ng/kg/min IV epoprostenol was prescribed for treatment. During the first month, the patient's dyspnea improved and a discrete asymptomatic erythema appeared. One month later, we increased the patient's epoprostenol dose to 14 ng/kg/min. After 2 weeks, the patient developed a progressive maculopapular exanthema, chills, and intense pruritus, rapidly evolving to erythroderma with large areas of exfoliation (Fig. 1). The patient had no mucosal lesions, systemic symptoms, or fever. Haemograma and biochemical determinations were normal. Histopathologic examination of the skin was consistent with a true drug reaction, excluding just vasodilatation (Fig. 2). Epoprostenol was believed to be the most likely cause as it was the most recently added drug. Due to the severity of respiratory symptoms, epoprostenol was maintained and oral prednisone was initiated at 16 mg/24 h together with methylprednisolone 0.1% ointment.
One month later, the patient continued with diffuse erythema and intense pruritus, so epoprostenol was tapered to 12 ng/kg/min. One week later the patient's erythema improved, but her dyspnea increased, so epoprostenol was again increased to 14 ng/kg/min. The patient remained hemodynamically stable and her clinical cutaneous reaction slowly improved. Oral prednisone was tapered and epoprostenol was increased to 16 ng/kg/min. Two years later, the patient was tolerating epoprostenol with complete resolution of the erythroderma, without any change in her usual medication.
Dose-limiting side effects of epoprostenol are related to prostenoid vasoactivity, such as flushing, jaw pain, arthralgia, myalgia, nausea, hypotension, and headache1,3,4.
Patients receiving chronic epoprostenol therapy often develop slight erythema without other systemic symptoms4,5. Myers et al.4 reported cutaneous findings in patients receiving long-term epoprostenol therapy, including diffuse erythema with lower extremity accentuation, palpable purpura, brawny pretibial discoloration with edema, and one case of diffuse erythroderma and exfoliation4,5. In this case, they described a woman with PH secondary to connective tissue disease and who developed severe erythroderma that improved after discontinuation from drug treatment. Our patient had been following a stable medical regimen prior to receiving the new drug and she did not improve until the dose of epoprostenol was tapered; however, the drug was not discontinued. Our patient developed an erythroderma with at the dose of 14 ng/kg/min, slightly higher than a case published previously (11.5 ng/kg/min)4,5. The altered immune function associated with connective disease might increase the risk of drug-induced reaction5 independentof drug dose.
Our patient clinical course indicates that it may not be necessary to stop epoprostenol therapy for resolution of severe toxicoderma. Inmunomodulatory effects of epoprostenol therapy are poorly understood at present. As far as we know, this is the second case published on severe toxic erythroderma caused by epoprostenol.
Figures and Tables
References
1. Barst RJ, Rubin LJ, Long WA, McGoon MD, Rich S, Badesch DB, et al. Primary Pulmonary Hypertension Study Group. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med. 1996. 334:296–301.

2. Badesch DB, Tapson VF, McGoon MD, Brundage BH, Rubin LJ, Wigley FM, et al. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of disease. A randomized, controlled trial. Ann Intern Med. 2000. 132:425–434.

3. McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002. 106:1477–1482.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download