Dear Editor:
Behçet's disease (BD) is a systemic inflammatory disorder characterized by recurrent oral ulcers, genital ulcers, uveitis, and skin lesions1. Involvement of other organs such as gastrointestinal (GI) tract, central nervous system (CNS) or large vessels is less frequent. Among these systemic involvements of BD, GI involvement is relatively common; it occurs in approximately 10~30% of East-Asian BD patients2-4. Neuro-Behçet's disease (NBD) is relatively rare; the prevalence was about 5% in a large Korean epidemiologic study5,6. Due to the low prevalence and lack of large controlled studies, the clinical course and the presence of other organ involvement in patients with NBD is yet to be confirmed. Herein we report a rare case of simultaneous involvement of nervous and GI systems in a young female patient with BD. A 34-year-old woman with recurrent orogenital ulcers had been visiting outpatient clinics regularly since March 2007. Three months later, she complained of severe lower abdominal pain. Colonoscopic examination revealed a deep ulcer on the ileocecal valve, and administration of oral corticosteroids and sulfasalzaine was started on the suspicion of Behçet's colitis. Within one month of the medication, she additionally complained of left hemiparesis and facial palsy, dysarthria, and diplopia in spite of steroid treatment, and she was referred to our clinic. Brain magnetic resonance imaging showed a small acute infarction at the right central area of the midbrain and upper pons (Fig. 1). The characteristic location of the infarction without evidence of other demyelinating diseases and the typical clinical manifestations lead to the diagnosis of NBD, with the coexistence of Behçet's colitis. Since then, regular medication (prednisolone 10 mg/day) was taken over a 3-year follow up and then withdrawn. During the follow-up period, there was no evidence of disease progression though sequelae of NBD were observed. However, in October 2010, she presented with a 1-day history of lower abdominal pain and fever. Abdominal computed tomography studies revealed an ulcerative lesion in the terminal ileum (Fig. 2A). On emergency bowel resection, a 1 cm-sized ulceration was found around the ileocecal valve. Microscopically, the specimen showed chronic perforating enterocolitis with multiple ulcerations, consistent with recurrent Behçet's colitis (Fig. 2B). Oral corticosteroid (prednisolone 30 mg/day) was administrated for 10 days and tapered to 10 mg/day as maintenance therapy for 3 months. After a 5-month follow-up period, she remains stable with steroid-free therapy at present.
There are addressable issues in our case. First, the patient with BD had simultaneous onset of active ileal ulceration and acute neurologic deficits, which is known to be very rare7,8. However, she had suffered from Behçet's colitis since 1999 and the neurologic events followed 5 years later. Second, both systemic involvements of BD developed almost immediately following the initial diagnosis in this case. It was previously reported that both CNS and GI involvement in BD usually develops later in most cases - on average 4 years and 2 years after diagnosis, respectively9,10. In accordance with that report, there has been only one additional case, a 60-year-old woman, in our clinic who have had both CNS and GI involvement (data not shown). Third, NBD is known to be more frequent in males; however, both this case and the additional case of the 60-year-old woman were female. Generally, eye and CNS involvement are more frequent in males, while genital ulcers and arthritis are more frequent in females9. Finally, despite proper steroid treatment for Behçet's colitis, a new onset of CNS involvement and recurrence of ileocecal ulcer developed in our case.
Recently it was reported that a large deep ulcer may contribute to a refractory clinical course and a poor prognosis for patients with Behçet's colitis11. Our patient had about a 1 cm-sized deep ulcer, which could have contributed to the aggressive nature of the disease. In addition, there have been two case reports of acute neurologic deficits in BD patients who had a consequent active ileocecal ulcer in spite of steroid pulse therapy7,12. It seems that systemic steroid treatment may not be enough to control acute and severe systemic involvement in BD. Although the causes of the aggressive and refractory course of disease were not clearly demonstrated, genetic polymorphisms such as in the matrix metalloproteinases (MMPs) gene might affect clinical and therapeutic outcomes in BD13. Homozygotes of MMP-9 (MMP9-1562*C/*C), a novel susceptibility gene, and which might affect the natural course of BD, was also found in our case (data not shown). In conclusion, we experienced a rare case of simultaneous involvement of nervous and GI systems in refractory BD. Further studies of genetic polymorphisms of other candidate genes may clarify the individual differences in therapeutic outcomes and disease courses of BD.
Figures and Tables
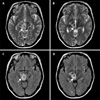 | Fig. 1Axial brain magnetic resonance imaging revealed a hyperintense lesion in the right central area of the mesodiencephalic junction on a T2-weighted image (A: midbrain, B: upper pons) and a fluid-attenuated inversion-recovery sequence (C: midbrain, D: upper pons). These findings suggested that a small infarction had occurred (arrows). |
 | Fig. 2(A) Abdominal computed tomography study revealed an ulcerative lesion in the terminal ileum (arrows). (B) The specimen from ileocecal resection revealed perforating enterocolitis with multiple ulceration, lymphoid aggregates, and fibrosis, consistent with Behçet's colitis (original magnification, H&E, ×10). |
References
1. Sakane T, Takeno M, Suzuki N, Inaba G. Behçet's disease. N Engl J Med. 1999. 341:1284–1291.
2. Bayraktar Y, Ozaslan E, Van Thiel DH. Gastrointestinal manifestations of Behcet's disease. J Clin Gastroenterol. 2000. 30:144–154.

3. Lakhanpal S, Tani K, Lie JT, Katoh K, Ishigatsubo Y, Ohokubo T. Pathologic features of Behçet's syndrome: a review of Japanese autopsy registry data. Hum Pathol. 1985. 16:790–795.

4. Kim HJ, Bang D, Lee SH, Yang DS, Kim DH, Lee KH, et al. Behçet's syndrome in Korea: a look at the clinical picture. Yonsei Med J. 1988. 29:72–78.
5. Bang D, Lee JH, Lee ES, Lee S, Choi JS, Kim YK, et al. Epidemiologic and clinical survey of Behcet's disease in Korea: the first multicenter study. J Korean Med Sci. 2001. 16:615–618.
6. Al-Araji A, Kidd DP. Neuro-Behçet's disease: epidemiology, clinical characteristics, and management. Lancet Neurol. 2009. 8:192–204.

7. Ohira H, Tsutsumi A, Yasuda S, Horita T, Takeuchi R, Kasahara H, et al. Severe neuro-Behçet with perforation of the intestine. Nihon Naika Gakkai Zasshi. 2000. 89:1435–1437.

8. Ideguchi H, Suda A, Takeno M, Kirino Y, Ihata A, Ueda A, et al. Neurological manifestations of Behçet's disease in Japan: a study of 54 patients. J Neurol. 2010. 257:1012–1020.

9. Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y. Behçet disease: evolution of clinical manifestations. Medicine (Baltimore). 2011. 90:125–132.

10. Alpsoy E, Donmez L, Onder M, Gunasti S, Usta A, Karincaoglu Y, et al. Clinical features and natural course of Behçet's disease in 661 cases: a multicentre study. Br J Dermatol. 2007. 157:901–906.
11. Kim MC, Shin SJ, Lim SG, Lee KR, Woo H, Choi SJ, et al. Clinical course of intestinal Behcet's disease according to the characteristics of ulcer in colonoscopy. Intest Res. 2010. 8:40–47.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download