Abstract
Background
Patients with fever and rash often pose an urgent diagnostic and therapeutic dilemma for the clinician. The nonspecificity of many fever and rash syndromes mandates a systemic approach to diagnosis.
Objective
We
aimed to determine the etiology of fever and rash in 100 adult patients followed-up as in- or outpatients prospectively.
Methods
All the patients, who presented with rash and fever, were followed-up prospectively and their clinical and laboratory studies were evaluated.
Results
The median age was 35 years (14~79 years); 45 were female and 55 were male. Patients were divided into 3 groups according to the etiology: infectious (50%), noninfectious (40%) and undiagnosed (10%). The most common type of rash was maculopapular, and the most common 5 causes were measles, cutaneous drug reactions, varicella, adult-onset Still's disease (ASD) and rickettsial disease. Viral diseases among infectious causes and cutaneous drug reactions, among the noninfectious causes, were determined as the main diseases. The mortality rate was 5% and the reasons of mortality were as follows: toxic epidermal necrolysis (2 patients), ASD (1), staphylococcal toxic shock syndrome (1) and graft-versus-host disease (1).
Conclusion
Adult patients with fever and rash had a wide differential diagnosis. The most common type of rash was determined as maculopapular, and the most frequent five diseases were measles, drug reactions, chickenpox, ASD and rickettsial infection. Viral diseases among infectious causes and drug reactions among noninfectious causes were determined as the leading etiologies.
Clinicians are often faced with diseases that are presented with fever and rash. They require quick and rational approach because some of these patients might be in a life-threatening condition or need isolation in order to decrase its potential transmission to others.
A detailed history and physical examination are essential. Basic laboratory tests, dermatology consultation and skin biopsy, when needed, are all helpful for the diagnosis. Diagrams of differential diagnosis based on history and physical examination and epidemiology of the diseases with fever and rash may contribute to the establishment of diagnosis. These may delay the decisions about the need of isolation and start of antimicrobial treatment because of several causes, such as pending test results, confirmation of diagnosis and consequently following the patient, either in outpatient or inpatient settings.
An appropriate approach to a patient with fever and rash needs history, physical examination, biochemical and microbiological investigations. Up to our search, there are no studies aiming to detect the etiology of patients admitted with fever and rash in the English language literature (Pubmed 1963-2010). We aimed prospectively to find out the etiologies of consecutive adult patients with fever and rash.
The study was approved by the Institution Review Board of the medical school.
Consecutive adult patients with fever and rash were evaluated, and the data were filled in a dedicated form prospectively in Istanbul University, Cerrahpaşa Medical Faculty, Infectious Diseases and Internal Medicine Departments. They were followed as the outpatient or inpatient and diagnostic tests and treatment were made when needed.
Cases with axillary fever of ≥37.5℃ and rash in any part of the body were evaluated, and their data, such as age, gender, any previously diagnosed disease, vaccination in childhood, contact with a patient with rash and fever, contact with an animal, suspicious sexual contact, journey, drug use, initial complaints, detailed features of rash and other findings of physical examination, laboratory findings and developments during follow-up were considered. For this purpose, a dedicated form permitting to enter the clinical and laboratory data, daily evaluation, and follow-up notes form was prepared. Clinical diagnosis was confirmed with necessary tests and response to the treatment if any was observed. The treatment and follow-up of such patients of etiology other than infection were determined by consultation in the Departments of Internal Medicine and Dermatology.
Laboratory tests were done due to predicted diagnosis as a result of patient's history and physical examination. For infectious causes, serologic tests and necessary cultures were obtained if viral and bacterial diseases are suspected, respectively. For non-infectious causes, essential tests were performed, according to the presumed diagnosis and skin biopsy if needed. Serum samples were taken from the patients initially, and were kept in -21℃.
Patients were divided into three groups, including infectious causes, noninfectious causes and undiagnosed. At the end of the study, data about the history and physical examination were compared with that of biochemical results statistically by Chi-square test, Fischer's exact probability test and one way ANOVA test.
