Abstract
Eccrine angiomatous hamartoma (EAH) is a rare benign disease that is characterized by an abnormal proliferation of eccrine glands and vascular elements. It is generally congenital, but it can appear before puberty. It usually presents as a single plaque or nodule, but multiple patch-like lesions are also possible. EAH is mostly asymptomatic, but it is sometimes associated with pain or hyperhidrosis. It generally does not require aggressive treatment, but the lesion can be excised due to pain, enlargement and cosmetic reasons. A 3-week-old Korean female presented with a hemorrhagic skin lesion on the right foot since birth. There was no specific birth history. The lesion first appeared on the third toe of the right foot and quickly spread to almost half of the right foot. Histopathology examination revealed acanthosis in the epidermis and a proliferation of eccrine ducts, glands and capillaries. The eccrine glands were immunohistochemically-positive for carcinoembryonic antigen.
Eccrine angiomatous hamartoma (EAH) is a rare disease that is histologically characterized by increased numbers of eccrine structures and numerous capillary channels1. It commonly appears as a flesh-colored, red, violaceous, blue, or yellow-colored solitary nodule or plaque on the distal extremities, sometimes presents as multiple papules, and rarely presents as maculopatches on the trunk, buttocks, and neck. It may be congenital or it can arise before puberty, but the lesion rarely presents in adulthood. EAH is mostly asymptomatic, but pain, hypertrichosis, and local hyperhidrosis are commonly reported features. Enlargement typically occurs and this is associated with growth of the patient. Although it is a benign hamartoma, it is often excised because of pain or enlargement and for cosmetic reasons2.
We report here on a case of a congenital EAH that appeared as fast-growing hemorrhage-like maculopatches.
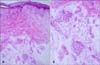
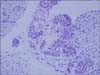
A 3-week-old Korean girl presented with well-demarcated hemorrhage-like maculopatches on the right foot since birth, and this lesion had appeared as a small hemorrhagic macule on the third toe of the right foot and then quickly spread over the ensuing 1 week. There was no specific birth history or trauma history. On examination, the lesions were revealed to be erythematous petechiae-like maculopatches that covered almost half of the right sole dorsum and toes. The condition was seemingly painless with palpation and it did not appear to be hypertrichotic (Fig. 1). The mother of the patient reported that there was no hyperhidrosis. A 4-mm punch biopsy was done. In the subsequent histopathology, slight acanthosis was found in the epidermis. In the dermis, there were numerous hyperplastic eccrine glands and capillaries nearby, but no pilar, lipomatous, mucinous, or lymphatic structural hyperplasia (Fig. 2). The eccrine glands were positive for carcinoembryonic antigen (CEA) on immunohistochemistry examination (Fig. 3). Based on the histopathological features, the lesion was diagnosed as EAH. The treatment options presented to the parents included observation or surgical excision. The decision was for observation.
EAH is a rare benign tumor of the skin, and it is defined histopathologically as eccrine hyperplasia with a proliferation of vascular elements and, in some cases, the presence of other dermal elements such as mucin or lipid. The first of these lesions was documented in 1859 in the description of an angiomatous tumor located on the cheek of a child2. The term EAH was coined in 19683. Other terms such as sudoriparous angioma were used in prior reports3. A pathophysiologic theory to explain EAH involves a biochemical fault in the interactions between the differentiating epithelium and subjacent mesenchyme that gives rise to an abnormal proliferation of adnexal and vascular structures4.
A study that reviewed 37 EAH cases revealed the generally congenital nature of EAH (16 of 35 cases, 45.7%; two cases were not mentioned) and its prevalent appearance at a prepuburtal age (21 of 36 cases, 58%; one case was not mentioned)2. Although it rarely occurs in adulthood, there have been some reported cases of late-onset EAH5. Results from the same study indicate that a single nodule (32/37, 86.5%) or plaque (28/37, 75.6%) is the dominant lesion, but multiple nodules (5/37, 13.5%) or papulopatches (12/37, 32.4%) are also possible, and that EAH is mostly located in the extremities (30/37,81.1%). Considering the reported clinical symptoms, EAH has various features. Results from the aforementioned study indicated an asymptomatic nature (12/33, 36.3%), but it can also present with pain (14/33, 42.4%), hyperhidrosis (12/35, 34.3%) or hypertrichosis (10/37, 27.0%). There is no gender preference. The same clinical features were evident in five congenital cases2,4. The clinical differential diagnoses of EAH include vascular malformations, tufted angioma, smooth muscle hamartoma, glomus tumor, blue rubber bleb nevus, and macular telangiectatic mastocytosis2.
In addition to the present data, we also reviewed the results from 14 Korean cases6-16. A summary of the results is presented in Table 1; the clinical features were almost the same clinical features as those described in an English review article2. The present and previous Korean patient data were obtained from slightly more females (n=9) than males (n=6). The lesions were mostly congenital (9/14, 64.2%), and lesions could be be asymptomatic (5/15, 33.3%) or painful (6/15, 40.0%), and excessive sweating was evident (10/15, 66.7%). A single lesion was typically present (12/15, 80.0%) and almost always as a nodule (11/15, 73.3%). But, three cases that presented as a patch, including our case. Lesions appeared on the extremities in most cases (12/15, 80.0%). Clinically, our case was quite consistent with most of the reported cases, except for the appearance as a skin patch instead of as nodules or plaques. Although two previous cases displayed a lesion patch, similar to the present case, they did not show traumatic hemorrhage-like maculopatches as in our case. Rather, the lesions of the two previous cases appeared like a nevus flammeus eruption8,16. The present case could represent a truly new type of EAH lesion. Alternatively, it may have not fully developed to become a nodule or plaque because the patient was too young. The differential diagnoses of hemorrhage-like maculopatches in infants include hematologic disorder, such as leukemia and Langerhans cell histiocytosis, hemangioma, and true traumatic hemorrhage.
Histologically, EAH displays variable epidermal findings such as normal or irregular acanthosis, papillomatosis and/or hyperkeratosis, hyperplasia of normal or dilated eccrine glands in close association with capillary angiomatous foci, and the variable presence of pilar, lipomatous, mucinous, and lymphatic structures2,4. There was mild acanthosis in the epidermis and hyperplasia of the nearby normal eccrine glands and capillaries in our case. These findings match with those of most of the previous cases.
Immunohistochemical analyses of EAH has demonstrated that the secretory portions of the eccrine glands are positive for S100, CEA, epithelial membrane antigen, and Cam5.2, and that the ductal components stain positively for CEA and cytokeratin 1, and are weakly positive for epithelial membrane antigen2. CEA staining done presently was also positive on the ductal and secretory portions of the eccrine glands.
In summary, we report here on a case of congenital EAH that had the appearance of a hemorrhagic lesion. To the best of our knowledge, this is the first case of EAH showing such unique clinical features.
Figures and Tables
References
1. Ahmed TSS, Del Priore J, Seykora JT. Elder DE, Elenitsas R, Johnson B, Loffreda M, Miller J, Miller OF, editors. Tumors of the epidermal appendages. Lever's histopathology of the skin. 2009. Philadelphia: Lippincott-Williams and Wilkins;883.
2. Pelle MT, Pride HB, Tyler WB. Eccrine angiomatous hamartoma. J Am Acad Dermatol. 2002. 47:429–435.

