Abstract
Background
Merkel cell carcinoma (MCC) is an increasingly common neuroendocrine cancer of the skin. Merkel cell polyomavirus (MCPyV) is one of the causative agents of MCC. The prevalence of MCPyV in primary MCC and sun-exposed non-MCC tumors has been known to have different results depending on where it was investigated.
Objective
This study assesses the prevalence of MCPyV from primary MCC and sun-exposed non-MCC tumors in Korea.
Methods
A molecular pathology study was performed on 7 tissue specimens of MCC, 1 tissue specimen of metastatic small cell carcinoma of the lung, and 32 tissue specimens of non-MCC tumors occurring from sun-exposed areas [8 basal cell carcinomas (BCCs), 8 squamous cell carcinomas (SCCs), 8 actinic keratoses (AKs), and 8 seborrheic keratoses (SKs)]. All specimens were analyzed to determine the presence of MCPyV-DNA using both polymerase chain reaction (PCR) and real-time quantitative PCR. Immunohistochemistry with monoclonal antibody of MCPyV large T antigen (CM2B4) was also conducted.
Merkel cell carcinoma (MCC) is a leading cause of death in non-melanoma skin cancer. MCC is a highly aggressive primary skin cancer with neuroendocrine differentiation, and frequently recurs in lymph nodes and distant metastases. The known risk factors for MCC include advanced age (>50 years), demographic factors (predominance of Europeans), and sun-exposed skin (ultraviolet radiation)1,2. Interestingly, MCC is also associated with immunosuppression (11-fold risk for people with AIDS and 5-fold for organ-transplanted patients)1,2. These findings linked to immunosuppression raised the possibility of a possible infectious etiology as the likely causative agent of MCC.
Polyomaviruses, small, double-stranded DNA viruses, have five known members of the polyomavirus family for which humans are the primary host. In 1971, BK and JC viruses were identified3,4, followed by WU and KI polyomaviruses discovered in 20075,6. In 2008, Feng et al.7 detected a novel human polyomavirus, named Merkel cell polyomavirus (MCPyV), suggested that MCPyV-infection and integration precede clonal expansion of MCC tumor cells, and that MCPyV may be a contributing factor in the pathogenesis of MCC. Several studies rapidly confirmed this initial finding8-10. Most results were inconsistent with previous findings7-10. MCPyV was detected in 75~89% of MCCs7-10. However, prevalence studies of MCPyV in the non-MCC population have given mixed results11-14.
To determine if MCPyV plays a role in MCC and non-MCC tumors in Korea, we examined tumor specimens obtained from immunocompetent patients with primary MCC and other non-MCC skin cancers using a polymerase chain reaction (PCR) and real time quantitative PCR (RT-PCR). Immunohistochemistry was also conducted with CM2B4, a monoclonal antibody raised against exon 2 of the MCPyV large T (LT) antigen15.
Seven Korean patients were identified as having a pathologic diagnosis of primary MCC on sun-exposed skin. This study included other non-melanoma tumor tissues from one Korean patient with metastatic small cell carcinoma of lung origin and from 32 Korean patients with 8 basal cell carcinomas (BCC), 8 squamous cell carcinomas (SCC), 8 actinic keratoses (AK), and 8 seborrheic keratoses (SK) occurring in sun-exposed areas.
These specimens were taken between 2000 and 2010 in Chonnam province of South Korea. Archival formalin-fixed paraffin-embedded (FFPE) MCC and other non-MCC skin tumor blocks were retrieved, and the patients' charts were reviewed. All MCC cases were confirmed by immunostaining with cytokeratin 20, cytokeratin 7, epithelial membrane antigen, neuron specific enolase, thyroid transcription factor-1, and others. Serial sections of all specimens were used for DNA preparation and CM2B4 immunostain.
DNA extraction from FFPE specimens and PCR analysis were performed as previously described16. Tumor-rich areas of each tumor block were extracted from three paraffin sections of 10 µm thickness. DNA was isolated using QIAamp DNA FFPE Tissue Kit (Qiagen, Fremont, CA, USA) according to the manufacturer's instructions. A PCR pre-mixture kit (ELPIS, Daejeon, Korea) was used for semi-quantitative PCR. To detect MCPyV DNA, we used two sets of primers to target the large and small T-antigen region. Their primer sequences were as follows: 138 base-pair product (MCV138 forward 5'-GGTTAGAGATGCTGGAAATGACC-3' and reverse 5'-CAAATAAGCAGCAGTACCAGGC-3'), and 191 base pair product (MCV191 forward 5'-CCACTTTATTATCTTAGCCCAT-3' and reverse 5'-TCCTTTTGGCTAGAACAGTGTC-3').
