Abstract
Pigmentary demarcation lines are abrupt transition lines between the areas of deeper pigmentation and the areas of lighter, normal pigmentation. Type B pigmentary demarcation lines involve the posterior medial portion of the lower extremities and are more commonly associated with pregnancy. We present a case of pigmentary demarcation lines of pregnancy with erythematous changes, involving both the anterior and posterior aspects of the lower extremities.
Pigmentary demarcation lines (PDLs) are abrupt transition lines between the areas of deeper pigmentation and the areas of lighter, normal pigmentation. They are classified into 5 groups, based on their locations; type A involving the lateral aspect of the upper anterior arms; type B involving the posteromedial portion of the lower extremities; type C involving the hypopigmented lines in pre- and parasternal areas; type D involving the posteromedial area of the spine; and type E involving the bilateral hypopigmented bands on the chest1. Recently, it was suggested that these lines may occur on the face, and additional categories F, G, and H have been suggested2. Type B PDLs are more commonly associated with pregnancy, and are mostly known to occur after the seventh month of pregnancy3. We present a case of type B PDLs of pregnancy, with three interesting main features: 1) a relatively early onset at the end of the fourth month of pregnancy, 2) association of erythematous changes, and 3) unique distribution, involving both the anterior and the posterior aspects of the lower extremities. To our knowledge, this is the first case of type B PDLs, involving not only the posterior portion of the lower extremities, but also the anterior thighs and knees.
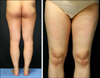
A 32-year-old primigravida presented with asymptomatic, erythematous, pigmented patches on her lower extremities, which developed around the 18th week of her pregnancy. Initially, she visited an obstetrician, and was later referred to our dermatology clinic for the cutaneous lesions. She had been diagnosed with stage 1E mantle cell lymphoma of the left conjunctiva two years ago, and was in complete remission after receiving chemotherapy of cyclophosphamide, doxorubicin, vincristine, and prednisolone. There was no family history of abnormal cutaneous pigmentation. At the 17th week of her pregnancy, serum unconjugate estriol (E3) level was investigated, as a part of the fetal screening. Unconjugate E3 was 1.475 multiples of the median (MoM), indicating a higher level than the median value, but within the normal range. Other laboratory results were within normal limits. The cutaneous examination revealed bilateral, symmetrical, well-demarcated, erythematous pigmented patches, from the buttocks down to the popliteal fossae, and also on the anterior thighs and knees (Fig. 1). The lesions had clear boundaries between the hyperpigmentation and adjacent normal skin. Histopathologic examination showed basal layer pigmentation and dilation of the small vessels with perivascular lymphohistiocytic infiltration in the upper dermis (Fig. 2). The spontaneous fading or disappearance of the pigmentation after delivery in most cases of PDLs of pregnancy was explained, and the patient was reassured and advised on the expectant observation. A day after delivery, the erythema had disappeared, spontaneously. Three weeks after delivery, the lines had mostly faded (Fig. 3).
The cause of PDLs during pregnancy is unknown. Hormonal alterations, regarding estrogen, progesterone, and melanocyte-stimulating hormone (MSH), can be considered. The inciting factors of the pigmentary changes in the pregnancy include fetoplacental hormone production or alterations in clearance, which may increase the plasma availability of hormones, such as estrogens and progesterone4. In addition, plasma levels of MSH become significantly elevated by the 8 weeks' gestation, presumably as a result of enlargement of the intermediate lobe of the pituitary gland. Moreover, the production of pro-opiomelanocortin, a source of - and - MSH, has been shown in placental extracts5. The role of hormonal alterations in PDLs is further supported by the report of a nonpregnant woman with type B PDLs, receiving long-term estrogenic medication6. An amenorrheic woman with type B PDLs and decreased titers of estradiol and elevated levels of follicle-stimulating hormone has also been reported7. In the latter case, the hormonal changes were different from the changes in sex hormones during pregnancy. However, there still may be a relationship between abnormal levels of sex hormones and PDLs. Our patient exhibited erythematous changes, in addition to the pigmentation, and histopathologic findings showed dilated vessels in the upper dermis. Estrogen-induced changes in small blood vessels occur during pregnancy, and the blood vessels are found to be widely dilated in the superficial dermis. The erythematous changes in our patient may have resulted from the alteration of estrogen levels in pregnancy. Compression of peripheral nerves emerging from S1 and S2 levels by the enlarged uterus and resulting erythema, pigmentation from neurogenic inflammation has also been suggested8. However, PDLs are not associated with specific symptoms. Furthermore, the involved areas of the anterior thighs and knees in our case do not correspond to the innervation of S1 and S2. To our knowledge, there have been two reports on PDLs with erythematous changes3,8. Mild basal layer pigmentation was observed in previous reports of PDLs that examined the biopsies, histopathologically8.
PDLs are asymptomatic, and therefore, may be overlooked by patients and physicians. Obstetricians, as well as dermatologists, should be aware of this pregnancy-related condition.
Figures and Tables
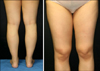 | Fig. 1Bilateral, symmetrical, well-demarcated, erythematous pigmented patches from the buttocks down to the popliteal fossae, the anterior thighs, and knees. |
References
1. Miura O. On the demarcation lines of pigmentation observed among the Japanese, on inner sides of their extremities and on anterior and posterior sides of their medial regions. Tohoku J Exp Med. 1951. 54:135–140.

2. Somani VK, Razvi F, Sita VN. Pigmentary demarcation lines over the face. Indian J Dermatol Venereol Leprol. 2004. 70:336–341.

3. Nakama T, Hashikawa K, Higuchi M, Ishii N, Miyasato M, Hamada T, et al. Pigmentary demarcation lines associated with pregnancy. Clin Exp Dermatol. 2009. 34:e573–e576.
4. Kanda N, Watanabe S. Regulatory roles of sex hormones in cutaneous biology and immunology. J Dermatol Sci. 2005. 38:1–7.
5. Bicknell AB. The tissue-specific processing of pro-opiomelanocortin. J Neuroendocrinol. 2008. 20:692–699.

6. Delmonte S, Parodi A, Rebora A. Pigmentary demarcation lines type B in a white non-pregnant woman. Acta Derm Venereol. 1997. 77:82.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download