Abstract
Background
Skin acts as the first line of defense against any foreign materials outside of our body. In inflammatory skin disease, the pathogenesis is due to an immune reaction in the keratinocytes, immune cells and soluble mediators. Balneotherapy is widely used for the treatment of inflammatory skin disease, but the mechanisms are only partly understood by immune regulation. Balneotherapy in dermatologic disease can affect the secretion of pro-inflammatory cytokines, IL-1α and tumor necrosis factor from keratinocytes, and possibly affect the T cell differentiation.
Objective
In this study, we evaluated the effect of spa spring water from Yong-gung oncheon on the cells, and investigated the skin immune reaction.
Methods
We investigated the immunomodulatory or anti-inflammatory effect of thermal spring water on the expression of pro-inflammatory cytokines in the HaCaT cells under Toll-like receptor (TLR) stimulation, as well as the effect on the differentiation of CD4+ T cells under spring water.
Results
The treatment of spa spring water from Yong-gung oncheon decreased the expression of proinflammatory cytokines under TLR stimulation to the HaCaT cells and antigen presenting cells. In addition, spa spring water attenuated the differentiation process of subsets of CD4+ T cells, i.e., Th1, Th2 and Th17 cells. All these immune parameters can be used to evaluate the efficacy of spa spring water in Korea, in terms of the immune modulatory effect.
Skin contributes to the first line of defense against any foreign materials outside of our body, as a physical barrier. As immune sentinels, keratinocytes can recognize foreign or danger stimuli from the outside via pattern-recognition receptors, such as Toll-like receptors (TLRs), and release innate immune mediators, including cytokines and chemokines, under the stimulation of the keratinocytes. Epidermal keratinocytes express several TLRs, including TLR1, TLR2, TLR3, TLR4, TLR5, TLR6, TLR7 and TLR91, and through the TLRs, keratinocytes initiate and promote immune responses in the skin.
For inflammatory skin disease, pathogenesis is due to the sum of the immune reactions of the keratinocytes, immune cells and soluble mediators. The three main types of CD4+ T cells can be found in the skin during inflammatory skin disease, i.e., Th1, Th2 and Th17. For example, Th1-dominant immune reactions were reported to be associated with the autoimmunity or psoriasis, and Th2-dominant responses were related to that of asthma or atopic dermatitis. The Th17 cells were reported to contribute to defend against various fungal or bacterial infections, and possibly induced atopic dermatitis and epidermal changes in psoriasis2,3 via secretion of interleukin (IL)-17 and IL-22. IL-17 and IL-22 increased antimicrobial peptides, β-defensins and cathelicidins, from keratinocytes4. In addition to the antimicrobial peptides, keratinocytes secrete cytokines, including IL-1, IL-6, IL-10, IL-18 and tumor necrosis factor (TNF)5.
Spa therapy is widely used for the treatment of inflammatory skin diseases, such as atopic dermatitis, psoriasis, pruritus, rosacea, seborrheic dermatitis and others6. The efficacy of spa therapy for inflammatory skin diseases and the mechanisms are only partly understood, and presumably incorporate chemical, thermal, mechanical and immunomodulatory effects7,8. Among them, we investigated the immunomodulatory or anti-inflammatory effect of thermal spring water on the expression of pro-inflammatory cytokines in the HaCaT cells under TLR stimulation, as well as the effect on differentiation of CD4+ T cells under spring water.
HaCaT (human keratinocyte cell line) was kindly provided by Dr. Tae-Yoon Kim (College of Medicine, The Catholic University of Korea) and was cultured in Dulbeco's Modified Eagle Medium (DMEM, Gibco-BRL, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS, Gibco- BRL) and 100 U/ml penicillin/streptomycin (Gibco- BRL), at 37℃ in an incubator containing 5% CO2.
