Abstract
Background
Topical application of corticosteroids also has an influence on skin barrier impairment. Physiological lipid mixtures, such as multi-lamellar emulsion (MLE) containing a natural lipid component leads to effective recovery of the barrier function.
Objective
The purpose of this study was to conduct an evaluation of the therapeutic efficacy and skin barrier protection of topical mometasone furoate in MLE.
Methods
A multi-center randomized, double-blind, controlled study was performed to assess the efficacy and safety of mometasone furoate cream in MLE for Korean patients with eczema. The study group included 175 patients with eczema, who applied either mometasone furoate in MLE cream or methylprednisolone aceponate cream for 2 weeks. Treatment efficacy was evaluated using the physician's global assessment of clinical response (PGA), trans-epidermal water loss (TEWL), and visual analogue scale (VAS) for pruritus. Patients were evaluated using these indices at days 4, 8, and 15.
Results
Comparison of PGA score, TEWL, and VAS score at baseline with those at days 4, 8, and 15 of treatment showed a significant improvement in both groups. Patients who applied mometasone furoate in MLE (74.8%) showed better results (p<0.05) than those who applied methylprednisolone aceponate (47.8%). The TEWL improvement ratio was higher in the mometasone furoate in MLE group than that in the methylprednisolone aceponate group, and VAS improvement was also better in the mometasone furoate in MLE group.
Topical steroids are an important and common treatment modality for eczematous skin disorders. The choice of topical steroid varies based on skin disease severity, potency, and delivery vehicle used. Appropriate use of a topical steroid makes it possible to treat an eczematous disorder effectively. However, they are many notable side effects such as skin atrophy, acneiform eruptions, hypertrichosis, hypopigmentation, and development of a cutaneous infection. Such topical glucocorticoid side effects make many patients hesitant to use topical steroids.
Efforts to minimize the side effects of topical steroids have been attempted. One approach is to develop novel steroids such as non-halogenated double-ester-type glucocorticoids1. Another technique is to use topical steroid together with an anti-atrophogenic substance2. In particular, topical materials that not only minimize side effects of topical steroid but enhance the physiological lipid mixture have been investigated.
Another important aspect of eczema treatment is normalizing the defective skin barrier, because impaired skin barrier function is an important factor in the pathogenesis of eczema. Skin barrier function is affected by multiple factors, including downregulation of filaggrin and locogrin, reduced ceramide levels, increased proteolytic enzyme levels, and enhanced trans-epidermal water loss (TEWL)3. The epidermal barrier is composed of a combination of corneocytes and intercellular lipids4,5. The stratum corneum (SC) provides a mechanical protection to the skin. It functions as a barrier to water loss and permeation of soluble substances from the environment. Regulation of permeability, desquamation, antimicrobial peptide activity, toxin exclusion, and selective chemical absorption are all primary functions of the extracellular lipid matrix. In contrast, mechanical reinforcement, hydration, cytokine-mediated initiation of inflammation, and protection from ultraviolet (UV) damage are all provided by corneocytes. Among various factors, hydrophobic intercellular lipids are the most important factor for skin barrier function, and diminished ceramides create a leaky barrier. Particularly in the case of atopic dermatitis (AD), abnormal barrier function results from disruption of the multi-lamellar structure due to a significant reduction in the amount of intercellular lipid ceramides in the SC6-8.
A disrupted skin barrier can be replenished by a physiological lipid mixture. Multi-lamellar emulsions (MLEs) containing pseudoceramide has a multi-lamellar structure similar to intercellular lipids of the SC9. Lee et al.9 reported that patients with AD treated only with a MLE improved more than those applying a commercial moisturizing cream in an objective assessment and subjective satisfaction scores for symptoms and signs. Ahn et al.10 reported on a co-application of MLE for topical steroid-protected skin barrier function, reinforcing the skin barrier permeability. Topical application of ceramides results in restoration of barrier function by reducing TEWL9. Effective enhancement of skin barrier function with a physiological lipid mixture has been reported recently. Chamlin et al.11 reported on alleviation of childhood AD using a ceramide-dominant, barrier-repair lipid, and attributed the improvement seen in their patients to a normalization of barrier function, which in turn dampened the cytokine cascade that initiates and sustains AD.