MCPyV DNA was quantified by an RT-PCR assay in all specimens. Total mRNA was isolated from FFPE sections using the RNeasy mini kit (Qiagen). The cDNA was obtained from 500 ng of total RNA using the Omniscript RT kit (Qiagen). RT-PCR was performed using the HOT FIREPol EvaGreen® qPCR Mix Plus (Solis BioDyne, Tartu, Estonia), in triplicates, through the RotorGene 3000 (Corbett Research Co., Mortlake, Australia) based on the same primers used for the PCR. DNA quality was confirmed by PCR using GAPDH (forward 5'-TGACCACAGTCCATGCCATC-3' and reverse 5'-TTACTCCTTGGAGGCCATGT-3'). The PCR-negative controls were constantly negative in all experiments. All the sequenced PCR amplicons showed 97~99% homology in the National Center for Biotechnology information (NCBI) Entrez Nucleotide database gb/EU 375803.1 MCPyV isolate MCC350, using the NCBI BLAST searches.
To estimate MCPyV infection and expression of MCPyV T antigen protein, archival paraffin-embedded tissue blocks were stained with a monoclonal antibody, CM2B4, raised against exon 2 of the MCPyV T antigen15. Epitope retrieval was performed using an EDTA antigen retrieval buffer (DAKO, Glostrup, Denmark). After blocking with Protein Block (DAKO), specimens were incubated with CM2B4 (1:50 dilution, Santa Cruz Biotechnology, Santa Cruz, CA, USA). After washing, specimens were incubated with Mouse Envision polymer (DAKO) for subsequent deaminobenzidine reactions. The methods have been described elsewhere15.
None of the patients were immunosuppressed. The mean age of all MCC patients was 62.4±20.7 years. There were more females (n=6, 85.7%) than males (n=1, 14.3%). MCPyV-DNA was detected in six of seven (85.7%) tissue specimens in the MCC group. The regions amplified by PCR corresponded with the genomic sequence of MCPyV (Fig. 1). All six females were positive in all the primer sets, while one male patient was negative for MCPyV-DNA in the tumor tissue. The mean age of the MCPyV-positive patients was 59.5±20.9 years. The mean age of the MCC group in this study was lower than in others, because one of the MCPyV-positive patients was a 22-year-old woman. She had undergone surgical excision twice, each time using radiation therapy. She presented with recurrent MCC on her right lower leg. The tumor was confirmed by repeated immunohistochemical staining and electron microscope study.
The MCPyV detection assays were applied to non-MCC tumors, including AK, SK, BCC, and SCC. A small cell carcinoma, which is a neuroendocrine carcinoma often confused with MCC because of its similar histology, was also included. All 32 non-MCC tumors on the sun-exposed skins were negative for MCPyV-DNA by PCR using both MCV138 and MCV191 primer sets (Fig. 1). In addition, MCPyV sequences were not detected in the DNA derived from the small cell carcinoma.
MCPyV DNA was quantified by an RT-PCR assay in all specimens. The MCPyV DNA level was significantly higher in MCC than in non-MCC skin tumors, which had similar levels with the control group (Fig. 2). Clinicopathologic data are summarized in Table 1.
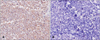
Five (71%) of the seven MCC tumors in our cohort were immunoreactive for CM2B4. All five immunoreactive cases were positive for MCPyV by PCR. MCC tumors that were positive by CM2B4 staining revealed antigen expression to the majority of tumor cells and showed diffuse nuclear staining (Fig. 3A). However, the antibody was not observed in the normal tissue cells surrounding the tumor cells. The small cell carcinoma, which did not detect MCPyV by PCR, did not show any immunoreactivity (Fig. 3B).
Several studies have confirmed the presence of clonal integration of MCPyV in the genomes for the majority of MCCs7-10, and revealed the prevalence of MCPyV in the non-MCC population and its possible role in the pathogenesis of other skin cancers11-16. Andres et al.16 detected the prevalence of MCPyV in 12 of 33 MCCs and in two of 33 among sun-exposed non-MCC tumors, which involved SK (n=12), BCC (n=11), and lentigo maligna melanoma (LMM, n=10). MCPyV was detected in two of 12 SK, while all LMM and BCC tissue specimens were negative for MCPyV16. They suggested that there were no relevant associations between MCPyV and SK, BCC, and LMM16. However, the prevalence of MCPyV in the non-MCC population is still disputed11-15.
Although the prevalence of malignant cancers such as BCC and SCC is high in Korea, the prevalence of MCC is probably very low compared to Europe and North America. This is because only a handful of primary MCC cases have been reported in the Korean literature and only seven patients were diagnosed during the past 11 years in our clinical center. Although our MCC group is too small to predict MCPyV-prevalence among MCC patients, the prevalence of MCPyV in MCC coincides with previous data7,9. Feng et al.7 identified a new human polyomavirus that showed monoclonal integration of MCPyV-genome in 8 of 10 MCCs (80%). Becker et al.9 observed the presence of MCPyV in 45 of 53 MCC patients of European descent (84.9%). Garneski et al.13 observed that North American MCC tumors were 69% positive for MCPyV DNA, while Australian MCC tumors were only 24% positive. They believed that this difference might be due to the increased sun exposure in Australia13. In Korea, viral infections may contribute to the pathogenesis of MCC as a more important cofactor since excessive sun exposure is generally avoided and the skin type is stronger against sun damage. In our study, MCPyV-DNA was identified from a 22 year-old woman MCC patient. This suggests that MCPyV might play a greater role in the development of MCC than sun exposure.