Of the 100 cases in the study, 55 were men and 45 were women; the mean age was 35 years (14~79 years). Of the patients with fever and rash, 49% were due to infectious causes, while 41% were due to noninfectious causes and 10 cases were undiagnosed. Distribution of cases is shown in Table 1. Based on the data of 100 patients in our study, 66 used any drug because of any underlying diseases, 1 had contact with the tick, and 5 had travel history. Seventy-four patients were hospitalized and 26 were followed as outpatients. Symptoms and signs of these patients were as follows; Symptoms: fatigue 64%, headache 42%, sore throat and cough 40%, myalgia 37%, arthralgia 30%, photophobia 18%, and diarrhea 9%. Signs: lymphadenopathy 37%, tonsillopharyngitis 24%, conjunctivitis 19%, hepatomegaly 16%, cardiac murmur 11%, splenomegaly 9%, abnormal lung oscultation and hypotension 8%, arthritis 7%, and confusion 3%.
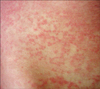
The types of rash in our series were as follows: macular 14%, maculopapular 34%, papule 7%, diffuse erythema 17%, purpura/ecchymosis 7%, nodule 2%, and polymorphic lesions 18%. Rash was accompanied by itching in 40 patients.
Mortality rate was 5%, despite the appropriate treatment. Diagnoses of these were adult onset Still's disease (ASD), graft-versus-host disease (GVHD), toxic shock syndrome (TSS) and toxic epidermal necrolysis (TEN) (2 cases).
The most common infectious causes were measles (12 cases), chickenpox (11 cases) and rickettsioses (8 cases). Confirmation of clinical diagnosis by serologic tests was available for 11 of 12 measles, 6 of 9 chickenpox and 5 of 6 rickettsial cases. TSS was found as the fourth most frequent etiology among the infectious causes. Three out of 4 patients were women. These patients had erythema and desquamation started from hands and feet after improving of the rash. Erysipelas, infectious mononucleosis and rubella were present in 3 cases each. All 3 cases with erysipelas had an erythema, which was clearly limited, bright, hot, and having a diameter varying from 10 to 20 cm. Two cases had adenopathy in the related lymphatic region. Infectious mononucleosis cases were 2 women and a man, having an age interval of 16~29 years. Two of them had macular and one had urticerial rash. All three experienced itching. Rash of the 2 cases developed after using amoxicilline for tonsillitis (Fig. 1). All of them had cervical lymphadenopathy and atypical lymphocytes in peripheral blood smear. Rubella was present in 3 men; maculopapular lesions were observed mostly in the trunk, and they had cervical and preauricular lymphadenopathies. Other 7 infectious diseases were represented in our series with one case each.
Drug reactions were the most common etiology among non-infectious causes. Among the Stevens-Johnson syndrome (SJS) and TEN cases, antibiotics and antiepileptics were the most common drugs (Table 2). In 2 cases, the diagnosis of TEN was confirmed with skin biopsy, and both died. Another patient developed purpura fulminans after propylthiouracil use (Fig. 2). Among the noninfectious causes, second largest group was connective tissue diseases. The highest numbers accounted ASD. All 8 cases had a common feature of emergence of rash with fever and disappearing with decreasing of fever. Other than fatigue and myalgia, 4 had sore throat, 3 had arthritis, lymphadenopathy, 2 had hepatomegaly and 1 had splenomegaly. The diagnosis was established by criteria of Cush et al.1. Acute renal failure developed in 1 patient, who then died of multiple organ failure in the intensive care unit.
Small vessel vasculitis was found in 5 patients in our series after drug reactions and connective tissue diseases. Three of them were diagnosed as Henoch Schönlein purpura (HSP). They had palpable purpuras, especially on gluteal region and extremities. Two patients' skin biopsies were reported as leukocytoclastic vasculitis. Similarly, other 2 cases of small vessel vasculitis were also reported as leukocytoclastic vasculitis. One patient had diffuse palpable purpuras, while another patient had acral cyanosis, accompanying vasculitic bullous lesions. Three women with an age range of 22~41 years were followed as urticeria. Two of them had itching and maculopapular, and one of them had erythematous rash. One of the 3 diseases, which were presented with one patient each in noninfectious causes of our series, was GVHD due to blood transfusion. He had oral mucositis accompanying maculopapular and bullous rashes with positive Nikolsky's sign and desquamation, thereafter. Skin biopsy confirmed the diagnosis; the patient died during follow-up in intensive care unit. A 63-year-old man had nodular, pustular and painful lesions on an erythematous background. He had high erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and leukocytes. Skin biopsy was reported as Sweet's syndrome. No hematologic disease was found. There were 2 patients with erythema nodosum: one was confirmed to have sarcoidosis and the other patient was diagnosed as primary erythema nodosum.