Water was collected from the Yong-gung oncheon (Incheon-si, Gangwha-gun, Korea) spring and filtered through 0.44 um filters. Waters were stored at 4℃, until used for the experiments. For the measurement of water osmolarity, we used a Micro-Osmometer 210 (FISKE Associate, Norwood, MA, USA).
For the 3-(4,5-dimethylthizol-2-yl) 2,5-diphenyl tetrazolium bromide (MTT, Sigma-Aldrich, St. Louis, MO, USA) assay, cells were plated onto 96-well microtiter plates at a density of 3×104/200 µl in fresh medium, and then treated with hot spring water at a serially diluted concentration. Cells were cultured for 1, 4, 10, and 24 hours, respectively, to observe a time dependent effect. After the indicated time, 20 µl of MTT (5 mg/ml in phosphate-buffered saline) was added to each well, and the plates were returned to the incubator for an additional 4 hours. At the end of the incubation period, the supernatants were discarded by a suction and 200 µl dimethyl sulfoxide was added to all the wells, in order to dissolve the dark blue formazan crystals. The plates were subsequently covered with aluminum foil, gently shaken for 15 minutes, and read at a wavelength of 570 nm.
TLR agonists were treated with the following final concentrations for 24 hours. Tripamitoyl-S-glyceryl-cysteine (Pam3Cys, 1 µl/ml), heat-killed Listeria monocytogenes (HKLM, 106 cells/ml), polyriboinosinic polyribocytidylic acid (poly (I : C), 10 µl/ml), lipopolysaccharide (LPS, 10 µl/ml), flagellin (10 µl/ml), and Pam2CGDPKHPKSF (FSL-1, 1 µl/m) were from InvivoGen (San Diego, CA, USA). Spa spring waters were added simultaneously or pre-treated 2 hours before the TLR agonist treatment. Cells were cultured for 1, 4, 10, or 24 hours in each treatment group.
Levels of IL-6, IL-8, granulocyte-macrophage colony-stimulating factor (GM-CSF), and TNF-α (BD OptEIA™, BD Biosciences Pharmingen, San Diego, CA, USA), IL-1α (Biolegend, San Diego, CA, USA) in HaCaT supernatant treated with TLR agonist in the presence or absence of hot spring water were quantified according to the manufacturer's protocol. IL-6 and TNF-α in mouse antigen presenting cells (APC) supernatant were also measured. In brief, the wells were coated with 100 µl of capture antibody in coating buffer (0.1 M sodium carbonate, pH 9.5) and the plates were incubated overnight at 4℃. After washing the wells with washing buffer (phosphate buffered saline [PBS] with 0.05% Tween-20), the wells were blocked with assay diluents (10% FBS in PBS) for 1 hour at room temperature (RT), followed by the addition of 100 µl/well of cell supernatant and cytokine standard solutions for 2 hours at RT. After washing, 100 µl of detection antibody and streptavidin-conjugated horseradish peroxidase reagent were added to the wells, which was then incubated for 1 hour at RT. After extensive washing, 100 µl of substrate solution (tetramethylbenzidine and hydrogen peroxide, BD Biosciences Pharmingen) was added to each well and the plates were incubated for 30 minutes at RT, in darkness. Stop solutions (2 N H2SO4) were added, and the absorbance was read at 450 nm within 30 minutes.
Naïve CD4+ T cells were purified from the mouse spleens, via magnetic isolation (Miltenyi Biotec GmbH, Gladbach, Germany). For the preparation of the spleen cell suspensions, spleens from 8 weeks-old female Balb/c mice were removed and minced with a Nylon mesh (70 µm pore). After the cells were pelleted, erythrocytes were lysed using hypotonic buffer (0.15 M NH4Cl, 10 mM KHCO3, 0.1 mM Na2EDTA). The cells were washed in PBS and incubated with anti-CD4 antibody for 15 minutes, at 4℃. Directly following, the cells were conducted onto a magnetic separator to isolate the CD4+ cells and collected with positive selection. CD4- cells were seeded onto a culture dish of 100 mm in diameter and incubated for 4 hours for the collection of the adherent cells (used as APC in these experiments) by gentle pipetting.