Mometasone furoate is a potent topical steroid with proven efficacy, similar to betametasone12,13. Mometasone furoate contains hexylene glycol, which has antimicrobial properties. The effects of hexylene glycol on microorganisms may potentially be beneficial for treating eczematous disorders, with effects on microorganisms, possibly leading to better treatment and a longer relapse-free period14. It is also a safe and effective method for a long-term use to treat chronic, recurrent disease.
This study was performed to evaluate the clinical efficacy of this physiological lipid mixture as a vehicle of mometasone furoate in patients with eczema. We designed a multi-center, randomized, double-blind controlled assessment to compare mometasone furoate in MLE with methylprednisolone aceponate.
Patients with eczema and moderate to severe manifestations were enrolled. All patients showed eczematous skin lesions, presenting symmetrically. Patients <4 years old were excluded. The following patients were also excluded from the study: patients currently undergoing treatment with systemic glucocorticoids, antibiotics or immunosuppressive agents; those treated with UV radiation; those with other chronic non-eczematous skin diseases; those with infectious dermatoses, chronic medical illness such as diabetes; those pregnant or lactating; those with skin lesions involving the face or genital area; and those with other severe dermatoses or scars. We used a wash-out period for patients who had undergone treatment with topical and systemic corticosteroids. Patients taking a systemic corticosteroid had a wash-out period of 4 weeks. Patients who applied a topical corticosteroid had a wash-out period of 1 week. This study was approved by the Institutional Review Boards at Incheon St. Mary's Hospital, Kangnam Sacred Heart Hospital, Seoul National University Hospital, Severance Hospital, and Kwandong University Myongji Hospital.
After informed consent was obtained, the patients were randomly assigned to apply mometasone furorate in MLE on one side and apply methylprednisolone aceponate on the other side. The topically applied formulations were mometasone furoate in MLE and methylprednisolone aceponate. Together on each randomly assigned side, mometasone furoate in MLE was applied on one side for 2 weeks, and methylprednisolone aceponate was applied on the other side for 2 weeks. Mometasone furoate in MLE or methylprednisolone aceponate was applied topically to skin lesions once daily by all subjects.
The study included a baseline visit before treatment, and on days 1, 4, 8, and 15 after treatment initiation. Patients were observed and assessed by one physician on days 1, 4, 8, and 15 throughout the trial. The physician's global assessment of clinical response (PGA) score was adopted for an objective assessment of the clinical response to treatment. The PGA index was calculated from scales of erythema, vesiculation, pruritus, and burning/pain. Each parameter was judged on a 0~3 scale: 0=no symptoms, 1=mild, 2=moderate, and 3=severe. Clinical efficacy was assessed by the PGA improvement ratio. The PGA improvement ratio was calculated as:
PGA improvement ratio (%)=[(PGAday1-PGAdayn)/PGAday1]×100 (%)
The TEWL was measured by Tewameter® to evaluate epidermal permeability barrier function (Courage & Khazaka, Cologne, Germany) on days 1, 4, 8, and 15. Clinical efficacy of the improved skin barrier function was assessed by the TEWL improvement ratio. The TEWL improvement ratio was calculated as:
TEWL improvement ratio (%)=[(TEWLday1-TEWLdayn)/TEWLday1]×100 (%)
In addition, improvement of pruritus after treatment was assessed subjectively, using 10 visual analog scales that the patients scored. The visual analogue scale (VAS) improvement ratio was calculated as:
VAS improvement ratio (%)=[(VASday1-VASdayn)/VASday1] ×100 (%)
All adverse events were recorded, and whether they were treatment related or not was also noted.
Mcnemar's t-test was used to compare the PGA improvement ratio on days 1, 4, 8, and 15 of treatment. p<0.05 were regarded as statistically significant. A paired t-test and the Wilcoxon signed-rank test were used to verify significant differences in TEWL and VAS scores between groups A and B during the follow-up period.
A total of 175 patients were initially enrolled. Fifteen patients were excluded due either to violation of protocols or adverse reactions, and one patient was excluded due to a screening criteria violation. In total, 159 patients were analyzed (76 males and 83 females; age range, 5~79 years; mean age, 32.32±19.86, mean±standard deviation years old). No clinically significant differences were observed in the PGA score, TEWL, or VAS between the mometasone furoate in MLE group and the methylprednisolone aceponate group. Basal demographic characteristics of the study groups and basal results of the PGA, TEWL, and VAS scores are summarized in Table 1 and 2.