The prevalence of MCPyV in the non-MCC population revealed mixed findings11-14. MCV DNA prevalence is variably reported from 0% to 25% for SCC among immunocompetent patients11-13. Becker et al.9 documented a presence of MCPyV in 3 of 24 European-BCC-patients (12.5%). In the present study, non-MCC skin tumors included SK, AK, BCC, and SCC from immunocompetent patients. Interestingly, we were unable to detect any viral DNA in our non-MCC tumors groups from the immunocompetent patients. This result suggests that although non-MCC tumors may share several risk factors with MCC, such as advanced age and sun exposure, they may not be involved with MCPyV infection. The finding implicates the cause of low incidence of MCC in Korea. In our hypothesis, because the persons with MCPyV infection are very few in Korea, MCPyV was not detected in any of the non-MCC tumors, and MCC that was considered to be developed by MCPyV rarely occurred in Korea. Kassem et al.14, on the other hand, observed that 37.5% (36/96) of sporadic BCC among immunocompetent patients were MCPyV-positive. Rollison et al.11 detected MCV DNA in SCC tumor tissues from 55 of 145 cases (38%). They suggested that past exposure to MCPyV may be a risk factor for SCC11. Large-scale comprehensive studies are needed to show the prevalence of MCPyV in the non-MCC tumors.
MCPyV is a double-stranded DNA virus of 5,387 bp that expresses tumor (T) antigen mRNAs in tumor tissues7. BK, JC, WU, and KI human polyomaviruses belong to the SV40 subgroup, which induces tumor formation through the integration of polyomavirus DNA into the host in animals17. As SV40 LT antigen forces the cell into the S phase and promotes cell growth, MCPyV LT antigen also contains many common features18. The LT antigens derived from viruses in the MCC tumors have truncating mutations and lack the LT MCPyV helicase15. Shuda et al.15 developed a monoclonal antibody CM2B4 against a peptide fragment of the MCPyV T antigen exon 2 to detect MCPyV oncoprotein expression in the MCC tumor cells directly. The majority of the CM2B4-positive tumors showed strong and diffuse nuclear labeling in a large part of the tumor cell population and 77% of the PCR-positive tumors were immunoreactive for CM2B419. We examined seven MCC tumors, all of which were stained for CK20. Five of the seven tumors (71.4%) observed strong and diffuse nuclear labeling for CM2B4. All the tumors stained for CM2B4 were also positive for MCPyV by PCR (83.3% of all PCR-positive tumors). Although an immunostain using CM2B4 was less sensitive than PCR (71.4% vs. 85.7%, respectively) for MCPyV detection, it may be the simplest and most straightforward among several assays.
In summary, our findings of MCPyV by PCR and RT-PCR in 85.7% of our MCC patients were similar to previous reports. Although the sensitivity of MCPyV detection by CM2B4 staining was less compared to PCR, antibody MCPyV detection demonstrated a good correlation with the results obtained by the PCR method. Interestingly, in all the non-MCC tumors that shared risk factors with the MCCs, such as excessive sun damage and advanced age, MCPyV DNA was not detected. Our finding suggests that MCPyV may be a causal factor of MCC tumors, but not in non-MCC tumors in Korea.
Figures and Tables
 | Fig. 1Merkel cell polyomavirus (MCPyV) DNA was detected in six of seven (86%) tissue specimens from Merkel cell carcinoma (MCC) patients by polymerase chain reaction with two sets of primers (MCV138 and MCV191). BCC: basal cell carcinomas, SCC: squamous cell carcinomas, AK: actinic keratoses, SK: seborrheic keratoses. *Metastatic small cell carcinoma of the lung. |
 | Fig. 2Merkel cell polyomavirus (MCPyV) DNA was quantified by a real-time polymerase chain reaction assay. MCPyV DNA level was significantly higher in Merkel cell carcinoma (MCC) than in non-MCC skin tumors. BCC: basal cell carcinomas, SCC: squamous cell carcinomas, AK: actinic keratoses, SK: seborrheic keratoses. *Metastatic small cell carcinoma of the lung. |
References
1. Bichakjian CK, Lowe L, Lao CD, Sandler HM, Bradford CR, Johnson TM, et al. Merkel cell carcinoma: critical review with guidelines for multidisciplinary management. Cancer. 2007. 110:1–12.