CD4+ naïve cells were seeded at a density of 2×105 per well in 96-well plates, and were cultured in DMEM, containing 10% FBS. For each of the helper T cell differentiation, the skewing conditions are as followed; IL-12 (25 ng/ml, Biolegend) and anti-CD28 (1 µg/ml, Biolegend) for Th1, IL-4 (25 ng/ml, Biolegend) and anti-CD28 (1 µg/ml, Biolegend) for Th2, IL-6 (25 ng/ml, Biolegend), transforming growth factor (TGF)-β (2 ng/ml, R&D system) and anti-CD28 (1 µg/ml, Biolegend) for Th17, IL-2 (25 ng/ml, Biolegend) and anti-CD28 (1 µg/ml, Biolegend) for T reg. All cells stimulated with anti-CD3 antibodies with serial dilutions, in which the initial concentration was 3 µg/ml. Cells were incubated for 3 days in the presence or absence of spa spring water.
Before seeding for the differentiation of each of the helper T cell differentiation, the CD4+ cells were labeled with carboxyfluorescein diacetate, succinimidyl ester (CFSE, CellTrace™ CFSE Cell Prolifetration kit, Invitrogen, Paisley, UK). First, the cells were resuspended in prewarmed PBS/0.1% bovine serum albumin, at a concentration of 106 cells/ml, and 10 µM of CFSE were added. After incubation at 37℃ for 10 minutes, 5 volumes of ice-cold culture media was added to the cells to quench the staining, incubated for 5 minutes on ice, and pelleted by centrifugation. The cells were resuspended in fresh media for a total of three washes, and seeded under each condition for the differentiation of Th1, Th2, Th17, and Treg cells. After 3 days, CD4+ and CFSE+ cells were measured for the degree of proliferation, via a flow cytometry, and were analyzed using ModFit LT software (Verity Software House, Topsham, ME, USA), based on the reduction of CFSE positive cells.
APCs were stimulated with TLR3 agonist, poly (I : C) (10 µg/ml) for 24 hours with or without spa spring waters. APCs stimulated with poly (I : C) with or without hot spring water were collected, washed and stained with anti-mouse I-A/I-E (Biolegend, clone M5/114.15.2, Rat IgG2b, κ) to analyze the expression of MHC II on the surface of APCs for 20 minutes, at RT. Samples were acquired on FACSCalibur system (BD Bioscience, San Jose, CA, USA) and were analyzed using CellQuest software (BD Bioscience).
Because the osmolarity of spa spring water from Yong-gung oncheon was 700 mOsm/kg, the HaCaT cells were not able to maintain the growth in undiluted culture medium (Fig. 1). Therefore, we first determined to set an optimal dilution concentration for HaCaT culture conditions by the MTT assay. For this, HaCaT cells were cultured with spa spring water at a concentration of serially 2-fold dilution for 1, 4, 10, and 24 hours and the minimum concentration of spa spring water was determined. We found that each group of cells was up to 100% of viability under a 1 : 32 fold dilution (Fig. 2).
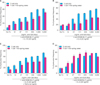
TLRs act as primary sensors that detect a wide variety of microbial components and elicit innate immune response, which guides the acquired immunity. Therefore, keratinocyte constitutively expressing TLRs may affect skin immune response, by regulating the inflammatory responses, via TLR signaling. We attempted to determine whether the spa spring water affected the TLR stimulated production of pro-inflammatory cytokines, including IL-1α, IL-6, IL-8, TNF-α, and GM-CSF, on the HaCaT cells. TLR1 agonist, through TLR6 agonist treatment, induced the attenuation of cytokine production in the exposure to spa spring in advance or simultaneously with TLR agonist treatment (Fig. 3, 4).
We subsequently attempted to ascertain the potential involvement of spa spring water in the differentiation of the helper T cells. Because the effector T cells, such as Th1, Th2, and Th17 cells act on various skin resident cells and potentiate the immune reaction, regulating T cell differentiation may modulate pro-inflammatory responses. To evaluate the in vitro suppressive capacity of spa spring water toward the helper T cell differentiation, magnetic sorted CD4+ T cells, from the spleen, were prepared from Balb/c mice. CFSE-labeled CD4+ T cells were cultured under various conditions, which polarized Th1, Th2, Th17, and Treg with or without spa spring water. After 3 days, the cells were harvested and stained with CD4 and