Abstract
Background
Short stature is sometimes seen in children with atopic dermatitis (AD); however, the topic has never been studied systematically. Objective: The aim of this study was to show whether AD itself affects stature in children and to evaluate the influence of other relevant factors such as genetic background, diet restrictions, and sleep disturbance on the stature of children with AD.
Objective
The aim of this study was to show whether AD itself affects stature in children and to evaluate the influence of other relevant factors such as genetic background, diet restrictions, and sleep disturbance on the stature of children with AD.
Methods
The study population included Korean children 7 to 8 years of age who live in one district of Seoul, Korea. We used a questionnaire as an investigating tool to survey genetic backgrounds, environmental factors, and comorbidities. Student's t-test and linear regression were employed for statistical analysis.
Results
In univariate analysis, the average stature in the AD group was short compared with the normal control group. Parental stature, dietary habit, and sleep patterns were also relevant factors with respect to stature. However, in multivariate analysis, AD itself had no influence on stature. Significant correlations were found for such factors as parental height, sleep disturbance, presence of asthma, and dietary restrictions, in decreasing magnitude.
Atopic dermatitis (AD) is a chronic, relapsing, inflammatory skin disease resulting from a complex interaction between genetic and environmental factors1. Several cross-sectional studies have reported impaired growth in children with AD and a higher prevalence of AD among children with short stature compared to those with normal stature2-4. Several hypotheses have been proposed to explain the link between short stature and children with AD. Short stature may be a result of asthma5, which commonly coexists with dermatitis, or be due to the use of topical corticosteroids. It is thought that 'active allergy' may cause growth failure, though published data do not allow one to distinguish between the effects of 'allergy' and those of untreated asthma6. Defective gastrointestinal handling of certain proteins may play a part in the pathogenesis of AD, and partial villous atrophy has been found among an atypical group of children with dermatitis7; therefore, malabsorption may contribute to growth failure8. Inappropriate dietary restrictions, which may be seen in some children with AD, can also impair growth9. Children with severe dermatitis often sleep badly, and this may interfere with growth hormone release. However, a longitudinal growth study found that atopic prepubescent children were not shorter than the normal control (NC) group, but did have decreased stature velocities consistent with constitutional growth delays as they hit puberty. However, this delay may be temporary since a study found adults with childhood onset AD reached normal adult stature despite the childhood disease. Despite the debate over short stature and children with AD, the topic has never been systematically studied, and it is not mentioned in the standard textbook on AD. The aim of this study was to determine whether AD itself affects stature in children, and to evaluate the influence of other relevant factors such as genetic background, diet restrictions, and sleep disturbance on the stature of children with AD.
The present study included Korean elementary school children with AD, from Dongjak-gu and its surrounding region. Parents of the children were asked to complete an anonymous questionnaire on the topic of AD in the clinic. Parents that consented to filling out the questionnaire had their child's standing stature measured on a wall chart and self-reported their own stature. The information obtained from the questionnaires was used to divide a total of 2,372 children (mean age, 8.3 years) recruited for the study into two groups: AD group and NC group (Table 1). Of these, analyses were performed on 517 patients with AD (316 males and 201 females; mean age, 7.18±5.04 years) and 618 NCs (310 males and 308 females; mean age, 7.78±6.64 years). NCs were individuals without AD, allergic asthma, allergic rhinitis, atopic keratoconjunctivitis, or other allergic symptoms reported in the questionnaire. In addition, their total serum immunoglobulin E levels were within the normal range.
The questionnaire consisted of questions regarding AD, diet restrictions, and sleep disturbance (Table 2). If the child had been previously diagnosed with AD, the age of onset was noted. Patients with a known independent cause for short stature, history of long term systemic disease, or endocrine problems during childhood were excluded from the study and control group. In addition, the stature of both parents was recorded, as genetic background may influence a child's stature10.
AD was diagnosed by following the Korean guidelines of the 2005 Atopic Dermatitis Research Group11. Stature was standardized for age and gender using data from the Korea Agency Technology and Standards. In addition, mid-parental stature was calculated for each child to approximate the child's genetic stature potential and was also standardized for sex and age. In regards to diet restrictions, parents were asked if any foods were removed from the child's diet, and if so, what types of food were restricted. For factors related to sleep disturbance, children were asked if they had a hard time falling or staying asleep. The enquiry also included questions on the potential causes of sleep disturbance and how long the child has suffered from the sleep disorder. Independent t-tests were conducted to examine differences in mean stature between the AD and NC groups. Regression analysis was performed to estimate the average value of the dependent variables (between AD and stature), when the independent variables (genetic background, diet restrictions, and sleep disturbance) were fixed.
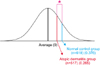
The standard normal distribution was used to compare the average stature of the AD (0.262±1.01 standard deviation [SD]) and NC group (0.362±1.00 SD). Both groups were taller than the average stature for age (Fig. 1); however, there was a difference in the average stature between the AD and NC groups (p<0.05). In other words, the AD group was shorter than the average stature for their age group.
Statistically significant differences in standing stature (standardized according to the Korea Agency Technology and Standards) were observed between patients with diet restrictions and those without restrictions. In addition, correlation analysis demonstrated a substantial negative correlation between stature and diet restrictions. Although the questionnaire was used to obtain information about the types of foods restricted, there were no preferences for specific foods removed from the diet, such as cheese, meat, milk or others.
After standardization of parental stature, a statistically significant relationship between the standardized stature of children and their parents was observed (p<0.001). In other words, the genetic relationship between parents' stature and their children's could explain the observed positive correlation.
In regards to sleep disturbance, a significant negative correlation with stature was observed. Sleep disturbance was defined as having present or past sleep difficulties. Here, a significant association was observed between sleep disturbance and short stature.
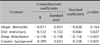