We performed a data analysis on patients who completed 15 days of treatment to assess efficacy. Comparison of the PGA score improvement ratio at baseline with days 4, 8, and 15 of treatment showed a significant increase for all follow-up periods. At baseline, the mean PGA score was 7.46±3.11 in the mometasone furoate in MLE group and 7.51±3.18 in the methylprednisolone group. After 15 days, the PGA improvement ratio in the mometasone furoate in MLE group was 82.62±21.62%, and that in the methylprednisolone acetonate group was 68.32±24.05% (p≤0.0001). The PGA improvement ratio for days 4, 8, and 15 is summarized in Fig. 1.
At baseline, the baseline TEWL score in the mometasone furoate in MLE group was 33.73±22.47 g/h/m2 and 33.05±21.96 g/h/m2 in the methylprednisolone acetonate group. No significant difference was observed between the groups. After 15 days of treatment, the TEWL improvement ratio increased in both groups for all follow-up periods. After 15 days of treatment in the mometasone furoate in MLE group, the TEWL improvement ratio, which was 48.30±68.04% at baseline, was statistically significant; and in the methylprednisolone acetonate group, the TEWL improvement ratio increased 32.74±50.07% from baseline after 15 days. Although the TEWL improvement ratio increased in both groups, the TEWL improvement ratio in the mometasone furoate in MLE group was superior to that in the methylprednisolone acetonate group (p≤0.0001). The TEWL improvement ratio for days 4, 8, and 15 is summarized in Fig. 2. The intergroup differences were statistically significant at every point.
The subjective VAS score was measured at every visit to evaluate improvement of pruritus. The initial VAS score was 5.83±2.31 in the mometasone furoate in MLE group and 5.99±2.29 in the methylprednisolone aceponate group (p>0.05). The VAS improvement ratio increased in both groups for all follow-up periods. After 15 days of treatment, the VAS improvement ratio score increased 83.28±23.47% from baseline in the mometasone furoate in MLE group and 75.41±27.24% in the methylprednisolone group.
In addition, pruritus showed a more significant improvement in the mometasone furoate in MLE group than that in the methylprednisolone group (p≤0.0001). The VAS improvement ratio at days 4 and 8 also showed an increase from baseline; however, no statistically significant intergroup difference was observed (p=0.2117, p=0.1131). The VAS improvement ratio on days 4, 8, and 15 is summarized in Fig. 3. The difference was statistically significant at day 15 (p≤0.0001).
An itching sensation was observed in two patients (1.15%) who applied mometasone furoate in MLE and in 4 patients (2.30%) who applied methylprednisolone aceponate. Urticaria was observed in one patient (0.57%). Herpes virus infection was observed in one patient (0.57%) at a non-applied site. Five patients were excluded from the study due to pruritus and urticaria.
Both mometasone furoate in MLE and methylprednisolone aceponate were effective treatments for eczema. Statistically significant differences in the PGA score were observed between the values at baseline and at day 15 of treatment. Patients who applied mometasone furoate in MLE showed better results in the PGA improvement ratio than those who applied methylprednisolone aceponate. Both agents are potent group II corticosteroids, and they had shown similar efficacy in previous studies. However, mometasone furoate in MLE showed superior efficacy, likely due to the effects of the physiological lipid mixture on enhanced skin barrier function.
This was supported by the results showing TEWL improvement, as it mirrors the skin barrier function. The TEWL improvement ratio was also higher in those who applied mometasone furoate in MLE. Prolonged treatment with a topical steroid creates structural defects in the epidermis, which has been attributed to a disturbance in epidermal differentiation and thinning of the SC10. A disrupted skin barrier due to abnormalities in intercellular lipid lamellae, which are thought to mediate transcutaneous water loss, results in an increase in TEWL score10. The VAS improvement ratio was higher with the physiological lipid mixture. Applying mometasone furoate in MLE resulted in significant improvement in clinical symptoms and signs of eczematous disorder. Subjectively, patients felt less of an itching sensation over the treatment period.