interferon (IFN)-γ for Th1, IL-4 for Th2, IL-17 for Th17 and Foxp3 for Treg cells, respectively. Then, the flow cytometry was employed to evaluate the precursor frequency in terms of the T cell differentiation. As shown in Fig. 5, CD4+ naïve T cells were profoundly proliferated and differentiated under each skewing condition, along with anti-CD3 stimulation. Spa spring water suppressed the proliferation of Th1, Th2 and Th17 cells. In contrast to the suppressive effect on Th1, Th2 and Th17 cells, proliferation and differentiation to Treg cells were promoted under spa spring water treatment. These results indicate that spa spring water may affect the distribution of the helper T cells in the immune response, by suppressing the polarization of the Th1, Th2 or Th17 cells.
Skin immunity is achieved by an interaction of different kinds of immune cells. In particular, APCs, such as Langerhans cells found in the epidermis, are the best-characterized dendritic cell population. They have the ability to process antigens in the periphery, transport it to the draining lymph nodes, where they are able to cluster with, and activate the antigen-specific naive T cells. APCs in the dermis may also provide alternative routes of antigen presentation, which can be important in the regulation of skin immune responses. Therefore, APCs are vital for the induction of immune responses to antigens encountered via the skin. To determine whether the expression of MHC II on the surface of APC is modulated by spa spring water, we isolated APC from BALB/C mouse spleen, and stimulated it with 20 µg/ml of poly (I : C) for 24 hours. TLR3 stimulation via poly (I : C) strongly induced MHC II expression on the APCs. By contrasts, APC treated spa spring water down-regulated the surface level of class II MHC expression, under TLR 3 stimulation (Fig. 6A). In addition, we observed that TLR3 agonist, poly (I : C) is a very potent inducer of inflammatory responses in the HaCaT cells9. Therefore, we measured and compared poly (I : C) mediated production of inflammatory cytokines from the APCs with or without spa spring water (Fig. 6B, C). APC induced TNF-α and IL-6 under poly (I : C) stimulation and cytokine production was reduced in the presence of spa spring water. These results showed that TLR-triggered inflammatory responses in APCs might also be modulated under spa spring water treatment.
In this study, we evaluated the effect of spa spring water from Yong-gung oncheon on cells related to the skin immune reaction. The treatment of spa spring water from Yong-gung oncheon decreased the expression of proinflammatory cytokines under TLR stimulation to the HaCaT cells and APCs. In addition, spa spring water attenuated the differentiation process of subsets of T helper cells, i.e., Th1, Th2 and Th17 cells.
The therapeutic mechanism of spa spring water in dermatologic diseases can be divided into three categories: active ingredient, thermal effects and mechanical effects. Minerals in spa spring water, such as sulfur, magnesium, calcium or selenium induce anti-inflammatory, keratolytic, antibacterial or antifungal effects6. For anti-inflammatory effects, the inhibition of Th1 differentiation, inhibition of cytokine production from keratinocytes, and modulatory effects on epidermal Langerhans cells have been reported10. In this study, we observed the significant inhibitory effect on the secretion of pro-inflammatory cytokines, including IL-6, IL-8, IL-1α, TNFα and GM-CSF from keratinocytes (Fig. 4). In addition, we observed the differentiation of Th1, Th2, or Th17, but not of Foxp3+ Treg cells under the treatment with water from Yong-gung oncheon (Fig. 5).