Linear regression was used to analyze the relationship between children's stature and the presence of AD, diet restrictions, sleep disturbance, and parental stature. In other words, this method was used to identify the relationship between the variables influencing stature and the effect of each variable on stature. Linear regression analysis showed that diet restrictions, sleep disturbance, and parental stature had a substantial effect on stature both independently or in concert. Depending on the standardized coefficient, both positive and negative correlations were observed. However, unlike the statistics obtained independently, the presence of AD did not have a substantial effect on stature after controlling for confounding factors. In other words, AD itself does not influence stature more than any of the other factors (Table 3).
AD is a long-lasting skin condition that typically begins in young infants or early childhood. AD will subside spontaneously by adolescence in approximately 90% of patients and can last into adulthood in the remaining 10% of patients12,13. Therefore, the effect of AD on growth impairment is a big concern for parents of children with AD. In addition, the 'active allergy' of AD itself, adverse effects caused by dermatitis treatment with topical steroids or other aggressive treatments, will influence the stature of children with AD14.
According to Thomas et al.15, treatment with topical steroids will improve AD in children. In addition, an ongoing study investigating the use of topical steroids on stature in children with AD found no correlation between the range of potencies of corticosteroids and statures of children, and the groups did not differ in either average stature or average mid-parental stature. Therefore, the general population of AD patients should be able to use topical corticosteroids without fear of significant growth impairment.
In this study, the stature of 7- to 8-year-old children with AD was evaluated. In addition, other factors affecting their stature such as genetic background, diet restrictions, and sleep disturbance were also systematically measured. Of a total of 2,372 children recruited in this study, 517 children with AD were analyzed for the influence of AD on the stature. Results from the analysis of these children demonstrated a negative correlation between stature and the presence of AD. However, in this particular study, we observed that children with AD were taller than the standardized height for age (0.262±1.00 SD). This observation could reflect the nutritional status of children or environmental factors in the district of Dongjak-gu. Considering that the subjects in this study were 6- to 7-year-old students, we found that the difference in stature between the AD and NC groups was 0.42 cm (p<0.05). The finding that children with AD were shorter than children in the NC group could be explained by several measurable factors. First, impairment of growth may be caused by the active allergy of AD itself and the use topical steroids for treatment. In fact, a previous study has shown a statistically significant correlation with comorbidity in asthma and AD and short stature16. In addition, several reports in the literature have suggested that topical steroid treatment interferes with the growth and development of children by inducing HPA axis suppression17-19. However, other studies have also been published that argue against this relationship between topical steroid treatment and impaired growth. In the present study, no conclusions could be drawn in regards to whether these factors contributed to short stature in children with AD; however, this could be due to the limitations of this study. In addition, genetic and environmental factors have been found to be positively correlated with stature, and therefore cannot be eliminated as factors influencing short stature in children with AD.
In addition to AD itself, we also investigated whether other factors associated with this disease such as diet restrictions and sleep disturbance affected the stature of children with AD. We found that children in the AD group with diet restrictions were shorter than the children in the AD group without diet restrictions. However, information on the types of food restricted was not included, a possible limitation of this study. Many parents limited certain food groups (for example, meat and dairy products) in their child's diet that were likely to cause food allergies. More information was needed in regards to the extent to which these specific food types were limited. The impairment of growth due to sleep disturbance has been demonstrated in several thesis papers. Impaired growth factor secretion and tissue acidosis were described as the possible mechanisms for the impaired growth20,21. Results from this study showed that children with sleep disturbance due to nasal congestion and itching were approximately 0.62 cm shorter compared to children with no sleep disturbance; a result that was statistically significant.
We know that each factor affected the stature of children independently. However, we could not overlook the possible associations between the factors and the overall health of children with AD. There are many cases of children with AD who are on diet restrictions and also having itching problems which disturb their sleep. In the present study, we analyzed four different factors by linear regression for the influence on stature: presence of AD, genetic background, diet restrictions, and sleep disturbances.
First, by using linear regression, we were able to analyze how much each of these factors affected stature. In other words, the extent to which each factor influenced height was calculated with standardized coefficients. The linear regression model showed a negative correlation between stature and the three variables: presence of AD, diet restrictions, and sleep disturbance. The standardized coefficient of sleep disturbance had the largest absolute value; therefore, this variable (sleep disturbance) had the biggest impact on stature. In addition, a positive correlation was observed between genetic background and stature.
Second, the effects of overall health on stature were shown to be statistically significant after controlling for each confounding factor. However, unlike the other factors, the presence of AD did not have a statistically significant effect on stature after controlling for the other confounding factors. In other words, AD itself did not significantly affect a child's stature. Since AD itself was not the cause of short stature in children with AD, other factors related to AD such as diet restrictions or sleep disturbance may have a more serious impact on the stature of children with AD. As such, these factors need to be considered in the management of AD. In regards to sleep disturbance, the parents of children with AD should be educated on the management of itching problems with medications such as antihistamines and limiting certain food types based on food allergy tests.
The present study had several limitations. First, the diagnosis of AD in patients was based on a questionnaire that addressed the medical history, not a physical examination by a doctor. Second, the questionnaire required patients and parents to recall their medical history, and therefore may be biased depending on their memory. Finally, as mentioned before, a more in-depth statistical analysis was not possible since this study involved qualitative interpretations such as the presence of sleep disturbance and diet restrictions.
Considering the results of the present study, the appropriate treatment for relief of symptoms in patients with AD is important. Additional research with more AD patients will be needed to better understand the effects of AD and other relevant factors on growth and to improve treatment outcomes.
Figures and Tables
Fig. 1
Stature differences between normal control and atopic dermatitis groups: standard normal distribution (*p<0.05).
ACKNOWLEDGMENT
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A091121).
References
1. Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol. 1994. 30:35–39.

