Dear Editor:
Venous aneurysm (VA) is defined as a solitary area of venous dilatation, not associated with an arteriovenous communication or a pseudoaneurysm1, and appears to be often misdiagnosed as a subcutaneous tumor. Here, we describe the case of VA in a patient's right great saphenous vein, which was difficult to diagnose due to complete thrombosis.
An 82-year-old Japanese man presented to our hospital with a 20-year history of an asymptomatic mass on his right inner thigh. Physical examination showed a, non-compressible, slightly relocatable, non-tender, subcutaneous mass 5 cm in diameter (Fig. 1A). The patient had a history of acute myocardial infarction five years earlier, and there was no history of catheterization from the site. The patient had been well controlled with an anticoagulant Clopidogrel. Ultrasound examination revealed a heterogeneous, predominantly hypoechoic mass and a color flow duplex scan showed slight blood flow in the peripheral area of the mass. There were no connecting afferent or efferent veins. Also, there was no deep vein thrombosis. Contrast-enhanced computed tomography (CT) demonstrated a cystic structure whose wall was enhanced. We diagnosed the mass as a subcutaneous cystic tumor such as epidermal cyst, because the mass had a cystic wall and no blood flow in the lumen. After withdrawal of Clopidogrel without heparinization for one week, local excision was performed.
Surgical exploration presented a dark bluish fusiform mass connected with an afferent and efferent segment of the great saphenous vein (Fig. 1B). Histological examination revealed a round luminal appearance with abluminal concentric muscular layers and organizing thrombus in the lumen (Fig. 1C). The elastica van Gieson stain revealed that elastic fibers were regularly distributed between the bundles of smooth muscle layers and elastic fibers in the intima were developed (Fig. 1D). A thrombosed VA of the great saphenous vein was diagnosed from all these findings. Six months after the surgery, the patient was symptom-free without any evidence of new lesions.
VA can be defined as a persistent isolated dilation of two to three times the normal diameter. VA occurs throughout the body, involving thoracic, visceral, neck, and extremity venous systems2. VA develops equally between the sexes or with a slight female predominance, and is seen at any age. Usually, a definable cause is not present, although trauma, infection, inflammation, congenital vein wall weakness and degenerative change have been proposed. VA in the deep venous system seems to have a greater association with severe thromboembolism such as pulmonary embolism than the superficial system including the great saphenous vein2. Our case was a VA in the superficial system, with no probability of silent pulmonary embolism, and no symptom of pulmonary embolism such as acute shortness of breath had been observed. Five cases of complete thrombosed VA have been reported in English literatures (Table 1)1-5. Our case is the first case which occurred in a great saphenous vein. Of these six cases, only one case was diagnosed precisely by accurate venous ultrasound imaging and CT scanning3, however the other five cases were misdiagnosed as a soft tissue tumor and so on, in spite of various imaging studies1,2,4,5.
Figures and Tables
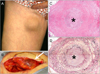 | Fig. 1(A) A non-compressible, poorly mobile, non-tender, subcutaneous mass 5 cm in diameter located on the inside of his right thigh. The overlying skin appeared normal. (B) An intraoperative finding. A dark bluish fusiform mass was revealed (arrow). (C) Histological findings. A round luminal appearance with a concentric muscular layer with organizing thrombus in the lumen was revealed (H&E stain, ×40). The occluded lumen was shown with a star. (D) Elastic fibers were distributed between the bundles of smooth muscle layers and internal elastic lamina-like elastic fibers in the intima were developed (elastica van Gieson stain, ×40). The occluded lumen was shown with a star. |
ACKNOWLEDGMENT
This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, and Health and from the Ministry of Health, Labor and Welfare of Japan.
References
1. De Waele JJ, Calle PA, Vermassen FE. Thrombosis of an aneurysm of the basilic vein upper extremity venous aneurysm. Acta Chir Belg. 2001. 101:308–309.

2. Morrison J, Rubin DA, Tomaino MM. Venous aneurysm of the distal forearm: MR imaging findings. AJR Am J Roentgenol. 1996. 167:1552–1554.

3. Gabrielli R, Rosati MS, Costanzo A, Chiappa R, Siani A, Caselli G. Primary tibial vein aneurysm with recurrent pulmonary emboli. J Vasc Surg. 2010. 52:464–466.

4. Tsolakis JA, Kakkos SK, Panagiotopoulus E. Popliteal venous aneurysm mimicking a soft tissue tumour. A case report. Int Angiol. 1999. 18:74–76.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download