3. Foshee JB, Grau RH, Adelson DM, Crowson N. Eccrine angiomatous harmartoma in an infant. Pediatr Dermatol. 2006. 23:365–368.

4. Larralde M, Bazzolo E, Boggio P, Abad ME, Santos Muñoz A. Eccrine angiomatous hamartoma: report of five congenital cases. Pediatr Dermatol. 2009. 26:316–319.

5. Jeong E, Park HJ, Oh ST, Lee JY, Cho BK. Late-onset eccrine angiomatous hamartoma on the forehead. Int J Dermatol. 2006. 45:598–599.

6. Ahn KJ, Kim KJ, Lee YS. Eccrine angiomatous hamartomam: report of case. Korean J Dermatol. 1981. 19:527–531.
7. Kim ST, Kim DH, Joung SW, Jun JB. A case of eccrine angiomatous hamartoma. Korean J Dermatol. 1982. 20:623–627.
8. Kim HY, Hwang SW, Kim YP. Sudoriparous angioma: report of two cases. Korean J Dermatol. 1982. 20:885–889.
9. Choi GJ, Cho KH, Houh D, Kim HO, Kim CW. Two case of sudoriparous angioma. Korean J Dermatol. 1982. 20:957–964.
10. Lee JC, Park JJ, Jung EC, Park SR. A case of eccrine angiomatous hamartoma. Korean J Dermatol. 1988. 26:255–258.
11. Ryu HJ, Oh CH, Kim IH. Two cases of eccrine angiomatous hamartoma. Korean J Dermatol. 2002. 40:1393–1396.
12. Choi J, Chung EC. A case of eccrine angiomatous hamartoma. Korean J Dermatol. 2003. 41:951–953.
13. Yoon SY, Choi MJ, Kang H. A case of eccrine angiomatous hamartoma in neurofibromatosis type-1 patient. Korean J Dermatol. 2006. 44:1339–1341.
14. Kwon YS, Lee KY, Kim DY, Park YK, Lee JH. A case of eccrine angiomatous hamartoma with unusual lipomatous involvement. Korean J Dermatol. 2008. 46:295–297.
15. Kim KH, Park HJ, Lee YS. A case of eccrine-pilar angiomatous hamartoma showing an unusual clinical manifestation. Korean J Dermatol. 1984. 22:549–552.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download