Abstract
Generalized granuloma annulare (GGA) is a rare benign granulomatous dermatosis characterized by disseminated necrobiotic dermal papules. Histologically, it presents as a lymphohistiocytic granuloma associated with varying degrees of connective tissue degeneration. It usually occurs in adults and rarely affects infants. Herein, we report an interesting case of GGA which occurred in a 3 month-old girl in association with Bacillus Calmette-Guerin vaccination.
Granuloma annulare (GA) is a benign granulomatous dermatosis, classified into localized, generalized, subcutaneous, and perforating types, depending on clinical manifestations. It has been known that generalized granuloma annulare (GGA) occurs in about 8-15% of all types of GA, mostly in adults aged 50 years or over and children aged about 10 years1,2. It has been suggested that some GGAs are associated with diabetes, thyroid diseases, and infectious diseases, such as chronic hepatitis C and acquired immune deficiency syndrome. It has presented as a paraneoplastic syndrome accompanied by malignant tumor, and has been reported to occur after Bacillus Calmette-Guerin (BCG), hepatitis B, or diphtheria/tetanus vaccinations3-9. Herein, we report a rare case of GGA related to BCG vaccination in a 3-month-old female. Only one case has been reported in the Korean literature3 but none in the English literature.
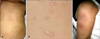
A 3-month-old girl presented with a month history of generalized asymptomatic papules. She had received a BCG vaccination on the left upper arm 1 month prior. At that time, there was an inflammatory reaction at the BCG injection site, which spontaneously disappeared after several days. One month later, skin lesions developed on the left upper arm at the BCG injected site and disseminated all over the body. The personal and family histories were not remarkable. Dermatological examination revealed well-demarcated, slightly erythematous firm papules on the trunk and extremities (Fig. 1). A skin biopsy specimen, taken from a papule on the trunk, revealed mild parakeratosis, acanthosis, focal spongiosis, and pale eosinophilic granular areas of degenerated collagen bundles surrounded by dense infiltration of lymphohistiocytes and multinucleated giant cells in the dermis (Fig. 2). Although Alcian blue staining of the section was negative, elastic staining showed a decrease of elastic fibers in the dermis, especially at the area of degenerated collagen. AFB staining, PAS staining, and Tb-PCR showed all negative results. After the treatment with topical steroid (Desonide 0.05% lotion) for a month, the lesions were resolved, and no relapse has occurred for 6 months.
GGA is a rare variant of GA, which affects the trunk and extremities. It is characterized by a later age of onset, a wide distribution of lesions, a chronic course with only rare spontaneous resolution, and a poor response to therapy compared with the localized type2,10. Although the pathogenensis of GGA has not been fully elucidated, the presence of activated T-cells in GA suggests that cell-mediated immunity plays a role. Additionally, it has been reported that GA occurred in association with trauma, insect bite, sun exposure, virus infection, and BCG vaccination2-5.
Four cases of infantile GGA have been reported in Korea1,3,11. Of these, 1 case was related to BCG vaccination (Table 1)3. In our case, the patient's parents mentioned that erythema and edema with heating sensation were present in the vaccinated area after a month of BCG vaccination and that they spontaneously resolved without treatment. Therefore, it was diagnosed as BCGitis. The skin lesions started from the BCGitis area and disseminated to the whole body, suggesting that BCG vaccination was a precipitating factor of GGA in our case. BCG vaccine contains a live, attenuated strain of Mycobacterium bovis, which is used worldwide for the prevention of tuberculosis. It is known that BCG is relatively safe; however, it has been reported that it may cause cutaneous complications--specific reactions (lymphadenitis, scrofuloderma, lupus vulgaris, lichen nitidus, or tuberculid) and nonspecific reactions (urticaria, purpura, granuloma annulare, erythema nodosum, or erythema multiforme)3. In particular, GA as a complication of BCG vaccination was reported in 2 cases in the English literature and 1 case in the Korean literature 3-5. It suggested that GA might occur in relation to the physical trauma of vaccination or a cell-mediated delayed hypersensitivity reaction against a certain antigen of the vaccine.
It is necessary to distinguish GGA from interstitial granulomatous dermatitis, papular xanthoma, or other infectious diseases such as cutaneous tuberculosis that show granulomatous lesions on histology. Interstitial granulomatous dermatitis is characterized by symmetric distribution of asymptomatic erythematous plaques or papules on the trunk and extremities, and shows palisading granulomas surrounding degenerated collagen on histology. However, it is differentiated by the findings that the infiltrating cells usually are neutrophils and eosinophils, and that dense lymphohistiocytic infiltration over the reticular dermis is present. In case of papular xanthoma, the asymptomatic yellow papules are mostly distributed on the head, trunk and upper extremities, and interstitial granulomas and histiocytes are observed on histology, but mainly foam cells and Touton giant cells are observed. In addition, we performed AFB staining, PAS staining, and a Tb-PCR test to distinguish GGA from infectious diseases, and those results were all negative, thereby excluding infectious diseases.
It has been reported that GGA shows more resistance to therapy than the localized type. Various treatments, such as systemic/topical steroids, cyclosporine, PUVA (psoralen+ UVA therapy), retinoid, antimalarial agents, Dapsone, and so on have been tried; however, those were not apparently effective2,10. Though the prognosis of our case and previously reported cases in infants were relatively good, they regressed 1 to 3 months after administration of oral or topical steroids and GGA did not recur, presenting different clinical courses from GGA in adults.
Herein, we report an interesting case of GGA which occurred in a 3 month-old girl in association with BCG vaccination, and it was rapidly improved by only applying topical steroids for a month, a treatment course different from that provided to adults afflicted with the condition.
Figures and Tables
Fig. 1
(A) Well-demarcated, slightly erythematous firm papules are present on the trunk. (B) Close-up view. (C) The Bacillus Calmette-Guerin injected site (left upper arm) shows post-inflammatory hyperpigmentation; the papules originated at this site.
References
1. Kim YJ, Kim YC, Lee ES, Kang HY. A case of generalized granuloma annulare in infant. Korean J Dermatol. 2006. 44:645–647.
2. Yun JH, Lee JY, Kim MK, Seo YJ, Kim MH, Cho KH, et al. Clinical and pathological features of generalized granuloma annulare with their correlation: a retrospective multicenter study in Korea. Ann Dermatol. 2009. 21:113–119.