Topical corticosteroids not only have antiproliferative effects but also suppress differentiation of the epidermal layer, resulting in defects in the epidermis10. Therefore, long-term use of topical glucocorticoid causes weakening of the skin barrier. Many studies have been performed to minimize the side effects of glucocorticoids. One attempt involves reinforcing the skin barrier function using a physiological lipid mixture. Man MQ et al.15 reported that topical application of a physiological lipid mixture results in accelerated recovery of barrier function, whereas an incomplete lipid mixture may inhibit the normal recovery response. Additionally, topical application of an MLE containing a pseudoceramide results in significantly decreased TEWL and skin pH16. Ahn et al.10 reported that concurrent application of MLE with steroid significantly reduces skin atrophy induced by steroid.
The physiological lipid mixture using a vehicle allows for the penetration of topical steroid into the skin and enhances delivery. Mometasone furorate in MLE showed a more beneficial effect than that of methylprednisolone aceponate, which has similar potency but not the physiological lipid mixture. As such, the treatment period for a topical steroid would be shortened using the same potency. The side effects of topical steroids are dependent on duration and frequency of application17. It is possible that the lower steroid potency causes similar effects to a higher potency steroid. We suggest that a physiological lipid mixture as a topical steroid vehicle enhances the effects of a topical steroid and diminishes the side effects.
Use of moisturizers is an important treatment method to improve skin hydration, even when overt disease is not observed. Daily treatment with topical moisturizers prevents exacerbation of skin lesions by reducing elevated TEWL. The MLE-containing moisturizers are effective for hydration of eczema and have a safety profile9. A physiological lipid mixture using pseudoceramides is presented in an orthorhombic lipid phase, which chiefly exists on the human SC lipid, while non-physiological lipid mixture moisturizers only show a liquid crystalline phase and a hexagonal phase. An increase in TEWL results in skin dehydration, and xerosis cutis itself aggravates eczematous disease and makes pruritus more severe.
Pruritus, the most common and important symptom of an eczematous skin disorder, causes a vicious itching-scratching cycle. Therefore, rapid amelioration of pruritus shortens disease duration and enhances treatment compliance. In recent studies, a physiological lipid mixture using pseudoceramides not only restored the skin barrier but also had an anti-inflammatory effect. Kang et al.18 reported that topical application of MLE using pseudoceramides results in diminished mRNA expression of interleukin (IL)-4 and tumor necrosis factor-α in murine atopic dermatitis-like skin lesions. IL-4 and IL-13 play a major role in allergic reactions. A suppressed immune response diminishes the cytokine cascade involved in the pathogenesis of pruritus.
In our study, only a few local side effects were observed such as pruritus and urticaria. The intensity of the itching sensation was mild, and the duration was a few hours to a day. As such, local side effects rarely required discontinuation of treatment.
In conclusion, mometasone furoate in MLE was a more effective treatment for moderate to severe skin eczema than that of methylprednisolone. As mometasone furoate in MLE induced improvement in skin barrier function, and we recommend more studies using of physiological lipid mixtures as a vehicle for topical therapeutic agents.
Figures and Tables
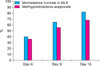 | Fig. 1The physician's global assessment of clinical response (PGA) improvement ratio at day 4, 8, 15. Comparison of the PGA improvement ratio between themometasone furoate in multi-lamella emulsion (MLE) group and the methylprednisolone group. A significant difference was observed in the PGA improvement ratio at all follow-up periods (p≤0.0001). |
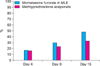 | Fig. 2The trans-epidermal water loss (TEWL) improvement ratio. Comparison of the TEWL improvement ratio between the mometasone furorate in multi-lamella emulsion (MLE) group and the methylprednisolone group. A significant difference was observed in the TEWL improvement ratio at all follow-up periods (p≤0.0001). |
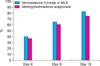 | Fig. 3The visual analog scale (VAS) improvement ratio. Comparison of the VAS improvement ratio between the mometasone furorate in multi-lamella emulsion (MLE) group and the methylprednisolone group. A significant difference was observed in the VAS improvement ratio at day 15 (p≤0.0001). |
References
1. Lange K, Gysler A, Bader M, Kleuser B, Korting HC, Schäfer-Korting M. Prednicarbate versus conventional topical glucocorticoids: pharmacodynamic characterization in vitro. Pharm Res. 1997. 14:1744–1749.
2. Lubach D, Rath J, Kietzmann M. Steroid-induced dermal thinning: discontinuous application of clobetasol-17-propionate ointment. Dermatology. 1992. 185:44–48.

