Abstract
Angiokeratoma is a rare vascular malformation of the upper dermis that presents clinically as deep red to blue-black in color and tends to take a diverse configuration without self-limiting. Here, we reported dermoscopic findings by two cases of angiokeratoma; solitary angiokeratoma and angiokeratoma circumscriptum. A 24-year-old male presented with a 2-months history of 5 mm sized black colored papule on the right buttock. A dermoscopic pattern characterized by red and dark lacunae, whitish veil covered with scale. A 26-year-old woman presented with multiple, 2~10 mm, dark colored papules on the anterior neck with zosteriform fashion since childhood. A dermoscopic pattern presented by red lacunae intermingled with whitish veil. As a previous report, our two cases was the most common dermoscopic pattern of angiokeratoma; red lacunae and whitish veil. Angiokeratoma is often diagnosed as melanocytic nevi, Spitz nevi, malignant melanomas, pigmented basal cell carcinomas, seborrheic keratoses, dermatofibromas and other vascular lesions including hemangiomas and pyogenic granulomas. However, in the dermoscopic view, these above lesions hardly show red lacunae with whitish veils. Therefore, the dermscopic view is a useful differential method of angiokeratoma.
Angiokeratomas (AKs) are benign vascular tumors characterized by red-blue verrucous hyperkeratotic papules with a diameter of 2 to 10 mm. Recently, dermoscopy has become a very useful method for the preoperative diagnosis of vascular lesions including AKs1. Zaballos et al.2 categorized three dermoscopic patterns of AKs, consisting of dark or red lacunae, a whitish veil, and peripheral erythema with a hemorrhagic crust2,3. In this study we present two cases of AKs diagnosed usefully as dermoscopic patterns.
A 24-year-old male presented at our outpatient clinic with a two-months history of a 5-mm black papule on the right buttock (Fig. 1a). The patient had a history of frequent bleeding of the lesion after washing without other trauma. The dermoscopic patterns were characterized by a whitish veil covered with scales and dark lacunae (Fig. 1c). Skin biopsy of the lesion showed numerous dilated, and thin-walled congested capillaries on the dermis and hyperkeratosis, with rete ridge elongations (Fig. 1b). AK was confirmed by clinical and histological examinations.
A 26-year-old woman presented with multiple lesions on the anterior neck since childhood. Physical examination revealed multiple 2~10 mm, dark, and zosteriform papules on the anterior neck (Fig. 2a). The patient had no previous history of bleeding from the lesions. The dermoscopic pattern showed red lacunae intermingled with a whitish veil (Fig. 2b). A punch biopsy specimen from the largest lesion on the anterior neck revealed hyperkeratosis and several dilated dermal vessels fully congested with red blood cells, which is consistent with AK (Fig. 2c).
AKs are rare vascular malformations of the upper dermis, which present clinically with deep-red to blue-black color and tend to take diverse, non-self-limiting configurations. The five clinical forms of AKs have been demonstrated as follows: (1) solitary and multiple AK, (2) AK circumscriptum, (3) AK Fordyce, (4) AK Mibelli, and (5) AK corporis diffusum4. AKs are histologically characterized by dilated subepidermal vessels congested with erythrocytes from large lacunae only in the papillary dermis. Acanthosis, papillomatosis and hyperkeratosis in the epidermis are also typical findings of AKs on the histological examination. Histologically, differential diagnosis of AKs includes verrucous hemangiomas, lymphangiomas, angiomas and malignant melanomas5. Verrucous hemangiomas show dilated capillaries in the deep dermis, and subcutaneous fat with hyperkeratosis. Lymphangiomas have a characteristic vascular space, usually without congested erythrocytes. Angiomas rarely show hyperkeratotic epidermis. Malignant melanomas show atypical melanocytes with invasion of the dermis. Our two cases showed solitary AK and AK circumscriptum by clinicopathologic examinations.
