Abstract
Lichens striatus (LS) is an acquired, self-limiting inflammatory dermatosis that follows the lines of Blaschko. The etiology of the eruption is unknown, but several theories have been proposed with focus on environmental factors, viral infection, cutaneous injury, hypersensitivity, and genetic predisposition. We describe a 19-year-old woman who developed a unilateral linear eruption 17 months after allogenic peripheral blood stem cell transplantation. Histopathology revealed features, which were consistent with LS. To the best of our knowledge, our patient is the first case describing the appearance of LS occurring after allogenic stem cell transplantation. We speculate that this condition represents an unusual form of localized, chronic graft-versus-host disease.
Lichen striatus (LS) is a self-limiting, inflammatory, linear dermatitis of unknown origin. It is an eruption characterized by sudden onset of flat-topped, 1 to 4 mm, pink, tan, or hypopigmented papules in a linear configuration or Blaschkoid distribution. The etiology of LS still remains elusive but it has been observed in atopic patients and subsequent to immunization or infection1. In our present report, we describe the development of LS in a patient with aplastic anemia after allogenic peripheral blood stem cell transplantation (PBSCT).
A 19-year old Korean woman was presented with 1-month history of an asymptomatic linear eruption on the left upper back and left arm. The lesion had initially appeared on the left wrist and slowly extended to left arm and back over the period of 3 weeks to form a linear band. About 17 months back, she underwent allogenic PBSCT from unrelated donor, as she was suffering from aplastic anemia. The PBSCT was successful and she didn't have any infections or graft-versus host disease except for herpes zoster on left T9 dermatome about 6 months back.
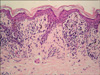
Physical examination revealed linearly arranged brownish to erythematous papules on and along the left wrist, arm and left back following the line of Blaschko (Fig. 1). Histopathologic examination of papules on left arm revealed the presence of a lichenoid, lymphocytic infiltration and scattered melanin incontinence in the papillary dermis with epidermal hyperkeratosis, exocytosis of lymphocytes and necrotic keratinocytes (Fig. 2). This condition was compatible with lichen striatus. The patient was treated with topical application of 0.1% tacrolimus ointment, twice daily. After 2 months of follow-up examination, it was seen that the lesion disappeared leaving mild hyperpigmentation.
To the best of our knowledge, our patient is the first report of LS occurring after allogenic stem cell transplantation (SCT). Blaschko lines have an embryologic origin and correspond to the direction of growth of the cutaneous cells, resulting in a cutaneous mosaicism2. The genetic mosaicism could be responsible for cutaneous antigenic mosaicism, and for instance the expression of which might be induced by a viral infection3. The viral infection could then trigger an inflammatory T-cell response in a Blaschko-linear fashion3. From pathogenetic point of view, LS has been considered to be the consequence of an acquired stimulus that induces a loss of immunotolerance to embryologically abnormal clones, resulting in a T-cell-mediated inflammatory reaction1. At base line, the aberrant clone of keratinocytes is not clinically apparent. However, several triggering factors such as infection, immunization, cutaneous injury, hypersensitivity have been reported to induce a loss of immunotolerance to embryologically abnormal clones, resulting in a T-cell-mediated inflammation (Fig. 3)1.
After allogenic SCT, the transplanted graft could contain immunologic competent cells, which can attack the recipient tissues, which are not present in the transplant donor. Graft-versus-host disease (GVHD) occurs by its own mechanism. Based on the time of presentation, cutaneous GVHD is divided into acute (<100 days after transplantation) and chronic disease (>100 days after transplantation). The chronic GVHD is further subclassified into a more epithelial or lichenoid and a main dermal or sclerodermoid form4. Lichenoid GVHD following a unilateral linear configuration was reported by Beers et al.5 While acute GVHD results from the action of alloreactive immunocompetent donor T cells, chronic GVHD occurs when autoreactive donor T cells differentiating within the host reacts against "altered self" or normal allogeneic determinants on host cells6. Viral infections may induce viral antigens that mimic minor or major histocompatibility complex antigens and trigger immune responses that induce GVHD5.
To our knowledge, LS has not been reported as a manifestation of chronic GVHD. In the case presented here, we believe that the occurrence of LS in our patient after PBSCT is more than just a mere coincidence. We postulate that the donor cells recognize the aberrant clone of keratinocytes by the mechanism of chronic GVHD, which had not been reacted by patient's own cells because of immunologic tolerance, developed in fetal life. Therefore, we think that SCT could be one of the triggering factors in the development of LS. In addition, we further report that LS after PBSCT may be a subtype of chronic GVHD. Further research and reports are needed to confirm this theory.
Figures and Tables
 | Fig. 1Linear brownish to erythematous papules along the left back and arm following the Blaschko line. |
References
1. Patrizi A, Neri I, Fiorentini C, Bonci A, Ricci G. Lichen striatus: clinical and laboratory features of 115 children. Pediatr Dermatol. 2004. 21:197–204.

3. Lipsker D, Cribier B, Girard-Lemaire F, Flori E, Grosshans E. Genetic mosaicism in an acquired inflammatory dermatosis following the lines of Blaschko. Arch Dermatol. 2000. 136:805–807.

4. Häusermann P, Walter RB, Halter J, Biedermann BC, Tichelli A, Itin P, et al. Cutaneous graft-versus-host disease: a guide for the dermatologist. Dermatology. 2008. 216:287–304.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download