Th17 cells are related to the autoimmunity or inflammatory skin disease, such as psoriasis or atopic dermatitis via IL-17 and IL-22 secretion. IL-17 acts directly on keratinocytes and induces the production of MIP-3α, IL-8 and β-defensin, whereas, IL-22 regulates the keratinocyte differentiation11,12. In addition, IL-17 promotes the neutrophil recruitment by inducing the neutrophil-attracting chemokines (CXCL1, CXCL2, CXCL5, and CXCL8) and stimulates neutrophil production by inducing granulopoiesis factors (G-CSF or GM-CSF)13. In case of Staphylococcus aureus infection, the role of Th17 was reported to be critical: in mice bacterial clearance was impaired in IL-17R-deficient mice, and in human hyper immunoglobulin E syndrome, atopic dermatitis, human immunodeficiency virus/acquired immune deficiency syndrome or mucocutaneous candidiasis, in which there is a common deficiency of Th17 cells. These IL-17-mediated defenses against S. aureus infection are involved with promotion of neutrophil recruitment via cytokines, chemokines or adhesion molecules and production of antimicrobial peptides. In this context, reduced Th17 cell differentiation, by spa spring water, implies that spa spring water may reduce the immune reaction in the epidermal layer, partly by affecting the antimicrobial peptide production and epidermal differentiation irrespective of antibacterial effect of IL-17.
Regulatory T cells (Treg cells) mediate immunosuppression and tolerogenic responses through contact-dependent or -independent mechanisms14-16. Foxp3+ Tregs produce IL-10 or TGF-β as effector molecules, and the balance between Treg cells and effector T cells is crucial for the maintenance of homeostasis and self-tolerance17. In this study, spa spring water from Yong-gung oncheon treatment induced Foxp3+ Treg cell differentiation in vitro, implying that the immune modulatory effect of spa spring water also includes Treg cell-induced immune suppressive effects.
TLRs are a type of pattern recognition receptor, which recognize microbial products known as pathogen-associated molecular patterns, i.e., bacterial lipoproteins, zymosan, LPS, flagellin, ssRNA, dsRNA, and unmethylated CpG DNA. TLRs are transmembrane receptors and present on the cell surface or on the surface of endosomal compartments. It was reported that TLR3 ligand poly (I : C) was the most potent stimulator of IL-8, IL-6 and TNFα secretion18 in the primary keratinocyte and HaCaT cell lines. In this experiment, we used TLR1 to TLR6 agonists to activate the HaCaT cells inducing pro-inflammatory cytokines. We observed that spa spring water treatment led to reduced IL-6, IL-8, TNF-α, IL-1α, and GM-CSF from the HaCaT cells, following TLR ligand treatments, and spa spring water from Yong-gung oncheon suppressed the expression of IL-6, TNF-α and class II MHC expression of APC in this experiment (Fig. 6). In case of atopic asthma, IL-5, IL-13, IL-1β, IFN-γ, IL-12, GM-CSF, IL-4, and IL-10 were elevated, compared with those of the non-atopic patients19. Further studies are required to compare the cytokine profile in non-atopic and atopic dermatitis patients after a spa treatment.
These results showed that spa spring water treatment suppressed the inflammatory cytokines production, and also modulated differentiation of CD4+ T cells into Th1, Th2, and Th17 cells, but not Tregs cells. With these experimental protocols, we can evaluate and compare the efficacy of spa spring waters in Korea, immunologically. Furthermore, we would define immune-active ingredient from this spa spring water to reveal immune modulatory mechanism of spa spring waters in Korea.
Figures and Tables
 | Fig. 1Cell culture with spa spring water led to detach HaCaT cells. The HaCaT cells cultured in Dulbeco's Modified Eagle Medium (DMEM, Gibco-BRL, Grand Island, NY, USA) with 10% fetal bovine serum (FBS, Gibco-BRL) (A) and DMEM prepared from undiluted spa spring water with 10% FBS (B). Original magnification ×200. Tx: Treatment. |
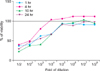 | Fig. 2Viability of HaCaT cells was not affected by spa spring water in the 1:32 fold of dilution. The HaCaT cells were plated at a density of 3×104/200 µl in fresh medium and treated with spa spring water as indicated. After 1, 4, 10, and 24 hours of culture, 20 µl of MTT (5 mg/ml in PBS) was added to each of the wells. After 4 hours, dark blue formazan crystals were dissolved, and the plates were read at a wavelength of 570 nm. 100% viability was determined based on the result of MTT assay of normally cultured HaCaT cells. PBS: peripheral blood smear examination. |