2. Rockville Merkel Cell Carcinoma Group. Merkel cell carcinoma: recent progress and current priorities on etiology, pathogenesis, and clinical management. J Clin Oncol. 2009. 27:4021–4026.
3. Gardner SD, Field AM, Coleman DV, Hulme B. New human papovavirus (B.K.) isolated from urine after renal transplantation. Lancet. 1971. 1:1253–1257.

4. Padgett BL, Walker DL. Prevalence of antibodies in human sera against JC virus, an isolate from a case of progressive multifocal leukoencephalopathy. J Infect Dis. 1973. 127:467–470.

5. Gaynor AM, Nissen MD, Whiley DM, Mackay IM, Lambert SB, Wu G, et al. Identification of a novel polyomavirus from patients with acute respiratory tract infections. PLoS Pathog. 2007. 3:e64.

6. Allander T, Andreasson K, Gupta S, Bjerkner A, Bogdanovic G, Persson MA, et al. Identification of a third human polyomavirus. J Virol. 2007. 81:4130–4136.

7. Feng H, Shuda M, Chang Y, Moore PS. Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science. 2008. 319:1096–1100.

8. Kassem A, Schöpflin A, Diaz C, Weyers W, Stickeler E, Werner M, et al. Frequent detection of Merkel cell polyomavirus in human Merkel cell carcinomas and identification of a unique deletion in the VP1 gene. Cancer Res. 2008. 68:5009–5013.

9. Becker JC, Houben R, Ugurel S, Trefzer U, Pföhler C, Schrama D. MC polyomavirus is frequently present in Merkel cell carcinoma of European patients. J Invest Dermatol. 2009. 129:248–250.

10. Foulongne V, Kluger N, Dereure O, Brieu N, Guillot B, Segondy M. Merkel cell polyomavirus and Merkel cell carcinoma, France. Emerg Infect Dis. 2008. 14:1491–1493.

11. Rollison DE, Giuliano AR, Messina JL, Fenske NA, Cherpelis BS, Sondak VK, et al. Case-control study of Merkel cell polyomavirus infection and cutaneous squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev. 2012. 21:74–81.

12. Mangana J, Dziunycz P, Kerl K, Dummer R, Cozzio A. Prevalence of Merkel cell polyomavirus among Swiss Merkel cell carcinoma patients. Dermatology. 2010. 221:184–188.

13. Garneski KM, Warcola AH, Feng Q, Kiviat NB, Leonard JH, Nghiem P. Merkel cell polyomavirus is more frequently present in North American than Australian Merkel cell carcinoma tumors. J Invest Dermatol. 2009. 129:246–248.

14. Kassem A, Technau K, Kurz AK, Pantulu D, Löning M, Kayser G, et al. Merkel cell polyomavirus sequences are frequently detected in nonmelanoma skin cancer of immunosuppressed patients. Int J Cancer. 2009. 125:356–361.

15. Shuda M, Arora R, Kwun HJ, Feng H, Sarid R, Fernández-Figueras MT, et al. Human Merkel cell polyomavirus infection I. MCV T antigen expression in Merkel cell carcinoma, lymphoid tissues and lymphoid tumors. Int J Cancer. 2009. 125:1243–1249.

16. Andres C, Belloni B, Puchta U, Sander CA, Flaig MJ. Prevalence of MCPyV in Merkel cell carcinoma and non-MCC tumors. J Cutan Pathol. 2010. 37:28–34.

17. Holländerová D, Raslová H, Blangy D, Forstová J, Berebbi M. Interference of mouse polyomavirus with the c-myc gene and its product in mouse mammary adenocarcinomas. Int J Oncol. 2003. 23:333–341.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download