Abstract
Background
The current modality of choice for the treatment of Port-wine stains (PWS) is laser photocoagulation. Laser therapy for the treatment of PWS, especially with a pulsed dye laser (PDL), has been proven safe and effective; however, because penetration of the PDL is too shallow for an effective ablation of the blebs, treatment of blebbed PWS, using PDL, may be insufficient.
Objective
We demonstrated the clinical efficacy of a 1,064 nm long pulsed Nd:YAG laser with contact cooling device for blebbed PWS.
Methods
Twenty one patients with blebbed PWS (Fitzpatrick skin types II-V) underwent a treatment, using a 1,064 nm long pulsed Nd:YAG laser with a contact cooling device at 8-week intervals. Treatments were done using 5~6 mm spot sizes at 20~30 ms and 95~170 J/cm2. Laser parameters were adjusted in order to meet the needs of each individual patient's lesions.
Port-wine stains (PWS) are present at birth. It is a congenital vascular malformations that composed of superficial collection of dilated vessels that grow commensurably with the child1. PWS may initially appear pale, erythematous macules or patches that darken in color with age. The surface of these patches may become raised and nodular, called blebs, especially as the individual ages.
Pulsed dye laser (PDL) has been a standard treatment modalities for PWS since the 1980s2. Early treatment of PWS lesions with smaller and thinner state, prior to their proportional growth with the child, may contribute to the high success rate of PDL treatment3; however, because the penetration of PDL exploiting wavelengths is too shallow for an effective ablation of the blebs, a significant proportion of blebbed PWS are resistant to PDL treatment. As an alternative, light source for PWS, a long-pulsed Nd:YAG laser penetrates deeply into the skin, and can be effective in the treatment of blebbed PWS. We demonstrate the clinical efficacy of a 1,064 nm long pulsed Nd:YAG laser, equipped with contact cooling device in the treatment of blebbed PWS.
Twenty-one healthy adult patients (11 male and 10 female) with Fitzpatrick skin types II-V, who ranged in age from 15 to 66 years (average, 45.64 years) with congenital PWS, underwent treatment for blebbed PWS. Nineteen patients had PWS lesions in a trigeminal location (V1~V3 distribution), and four patients had involvement of other sites (nose, neck, and trunk). In two cases, the treated lesions were spanned across the two anatomic sites. Six patients had received prior treatment for their vascular lesions, with an unsatisfactory results. Exclusion criteria included pregnancy, immunocompromised, and had past histories of hypertrophic scars or keloids.
Preliminary study was performed for the establishment and optimization of treatment parameters for specific wave-length combinations. Prior to performing this study, four successfully treated cases were published, as a case report, in the Annals of Dermatology (accepted for publication November, 2011). In addition, we attempted to apply and individualize these parameters to the heterogeneous types of vascular lesions, and to the large number of patients in this study.
A board-certified dermatologist delivered successive treatments, using a 1,064 nm long pulsed Nd:YAG laser with contact cooling device (COSJET SR®, Won Technology, Daejeon, Korea) at 8-week time intervals. Treatment energy densities varied between 95 J/cm2 and 170 J/cm2 with 20 ms to 30 ms pulse duration, and 5 mm to 6 mm spot size, depending on the location, size, depth, and color of the bleb within any given areas; surrounding flat lesions were treated with a additional 595 nm PDL (V beam perfecta®, Candela corp., Wayland, MA, USA) with 1.5 to 3 ms pulse duration, and 10 J/cm2 to 12 J/cm2. Laser parameters are shown in Table 1. For pain relief, application of a topical anesthetic cream (L.M.X.4®, Ferndale Laboratories, Inc., Ferndale, MI, USA) to the lesion at 1 mm thickness was done. And it was covered with an occlusive dressing before the laser treatment. After thirty minutes, the anesthetic was removed and cooling gel was applied to the lesion.
Multiple non-overlapping treatments were delivered to blebbed PWS and the clinical endpoint was constriction, darkening, or lightening of the vessels. All patients were advised that the treated area might have a bruised appearance for up to 2 weeks after the treatment, and that sun exposure should be avoided. No other wound care was recommended, except for the application of antibiotic ointment if blistering occurred.
At each clinical session, patients were routinely asked concerning the treatment response and adverse effects, and clinical improvement were determined by a clinical team, using a standard quartile grading scales (1~25%, 26~50%, 51~75%, >75% improvement), according to the comparison of the photographs at the baseline and at 8 weeks after the end of the treatment.
In general, all patients tolerated the treatment well, and clinical improvement of blebbed PWS was observed after use of a 1,064 nm long pulsed Nd:YAG laser with contact cooling device treatment. Excellent clinical improvement (>75%) was observed in 11 subjects, moderate improvement (51~75%) was observed in 7 subjects, and mild improvement (26~50%) was observed in 3 subjects (Fig. 1 and 2, Table 1); 85.7% of the patients experienced either a moderate or excellent response, with greater than 50% clearance. According to their size, most blebbed lesions required three or fewer treatment sessions at 8-week intervals. The total number of PDL treatments applied to the surrounding flat lesions were varied (range 1~12; mean 5.44). Selective epidermal cooling permits the use of higher dosages of light. Neither the total size of PWS nor the skin type was associated with the outcome of treatment.
Except for trivial textural change, no complications were observed. Purpura was the most common immediate adverse reaction, but was mild and transient. Other acute reactions, including erythema, edema, and blanching, were observed, but were also transient. Blistering was not observed and discoloration of any type was gone within approximately 4 weeks. No pigmentary changes or scarring were observed in any of the subjects throughout the treatment and follow-up periods.