 | Fig. 3Schematic diagram of experimental design. (A) The HaCaT cells were pre-incubated for 2 hours with spa spring water at a concentration of 1 : 30 fold dilution, and then stimulated with TLR1 to TLR6 agonist as indicated time. (B) The HaCaT cells were simultaneously exposed to spa spring water and TLR agonist and incubated as indicated time. TLR: toll-like receptor. |
 | Fig. 4Spa spring water impairs pro-inflammatory cytokine production on HaCaT cells under TLR stimulation. The HaCaT cells were treated with TLR1 through TLR6 agonist for 1, 4, 10, and 24 hours, respectively. Spa spring water diluted 1 : 30 fold was added prior to adding TLR agonists or simultaneously. After the indicated time, the supernatants were collected to measure secreted level of IL-6 (A), IL-8 (B), TNF-α (C), IL-1α (D), and GM-CSF (E) via ELISA. The data are expressed as the means±SEM (*p<0.05) of three independent experiments. TLR: Toll-like receptor, IL: interleukin, HKLM: heat-killed Listeria monocytogenes, LPS: lipopolysaccharide, FSL1: Pam2CGDPKHPKSF, TNF: tumor necrosis factor, GM-CSF: granulocyte macrophage-colony stimulating factor, SEM: standard error of the mean. |
 | Fig. 5Spa spring water inhibited the differentiation and proliferation of effector T cells and promoted Treg proliferation. The CD4+ naïve T cells were isolated, labeled with carboxyfluorescein diacetate, succinimidyl ester (CFSE, CellTrace™ CFSE Cell Prolifetration kit, Invitrogen, Paisley, UK), and cultured under skewing conditions for Th1, Th2, Th17, and Treg cells, respectively, in the presence or absence of spa spring water. Serially diluted (1 : 3) anti-CD3 antibodies were treated at a concentration starting from 3 µg/ml to monitor dose-dependent proliferation. On day 3, cells were harvested and proliferation was measured by flow cytometry. CD4+ IFN-γ+ Th1 cells (A), CD4+ IL-4+ Th2 cells (B), and CD4+ IL-17+ Th17 cells (C) were proliferated along with the increase of anti-CD3 stimulation, whereas they were inhibited under spa spring water. In contrast, spa spring water promoted proliferation of CD4+Foxp3+ Tregs (D) relative to those of the HaCaT cells cultured alone. Percentages of proliferative cells were represented as precursor frequency via analysis using ModFit LT software (Verity Software House, Topsham, ME, USA) based on the reduction of CFSE positive cells. The data are expressed as the means±SEM (*p<0.05) from three independent experiments. Tx: treatment, IFN: interferon, IL: interleukin, TGF: transforming growth factor, SEM: standard error of the mean. |
 | Fig. 6Spa spring water decreased class II MHC expression and impaired pro-inflammatory cytokine production on APCs under TLR3 stimulation. APCs were isolated and stimulated with 20 µg/ml of poly (I : C) for 24 hours. (A) Class II MHC expression was increased under poly (I : C) treatment and significantly reduced by adding spa spring water. Expressed levels were represented by histogram (left) and quantified as MFI (right). Poly (I : C) induced IL-6 (B) and TNF-α (C) were attenuated under spa spring water treatment. The data are expressed as the means±SEM (*p<0.05) from three independent experiments. APC: antigen presenting cell, TLR: Toll-like receptor, Tx: treatment, MFI: mean fluorescence intensity, IL: interleukin, IFN: interferon, SEM: standard error of the mean. |
ACKNOWLEDGMENT
This work was partly supported by the Korean Academy of Hot Spring and the Basic Science Research Program though the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science, and Technology [NRF-2010-0003185] to S-Y. Woo.
This manuscript has been presented at the Korean Dermatological Association, the 63th Autumn Meeting.
References
1. Lebre MC, van der Aar AM, van Baarsen L, van Capel TM, Schuitemaker JH, Kapsenberg ML, et al. Human keratinocytes express functional Toll-like receptor 3, 4, 5, and 9. J Invest Dermatol. 2007. 127:331–341.