A 27-year-old man was presented with ulcerative colitis, fever, diarrhea and ulcerative, vesiculobullose lesions in various parts of his body. He was diagnosed as attack of ulcerative colitis and pyoderma gangrenosum, and was found to have mild leukocytosis, elevated alanine aminotransferase (ALT), ESR and CRP. Cultures of tissue and blood were negative (Fig. 3).
Undiagnosed cases, with an age range of 16~70 years, consisted of 4 men and 6 women. Clinical, radiologic and microbiological tests were noncontributory. Clinical follow-up established no spesific diagnosis. Rash and fever disappeared without any treatment.
For an easy approach to differential diagnosis, medical history, physical examination and biochemical results of the 3 groups were compared and shown in Table 3. Headache (p=0.012) and conjunctivitis (p=0.011) were significant in infectious causes, while drug use (p=0.010) and arthritis (p=0.037) were significant in non-infectious causes. Accompanying sore throat/pharyngitis was determined, especially in measles, IMN and ASD; conjunctivitis in measles and TSS; lymphadenopathy in measles, chickenpox and drug-related rash; arthralgia/arthritis in rickettsial infection, adult Still's disease and drug-related rash. Enanthem was observed in measles and SJS; itching in chickenpox, IMN and urticeria; desquamation in TSS and TEN; hand/foot involvement in rickettsial infection.
Among the laboratory findings, elevation of ESR, lower than 50 mm/hr, was observed in 80% of infectious causes, 55% of noninfectious causes and 83% of undiagnosed group. Nearly 45~60% of all 3 groups had elevation of CRP higher than 10 times, most commonly seen in ASD, HSP, TSS, rickettsial infection and SJS. Leukocytosis was more seen in ASD; IMN and TSS, while leukopenia in measles and TEN. Nine percent of our cases had eosinophilia (≥500/mm3), but there was no significant difference when the three groups were compared (p=0.575). Reasons for fever and rash in eosinophilic patients were usually drug reaction and TSS.
Patients with fever and rash are a diagnostic challenge for the physician. The disorder can be classified according to the severity of the disease (life-threatening or not), to the etiology (infectious and noninfectious), to the microorganism (bacterial, viral, fungal, parazitic), and to the type of rash (petechial, urticerial, erythematous, vesiculobullose, maculopapular, etc.). Although there are case series, studies similar to the current one are lacking. Etiology of fever and rash in 100 patients was 50% infections, 40% noninfectious causes and 10% undiagnosed. The most common infectious causes were measles, chickenpox, rickettsial infection and toxic shock syndrome, while drug reactions and connective tissue diseases were the most common among the noninfectious causes. The most common rash was maculopapular type with a rate of 34%. One fourth (1/4) of patients had also mucosal involvement. Enanthem was mostly present in measles. Infectious group had headache and conjunctivitis more frequently, while noninfectious group had arthritis.
When we compared the three groups, no significant difference was determined among the laboratory findings. However, elevations of ESR and CRP were lower in the viral causes, considering that the infections were divided into two groups, such as viral and bacterial.
Measles is the most common viral disease in our study. Nine of 12 cases (ages: 18~29 years), stated that they had been vaccinated during childhood. Headache, sore throat, cough, and conjunctivitis were striking features besides fever and rash. The frequency of Koplik's spot, patognomonic for measles, is 67% in our study. Leukopenia is observed in half (50%) of our cases. In our series, 90% and 82% of our patients had high AST and ALT levels, respectively.
Chickenpox was detected in 11 cases in our series. Cough (55%) and lymphadenopathy (64%) were striking findings among the patients' complaints and physical examinations. Itching was mostly seen in urticeria, IMN and chickenpox. One of the patients with cough was diagnosed as varicella pneumonia because of bilateral lung infiltrations.
