Abstract
Granular parakeratosis is a recently recognized disorder of keratinization that is usually confined to intertriginous areas. The histopathologic features are distinctive and diagnostic. Rarely, histopathologic variants such as follicular granular parakeratosis and granular parakeratosis of eccrine ostia have been described. In this report, we describe a rare case of granular parakeratosis mostly confined to eccrine ostia.
Granular parakeratosis is an uncommon acquired disorder of keratinization. It is characterized by keratotic papules or plaques that are located in the intertriginous areas. Histopathologic features consist of hyperkeratosis, parakeratosis, and retention of keratohyaline granules in the stratum corneum. Until now, only one case of granular parakeratosis confined to the eccrine ostia has been reported1. We describe a rare case of granular parakeratosis that mostly affected the eccrine ostia.
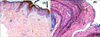
A 60-year-old female patient visited our clinic in August with a 15-year history of multiple brownish verrucous papules on her neck (Fig. 1A). She reported that each year these lesions appear in the spring, became more aggravated in the summer and resolved spontaneously in the fall or winter. Moreover, these lesions worsened when the patient was exposed to a hot environment, such as a sauna. Because the patient became hot easily and sweated profusely, especially on the neck, she regarded the lesions as a heat rash. Applications of topical steroids and antiperspirants, however, were ineffective. While sweating, the patient felt a burning sensation in the area around the lesions. A biopsy specimen of the papules revealed hyperkeratosis and prominent parakeratosis of the stratum corneum (Fig. 2A). High power resolution showed that the parakeratotic corneocytes contained basophilic granules similar to keratohyaline granules of the stratum granulosum (Fig. 2B). These changes were especially prominent around the eccrine ostia. The cutaneous lesions of our patient resolved spontaneously as the climate became cooler, and cleared completely when the patient revisited our clinic in October (Fig. 1B).
Granular parakeratosis is a rare benign disorder initially described by Northcutt et al.2 in 1991, who used the term "axillary granular parakeratosis". Women are affected more commonly than men3. It usually occurs during middle-age, but may also be observed in children4. Granular parakeratosis usually presents as hyperkeratotic papules or plaques on skin folds, including the axilla, groin, and mammary crease. It sometimes occurs on the abdomen or lumbosacral area.
Although the etiology of granular parakeratosis is unknown, it may be associated with contact reactions to antiperspirants, occlusion, excessive use of creams, and obesity. On the molecular level, granular parakeratosis has been associated with abnormalities in profilaggrin processing5, suggesting that the various aforementioned triggering factors may interfere with profilaggrin processing, resulting in granular parakeratosis. Granular parakeratosis may also be an epiphenomenon of molluscum contagiosum6, dermatomyositis7, fungal infection8, or carcinoma9. In our patient, granular parakeratosis was not an incidental finding because several lesions showed the same clinical findings of verrucous papules.
Histopathologically, granular parakeratosis is characterized by hyperkeratosis and prominent parakeratosis of the stratum corneum. Under high resolution, parakeratotic corneocytes have been found to contain keratohyaline granules, which are regarded as diagnostic. Although most patients with this condition have diffuse granular parakeratosis, some have variants such as follicular granular parakeratosis10 and granular parakeratosis of the eccrine ostia1.
Patients with the latter showed similar clinical presentation to our case; black and brownish spiny papules on the neck, which appeared in August, as well as experiencing a tingling sensation upon sweating1. The similar clinical manifestations and histopathologic findings of both conditions suggest that the pathomechanism of granular parakeratosis related with eccrine structures may be associated with sweating or high temperature. Another interesting feature is that both cases had these skin lesions on the neck, which is an unusual site for granular parakeratosis. This finding may be because the neck is an area susceptible to profuse sweating during hot season.
Many treatments have been attempted, but there is no optimal therapy for granular parakeratosis. Some cases have resolved spontaneously, while others resolved by stopping deodorant use. Various responses have been observed after treatment with oral and topical corticosteroid, oral and topical retinoid, oral and topical antifungal agents, oral antibiotics, topical vitamin D analogues, topical ammonium lactate, cryotherapy and botulinum toxin injection. In our case, the skin lesions disappeared as the temperature dropped. This phenomenon supports the aforementioned hypothesis that granular parakeratosis confined to eccrine ostia may be associated high temperature.
In conclusion, we report a unique histopathologic variant of granular parakeratosis that mainly affected the eccrine ostia.
Figures and Tables
Fig. 1
(A) Photograph of the patient at the first visit to our clinic in August, showing multiple tiny blackish verrucous papules on the neck. (B) Photograph at the follow-up visit in October, showing disappearance of cutaneous lesions.

Fig. 2
Histopathologic examination of a punch biopsy taken from the patient's neck, showing (A) hyperkeratosis and parakeratosis (arrows) (H&E, ×40). (B) Higher magnification showing parakeratotic corneocytes containing multiple basophilic granules (arrows), similar to keratohyaline granules (H&E, ×400). These changes were especially prominent in the stratum corneum of eccrine ostia.
References
1. Wang L, Yang L, Wang G, Gao T. Granular parakeratosis of eccrine ostia. Am J Dermatopathol. 2008. 30:65–66.

2. Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol. 1991. 24:541–544.

3. Scheinfeld NS, Mones J. Granular parakeratosis: pathologic and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol. 2005. 52:863–867.

4. Neri I, Patrizi A, Guerrini V, Fanti PA. Granular parakeratosis in a child. Dermatology. 2003. 206:177–178.

5. Metze D, Rütten A. Granular parakeratosis - a unique acquired disorder of keratinization. J Cutan Pathol. 1999. 26:339–352.

6. Pock L, Cermáková A, Zipfelová J, Hercogová J. Incidental granular parakeratosis associated with molluscum contagiosum. Am J Dermatopathol. 2006. 28:45–47.

7. Pock L, Hercogová J. Incidental granular parakeratosis associated with dermatomyositis. Am J Dermatopathol. 2006. 28:147–149.

8. Resnik KS, Kantor GR, DiLeonardo M. Dermatophyte-related granular parakeratosis. Am J Dermatopathol. 2004. 26:70–71.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download