Improvements in laser technology over the past decades have allowed for expedited lesion clearing, even for adult patients with PWS. Despite decades of improvement, laser therapy for the treatment of PWS remains a major challenge. For many clinicians, the pulsed dye laser (PDL) is considered as the treatment of choice for PWSs. Almost all PWSs lighten after a series of PDL exploiting wavelengths, ranging from 585 to 600 nm; however, blebbed PWS cannot be completely removed due to limited penetration depth. Different strategies, including excision, electrocautery, repetitive PDL treatments, pulse stacking with PDL, intense pulsed light platforms, and Nd:YAG 1,064 nm have been used for the treatment of resistant PWS4,5. A long-pulsed Nd:YAG laser penetrates deeply into the skin, and it can be effective in the treatment of vascular targets, such as nodular lesions in PWS and reticular leg veins, and provides cosmetically acceptable results6,7.
Selective epidermal cooling, which was studied by Gilchrest et al.8, was introduced in an effort to preserve the epidermis during the laser treatment of a dermal targets. Dynamic cooling devices, such as cold air (forced air convection), cryogen spray, and contact cooling (sapphire window), have generally allowed for use of higher fluencies in the vascular laser systems. Cooling, as well as a reduction of fluence, prevents adverse effects, such as pigmentary changes and scar formations, and also decreases pain during the treatment, and increases therapeutic outcome.
We have treated most blebs in PWSs using a 1,064 nm long pulsed Nd:YAG laser with contact cooling device. The laser penetrates more deeply into the tissue than visible light, therefore enabling a more deeper heat delivery into these relatively large vascular structures. In addition, it has a contact cooling system that is suitable for epidermal protection, contact compression capacity for control of blood flow to the treated area, and delicate cooling time control on demand. Furthermore, because absorption of melanin, at the 1,064 wavelength is relatively low, it is also suitable for patients with darker skin types, like Asians, whose epidermal melanin, present at higher concentrations, can act as a competing target chromophore for laser light. In this study, a 1,064 nm long pulsed Nd:YAG laser with fluence of 95 J/cm2 to 170 J/cm2, 20 ms to 30 ms pulse duration, 5 mm to 6 mm spot size, and dynamic cooling 30 to 40/20 was used every 8 weeks, illustrating an excellent response with treatment. Compared with the similar cases, which reported in other countries, there's no big difference in the parameter. In foreign countries, however, they mostly conducted a study with the sample of white people; therefore, when we consider that the target of this study are all non-Caucasians, we can see an excellent result, setting up a similar parameter. Also, it's quite remarkable that there are no side effects, such as hyperpigmentation and atrophic scar. Viewed in this light, a 1,064 nm long-pulsed Nd:YAG laser provide a effective treatment for the PWS in most skin types.
PWS typically consists of blood vessels with a diameter between 10 and 50 µm. Very few are >100 µm and most are <20 µm9. Non-responding PWS probably consist of vessels that are too small or too large. Very small vessels might contain too little oxyhemoglobin to permit sufficient absorption and consequent heating of the vessel wall. In very large vessels, there might not be sufficient energy to heat the whole target10. In addition, in the study from Yang et al.11, minimum purpuric dose (MPD) for long pulsed Nd:YAG laser varies widely among different PWS, and MPD values were lower in darker PWS. Based on the facts, laser setting, such as fluence and spot size were carefully determined, according to bulky malformation, the level of maturity, and MPD, and were used with 30 ms pulse duration based on our experience.
Laser therapy of PWS at younger ages is more effective than the treatment in adults, based on the premise that these lesions are relatively immature, and consists of superficial and smaller vessels12. Important morphological factors include depth of vessels, with superficially located vessels confirmed as a favorable factor13. The size and location of PWS are also important prognostic factors. A lesions on the head and neck, showing a better response than those at the other sites, and even among those confined to the face, the peripheral face, in particular, the central forehead, confers a better prognosis than the centrofacial areas (V2 distribution)14. Broader lesions (more than 20 cm2) tend to require additional laser treatments, compared with narrow lesions, with clearing tending to start from the periphery of lesions. These prognostic factors, determining therapeutic response, may allow for better appreciation of the heterogeneity of PWS, and eventually lead to a more targeted treatment.
PWS are commonly found on the face and neck, and, as such, may have serious psychological consequences. PWS also do not involute over time and may become hypertrophied in adulthood, resulting in an increased disfigurement. For these reasons, early intervention is needed. In blebbed PWS that are resistant to other treatment, our protocol - a 1,064 nm long pulsed Nd:YAG laser with contact cooling device on blebs, followed by PDL on the surrounding flat lesions - may be an efficacious alternative modality of choice for the treatment of blebbed PWS.
Figures and Tables
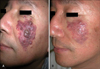 | Fig. 1Patient 7. (A) Several violaceous nodules with surrounding erythematous flat plaques on the left cheek (V2 distribution of a trigeminal location), (B) On blebs, three sessions of treatment with a 1,064 nm long pulsed Nd:YAG laser with contact cooling and six sessions of PDL on surrounding flat lesions. |
 | Fig. 2Patient 11. (A) Asymptomatic multiple purple nodules with surrounding erythematous flat plaques on the right cheek and nose (V2 distribution of a trigeminal location), (B) On blebs, one session of treatment with a 1,064 nm long pulsed Nd:YAG laser with contact cooling and five sessions of pulsed dye laser on surrounding flat lesions. |
References
1. Adamic M, Troilius A, Adatto M, Drosner M, Dahmane R. Vascular lasers and IPLS: guidelines for care from the European Society for Laser Dermatology (ESLD). J Cosmet Laser Ther. 2007. 9:113–124.