3. Yun JH, Kim KR, Lee JY, Yoon TY. A case of generalized granuloma annulare following BCG vaccination. Korean J Dermatol. 2008. 46:656–659.
4. Houcke-Bruge C, Delaporte E, Catteau B, Martin De Lassalle E, Piette F. Granuloma annulare following BCG vaccination. Ann Dermatol Venereol. 2001. 128:541–544.
5. Kakurai M, Kiyosawa T, Ohtsuki M, Nakagawa H. Multiple lesions of granuloma annulare following BCG vaccination: case report and review of the literature. Int J Dermatol. 2001. 40:579–581.

6. Wolf F, Grezard P, Berard F, Clavel G, Perrot H. Generalized granuloma annulare and hepatitis B vaccination. Eur J Dermatol. 1998. 8:435–436.
7. Criado PR, de Oliveira Ramos R, Vasconcellos C, Jardim Criado RF, Valente NY. Two case reports of cutaneous adverse reactions following hepatitis B vaccine: lichen planus and granuloma annulare. J Eur Acad Dermatol Venereol. 2004. 18:603–606.

8. Baskan EB, Tunali S, Kacar SD, Adim SB, Saricaoglu H. A case of granuloma annulare in a child following tetanus and diphtheria toxoid vaccination. J Eur Acad Dermatol Venereol. 2005. 19:639–640.

9. Baykal C, Ozkaya-Bayazit E, Kaymaz R. Granuloma annulare possibly triggered by antitetanus vaccination. J Eur Acad Dermatol Venereol. 2002. 16:516–518.





 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download