2. Rajka G. Natural history and clinical manifestations of atopic dermatitis. Clin Rev Allergy. 1986. 4:3–26.

3. Pike MG, Chang CL, Atherton DJ, Carpenter RG, Preece MA. Growth in atopic eczema: a controlled study by questionnaire. Arch Dis Child. 1989. 64:1566–1569.

4. Patel L, Clayton PE, Jenney ME, Ferguson JE, David TJ. Adult height in patients with childhood onset atopic dermatitis. Arch Dis Child. 1997. 76:505–508.

5. Ferguson AC, Murray AB, Tze WJ. Short stature and delayed skeletal maturation in children with allergic disease. J Allergy Clin Immunol. 1982. 69:461–466.

6. Cohen MB, Abram LE. Growth patterns of allergic children; a statistical study using the grid technique. J Allergy. 1948. 19:165–171.
7. Ukabam SO, Mann RJ, Cooper BT. Small intestinal permeability to sugars in patients with atopic eczema. Br J Dermatol. 1984. 110:649–652.

8. Sloper KS, Brook CG, Kingston D, Pearson JR, Shiner M. Eczema and atopy in early childhood: low IgA plasma cell counts in the jejunal mucosa. Arch Dis Child. 1981. 56:939–942.

9. Tarnow-Mordi WO, Moss C, Ross K. Failure to thrive owing to inappropriate diet free of gluten and cows' milk. Br Med J (Clin Res Ed). 1984. 289:1113–1114.

10. Tanner JM, Goldstein H, Whitehouse RH. Standards for children's height at ages 2-9 years allowing for heights of parents. Arch Dis Child. 1970. 45:755–762.

11. Park YL, Kim HD, Kim KH, Kim MN, Kim JW, Ro YS, et al. Report from ADRG: a study on the diagnostic criteria of Korean atopic dermatitis. Korean J Dermatol. 2006. 44:659–663.
12. Leung DYM, Rhodes AR, Geka RS. Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IM, Austen KF, editors. Atopic dermatitis. Dermatology in general medicine. 1993. 4th ed. New York: McGraw-Hill Book;1543–1564.
13. Ashtoon R, Leppard B. Differential diagnosis in dermatology. 1992. 2nd ed. Oxford: Radcliffe medical press;103–105.
14. Kristmundsdottir F, David TJ. Growth impairment in children with atopic eczema. J R Soc Med. 1987. 80:9–12.

15. Thomas MW, Panter AT, Morrell DS. Corticosteroids' effect on the height of atopic dermatitis patients: a controlled questionnaire study. Pediatr Dermatol. 2009. 26:524–528.

16. Murray AB, Fraser BM, Hardwick DF, Pirie GE. Chronic asthma and growth failure in children. Lancet. 1976. 2:197–198.

17. Patel L, Clayton PE, Addison GM, Price DA, David TJ. Adrenal function following topical steroid treatment in children with atopic dermatitis. Br J Dermatol. 1995. 132:950–955.

18. Vermeer BJ, Heremans GF. A case of growth retardation and cushing\'s syndrome due to excessive application of betamethasone-17-valerate ointment. Dermatologica. 1974. 149:299–304.

19. Allen DB. Effects of inhaled steroids on growth, bone metabolism, and adrenal function. Adv Pediatr. 2006. 53:101–110.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download