Drug related rash was observed in 12 cases in our study. Frequency of skin reactions after using the drug is 0~8% for community and 2~3% for hospitalized patients. Drug related rash is usually maculopapular (30~50%)2. Drugs considered to be responsible are antibiotics, anticonvulsants and nonsteroid antiinflammatory drugs3. In the study of Sharma et al.4 34.6% of 500 cases had maculopapular rash and the most causative drug was anticonvulsant (41.6%)4. Six of our 12 cases had maculopapular rash, and 4 of these had used antibiotics. Differences were observed among antibiotic groups, according to the race and region. Rash due to penicillin and cephalosporin was much more frequently observed than the other groups. Frequency of skin reaction is reported as 1~3% in cephalosporin group5. Moreover, arthralgia and lymphadenopathy were more common in patients who developed drug-related rash. Drugs are responsible for 50% cases of SJS, while this is more than 80% for TEN3. Two TEN cases of our study had used levofloxacin and metoprolol, one of 2 SJS cases had used phenytoin and the other had used antimicrobials (ceftriaxone and levofloxacin together). In our study, SJS cases improved while 2 TEN cases died.
Mediterranen spotted fever is an endemic rickettsial infection, observed in our country, South Europe, Asia, North and South Africa6. Especially, at the summer and spring time, it is infected by tick bite and 30~90% of cases have diagnostic black spot (tache noire) at the inoculation site, which should remind us if the patient also has fever, headache and rash. We have 8 rickettsial cases in our study.
Our cases with ASD were presented with fever, rash and arthritis/arthralgia. They were diagnosed according to the criteria of Cush et al.1: one major and 2 minor criteria are essential for diagnosis. Major diagnostic criteria are fever (≥39℃), arthralgia or arthritis, negative romatoid factor, and negative antinuclear antibody. Minor criteria are leukocytosis, spesific rash for ASD, pleuritis or pericarditis, hepatomegaly or splenomegaly or systemic lymphadenopathy. Rash accompanying fever and regression of rash with decreasing fever are quiet important diagnostic clues, spesific for our ASD cases.
Another disease causing fever and rash in our study was TSS with serious morbidity and mortality. Staphylococcal TSS is a systemic illness, which developes due to infection or colonization with toxin producing Staphylococcus aureus7. Streptococcal TSS is caused by toxin of Group A Streptococcus8. We had 4 cases: One was streptococcal and three of them were staphylococcal. One staphylococcal TSS case died in our study.
Our 10 patients with fever and rash remained undiagnosed. Rash of undiagnosed patients were various types, such as macular (3/10), maculopapular (3/10), papular (2/10) and erythematous (2/10). There was no striking finding of complaints, physical examination and laboratory tests. No diagnosis was determined as a result of investigations, according to the clinical features of patients. All these cases showed improvements.
To conclude, adult patients with fever and rash had a wide differential diagnosis. The most common type of rash was determined as maculopapular and the most frequent 5 diseases were measles, drug reactions, chickenpox, ASD and rickettsial infection. Viral diseases among the infectious causes and drug reactions among the noninfectious causes were determined as the first etiology that should be remembered for fever and rash of adults.
References
1. Cush JJ, Medsger TA Jr, Christy WC, Herbert DC, Cooperstein LA. Adult-onset Stills disease. Clinical course and outcome. Arthritis Rheum. 1987. 30:186–194.
2. Babu KS, Belgi G. Management of cutaneous drug reactions. Curr Allergy Asthma Rep. 2002. 2:26–33.

3. Bachot N, Roujeau JC. Differential diagnosis of severe cutaneous drug eruptions. Am J Clin Dermatol. 2003. 4:561–572.

4. Sharma VK, Sethuraman G, Kumar B. Cutaneous adverse drug reactions: clinical pattern and causative agents--a 6 year series from Chandigarh, India. J Postgrad Med. 2001. 47:95–99.
6. Lucchina LC, Wilson ME, Drake LA. Dermatology and the recently returned traveler: infectious diseases with dermatologic manifestations. Int J Dermatol. 1997. 36:167–181.

7. Todd J, Fishaut M, Kapral F, Welch T. Toxic-shock syndrome associated with phage-group-I Staphylococci. Lancet. 1978. 2:1116–1118.

8. The Working Group on Severe Streptococcal Infections. Defining the group A streptococcal toxic shock syndrome. Rationale and consensus definition. JAMA. 1993. 269:390–391.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download