2. Lanigan SW, Taibjee SM. Recent advances in laser treatment of port-wine stains. Br J Dermatol. 2004. 151:527–533.

3. Chapas AM, Geronemus RG. Physiologic changes in vascular birthmarks during early infancy: mechanisms and clinical implications. J Am Acad Dermatol. 2009. 61:1081–1082.

4. Ahcan U, Zorman P, Recek D, Ralca S, Majaron B. Port wine stain treatment with a dual-wavelength Nd:Yag laser and cryogen spray cooling: a pilot study. Lasers Surg Med. 2004. 34:164–167.

5. Stier MF, Glick SA, Hirsch RJ. Laser treatment of pediatric vascular lesions: Port wine stains and hemangiomas. J Am Acad Dermatol. 2008. 58:261–285.

6. Groot D, Rao J, Johnston P, Nakatsui T. Algorithm for using a long-pulsed Nd:YAG laser in the treatment of deep cutaneous vascular lesions. Dermatol Surg. 2003. 29:35–42.

7. Dover JS, Sadick NS, Goldman MP. The role of lasers and light sources in the treatment of leg veins. Dermatol Surg. 1999. 25:328–335.

8. Gilchrest BA, Rosen S, Noe JM. Chilling port wine stains improves the response to argon laser therapy. Plast Reconstr Surg. 1982. 69:278–283.

9. Edström DW, Hedblad MA, Ros AM. Flashlamp pulsed dye laser and argon-pumped dye laser in the treatment of port-wine stains: a clinical and histological comparison. Br J Dermatol. 2002. 146:285–289.

10. Frohm Nilsson M, Passian S, Wiegleb Edstrom D. Comparison of two dye lasers in the treatment of port-wine stains. Clin Exp Dermatol. 2010. 35:126–130.

11. Yang MU, Yaroslavsky AN, Farinelli WA, Flotte TJ, Rius-Diaz F, Tsao SS, et al. Long-pulsed neodymium:yttrium-aluminum-garnet laser treatment for port-wine stains. J Am Acad Dermatol. 2005. 52(3 Pt 1):480–490.

12. Haedersdal M, Efsen J, Gniadecka M, Fogh H, Keiding J, Wulf HC. Changes in skin redness, pigmentation, echostructure, thickness, and surface contour after 1 pulsed dye laser treatment of port-wine stains in children. Arch Dermatol. 1998. 134:175–181.

13. Nguyen CM, Yohn JJ, Huff C, Weston WL, Morelli JG. Facial port wine stains in childhood: prediction of the rate of improvement as a function of the age of the patient, size and location of the port wine stain and the number of treatments with the pulsed dye (585 nm) laser. Br J Dermatol. 1998. 138:821–825.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download