Comment on "Pseudopautrier's Abscess"
Dear Editor:
We read with great interest the article by Lee et al.1 entitled "The three dimensional conformal radiotherapy for hyperkeratotic plantar mycosis fungoides"1. We agree with the effectiveness of three-dimensional conformal radiotherapy for hyperkeratotic plantar mycosis fungoides (MF) and appreciate the educational figures. However, in this case report, the authors have described "the presence of intraepidermal collections of mononuclear cells showing hyperchromatic atypical cells that were compatible with Pautrier's microabscesses (PA)". We would like to suggest intraepidermal mononuclear collections described by the authors are not consistent with PA, but with pseudopautrier abscesses (PPA), regarded as a marker of spongiotic processs.
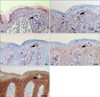
PA are one of the pathologic hallmarks of MF. They represent "punch-out" spaces in the epidermis filled with malignant T-lymphocytes (sometimes cerebriform). The aggregates of clonal T cells around Langerhans' cells explain the dependence of the T cells on interactions with these dendritic cells, particularly in the early stages of the disease2. PPA were first described as spongiotic stimulants of PA by Ackerman et al.3 in 1974. They consist of Langerhans cells, histiocytes, stellate keratinocytes and rare lymphocytes. In one study by Candiago et al.4, they were found in a variety of inflammatory disorders showing epidermal spongiosis, and were particularly frequent in spongiotic (43.4%), in lichenoid dermatitis (10%), and notably in MF (13.3%). Moreover, according to Kang et al.5, PPA were expressed in up to 25.5% of MF (24/94). They emphasize that the differential diagnostic hallmarks between PPA and PA are morphology, cell types, and particularly additional immunohistochemical findings, as shown in Fig. 1, 2.
Histologic findings considered as PA by Lee et al.1 favor more PPA, judging from adjacent prominent spongiosis, and predominance of nonlymphoid cells, showing presence of histiocyte, Langerhans cell, and stellate keratinocyte without atypical features. Additional immunohistochemical study will be also useful in the differential diagnosis, using CD1a, CD3, CD4, CD68, and high molecular cytokeratin5.
PPA are not an infrequent histologic finding in MF, particularly more common with MF palmaris et plantaris referring to the hyperkeratotic MF5. Thus, it is not suitable to exclude the diagnosis of MF unquestionably, when PPA are seen in biopsy specimen. In addition, when collections of intraepidermal mononuclear cells are observed in typical MF, the clinician should be cautious before concluding they are PA, and a careful histological and immunohistochemical evaluation must be performed carefully to distinguish PPA from PA.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download