In the dermoscopic view, Zaballos et al.2 reported that the presence of well-demarcated, round, and dark lacunae which histologically represent dilated vessels with thrombosis is a strong diagnostic sign of AK. Red lacunae refer to dilated vascular spaces without thrombosis in the upper dermis, while a whitish veil corresponds to acanthosis or hyperkeratosis. AKs were divided into three patterns by dermoscopic view2. All patterns include dark lacunae and whitish veil. Pattern 1 (sensitivity 84.4%, specificity 99.1%) consists of no other features, while pattern 2 (sensitivity 43.8%, specificity 100%) consists of peripheral erythema, and pattern 3 (sensitivity 53.1%, specificity 99.6%) consists of hemorrhagic crusts2. Our two cases showed that pattern 1 was the most common dermoscopic pattern of AKs, and AK circumscriptum presented less whitish veils than solitary AK. The difference in the number of rete ridge elongations can explain this phenomenon.
AKs are sometimes clinically misdiagnosed as pigmented lesions including melanocytic nevi, Spitz nevi, malignant melanomas and vascular lesions such as angiomas, hemangiomas and pyogenic granulomas. A previous report found that 20% of angiokeratomas were clinically diagnosed as melanomas6. However, in the dermoscopic view, non-vascular lesions rarely show red or dark lacunae with high specificity2. Pigmented lesions such as melanomas rarely show red or dark lacunae without whitish veils on the dermoscopic examination, which differs from AKs. Hemangiomas, dermoscopically reveal typically reddish or red-bluish colored lacunae which are not as sharply circumscribed as AKs6. Pyogenic granulomas can be confused with AKs because of the presence of the whitish veils, but are differentiated with AKs due to the absence of red of dark lacunae7. With dermoscopy, however, it is difficult to discriminate between verrucous hemangioma and AKs because of its difficulty in estimating the depth of lesion. The previous study suggested that differences of dermoscopic views exist in vascular patterns between the Asian and non-Asian groups8. A large study is needed to determine the dermoscopic signs presented by Asian patients only compared to other ethnic patients.
Therefore, we confirmed that dermoscopy is an easily applicable tool for diagnosis of AKs and the three angiokeratoma dermoscopic patterns provide useful differential criteria for non-vascular, as well as vascular lesions.
Figures and Tables
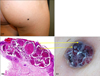 | Fig. 1(a) Five-millimeter black lesion is shown on the right buttock. (b) Histopathology and (c) dermoscopy of the lesion are shown. Dilated vascular spaces in the papillary dermis with thrombosis presented as dark lacunae. Hyperkeratosis and acanthosis appeared as a whitish veil (H&E, ×100). |
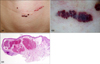 | Fig. 2(a) Multiple dark zosteriform papules on the anterior neck, shown macroscopically. (b) Dermoscopy of the lesion showed red and black lacunae with a whitish veil. (c) Microscopic appearance of the lesion showing hyperkeratosis and several dermal dilated vessels fully congested with red blood cells (H&E, ×100). |
References
2. Zaballos P, Daufí C, Puig S, Argenziano G, Moreno-Ramírez D, Cabo H, et al. Dermoscopy of solitary angiokeratomas: a morphological study. Arch Dermatol. 2007. 143:318–325.
3. Sahin MT, Türel-Ermertcan A, Oztürkcan S, Türkdogan P. Thrombosed solitary angiokeratoma of Mibelli simulating malignant melanoma: the importance of dermoscopy in differential diagnosis. J Eur Acad Dermatol Venereol. 2006. 20:102–104.
4. Mittal R, Aggarwal A, Srivastava G. Angiokeratoma circumscriptum: a case report and review of the literature. Int J Dermatol. 2005. 44:1031–1034.

5. Naranjo Sintes R, Pereda Hernandez J, Delgado Florencio V, Linares Solano J. Angiokeratoma. Apropos of 93 cases. Med Cutan Ibero Lat Am. 1988. 16:255–261.
6. Campos-do-Carmo G, Ramos-e-Silva M. Dermoscopy: basic concepts. Int J Dermatol. 2008. 47:712–719.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download