3. Leung DYM, Eichenfield LF, Boguniewicz M. Wolff K, Fitzpatrick TB, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, editors. Atopic dermatitis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;146–158.
6. Williams HC. Is the prevalence of atopic dermatitis increasing? Clin Exp Dermatol. 1992. 17:385–391.

7. Ogawa H, Yoshiike T. A speculative view of atopic dermatitis: barrier dysfunction in pathogenesis. J Dermatol Sci. 1993. 5:197–204.

8. Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin? J Invest Dermatol. 1991. 96:523–526.

9. Lee EJ, Suhr KB, Lee JH, Park JK, Jin CY, Youm JK, et al. The clinical efficacy of a multi-lamellar emulsion containing pseudoceramide in childhood atopic dermatitis: an open crossover study. Ann Dermatol. 2003. 15:133–138.

10. Ahn SK, Bak HN, Park BD, Kim YH, Youm JK, Choi EH, et al. Effects of a multilamellar emulsion on glucocorticoid-induced epidermal atrophy and barrier impairment. J Dermatol. 2006. 33:80–90.

11. Chamlin SL, Frieden IJ, Fowler A, Williams M, Kao J, Sheu M, et al. Ceramide-dominant, barrier-repair lipids improve childhood atopic dermatitis. Arch Dermatol. 2001. 137:1110–1112.
12. Hoybye S, Balk MS, De Cunha Bang F, Ottevanger V, Veien NK. Continuous and intermittent treatment of atopic dermatitis in adults with mometasone furoate versus hydrocortisone 17-butyrate. Curr Ther Res Clin Exp. 1991. 50:67–72.
13. Rakja G, Avrach W, Gärtner L, Overgaard-Petersen H. Mometasone furoate 0.1% fatty cream once daily versus betamethasone valerate 0.1% cream twice daily in the treatment of patients with atopic and allergic contact dermatitis. Curr Ther Res. 1993. 54:23–29.

14. Faergemann J, Christensen O, Sjövall P, Johnsson A, Hersle K, Nordin P, et al. An open study of efficacy and safety of long-term treatment with mometasone furoate fatty cream in the treatment of adult patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2000. 14:393–396.

15. Man MQ M, Feingold KR, Thornfeldt CR, Elias PM. Optimization of physiological lipid mixtures for barrier repair. J Invest Dermatol. 1996. 106:1096–1101.

16. Kim HJ, Park HJ, Yun JN, Jeong SK, Ahn SK, Lee SH. Pseudoceramide-containing physiological lipid mixture reduces adverse effects of topical steroids. Allergy Asthma Immunol Res. 2011. 3:96–102.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download