2. Di Cesare A, Di Meglio P, Nestle FO. The IL-23/Th17 axis in the immunopathogenesis of psoriasis. J Invest Dermatol. 2009. 129:1339–1350.

3. Di Cesare A, Di Meglio P, Nestle FO. A role for Th17 cells in the immunopathogenesis of atopic dermatitis? J Invest Dermatol. 2008. 128:2569–2571.

4. Liang SC, Tan XY, Luxenberg DP, Karim R, Dunussi-Joannopoulos K, Collins M, et al. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J Exp Med. 2006. 203:2271–2279.

5. Albanesi C, Scarponi C, Giustizieri ML, Girolomoni G. Keratinocytes in inflammatory skin diseases. Curr Drug Targets Inflamm Allergy. 2005. 4:329–334.

7. Valitutti S, Castellino F, Musiani P. Effect of sulfurous (thermal) water on T lymphocyte proliferative response. Ann Allergy. 1990. 65:463–468.
8. Celerier P, Richard A, Litoux P, Dreno B. Modulatory effects of selenium and strontium salts on keratinocyte-derived inflammatory cytokines. Arch Dermatol Res. 1995. 287:680–682.

9. Lee KH, Cho KA, Kim JY, Kim JY, Baek JH, Woo SY, et al. Filaggrin knockdown and Toll-like receptor 3 (TLR3) stimulation enhanced the production of thymic stromal lymphopoietin (TSLP) from epidermal layers. Exp Dermatol. 2011. 20:149–151.

10. Wiedow O, Streit V, Christophers E, Ständer M. Liberation of human leukocyte elastase by hypertonic saline baths in psoriasis. Hautarzt. 1989. 40:518–522.
11. Nograles KE, Zaba LC, Guttman-Yassky E, Fuentes-Duculan J, Suárez-Fariñas M, Cardinale I, et al. Th17 cytokines interleukin (IL)-17 and IL-22 modulate distinct inflammatory and keratinocyte-response pathways. Br J Dermatol. 2008. 159:1092–1102.

12. Boniface K, Bernard FX, Garcia M, Gurney AL, Lecron JC, Morel F. IL-22 inhibits epidermal differentiation and induces proinflammatory gene expression and migration of human keratinocytes. J Immunol. 2005. 174:3695–3702.

13. Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat Rev Immunol. 2010. 10:479–489.

14. Shevach EM. Mechanisms of foxp3+ T regulatory cell-mediated suppression. Immunity. 2009. 30:636–645.

15. Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat Rev Immunol. 2008. 8:523–532.

16. Tang Q, Bluestone JA. The Foxp3+ regulatory T cell: a jack of all trades, master of regulation. Nat Immunol. 2008. 9:239–244.

17. Wing K, Sakaguchi S. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol. 2010. 11:7–13.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download