Abstract
Psoriasis is a multi-factorial disease with various clinical manifestations. We present a case of unilateral psoriasis associated with ipsilateral lymphedema that developed after mastectomy for breast cancer. A 42-year-old Korean woman was referred to our clinic with a 1-month history of multiple erythematous scaly patches on the right arm, back, and breast and was diagnosed with psoriasis by a skin biopsy. Three years previously, she had been diagnosed with breast cancer (T1N2), underwent a right quadrantectomy and axillary lymph node dissection, and completed adjuvant chemotherapy followed by high-dose adjuvant radiotherapy. She had started rehabilitation therapy on the right arm for secondary lymphedema 30 months previously. Because of the long interval between radiation and psoriasis, we speculated that changes in the local milieu caused by the lymphedema might be a causative factor. We hereby report a rare case of unilateral psoriasis following post-mastectomy lymphedema.
Psoriasis is an inflammatory disease with various clinical manifestations but it usually shows a symmetric distribution. Several cases with unilateral distribution have been reported under various conditions such as the postoperative state of neurosurgery1, a Koebner reaction after radiotherapy2, and in association with inflammatory linear verrucous epidermal nevus3, and so on. We report the case of a 42-year-old woman, who presented with unilateral psoriasis that developed after an ipsilateral mastectomy for breast cancer.
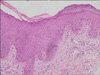
A 42-year-old woman with a known history of breast cancer was referred to our clinic with a 1-month history of multiple erythematous scaly patches on the right side of the arm, breast, and back (Fig. 1A). The lesions on the right arm appeared first and spread serially to the right breast and back during the next month. Three years previously she had been diagnosed with infiltrating ductal carcinoma of the right breast and underwent a right breast-conserving mastectomy and axillary lymph node dissection. Tumor stage was determined pathologically to be T1N2(4/10)M0. Three weeks later, she started adjuvant chemotherapy with four cycles of doxorubicin and cyclophosphamide, followed by four cycles of docetaxel for 5 months. After 1 month, she underwent radiation therapy to the whole right breast with a dose of 50.4 Gy and a boost to the tumor bed with a dose of 9 Gy in 33 total fractions. After radiation therapy was completed, she started rehabilitation therapy with complete decongestive therapy on the right arm for the secondary lymphedema. About 2 year later, she presented with a skin eruption. A physical examination showed multiple, oval to rounderythematous patches with silvery scale on the right arm, breast, and back. No associated symptoms were observed. She still suffered from the lymphedema and wore an elastic compression garment on the entire length of the right arm. A histological examination of the biopsy specimen from the right breast skin lesion revealed an irregular acanthosis with rete ridge elongation, parakeratotic mounds with focal hypogranulosis, and perivascular lymphocytic infiltration into the upper dermis (Fig. 2). Based on the histological features, the skin lesion was diagnosed as psoriasis. The patient was treated with twice-weekly applications of narrow-band ultraviolet B with a starting dose of 300 mJ/cm2 and a combined ointment containing calcipotriol and betamethasone dipropionate once per day. The lesions were nearly resolved after 1 month but post-inflammatory hyperpigmentation remained (Fig. 1B).
Psoriasis is a multi-factorial disease with various clinical patterns. Linear or unilateral psoriasis is a very rare clinical form of skin presentation. The psoriatic lesion commonly occurs as a linear lesion on the limbs but may also be limited to a dermatome on the trunk4. This particular manifestation usually presents related to several conditions, such as a post-nerve injury state1,5 or as a Koebner2,6 or reverse Koebner reaction7 after radiotherapy, in association with inflammatory skin disease3,8.
In our case, several factors were considered the cause of the psoriasis. First, the Koebner phenomenon after radiation therapy could be an etiological factor. However, because of the long interval between radiation and psoriasis, it was difficult to consider the unilateral distribution as a Koebner phenomenon. The Koebner phenomenon usually occurs 7~14 days after injury, but our patient had a 2-year interval between the skin eruption and radiation therapy. Some chemotherapeutic agents9 could induce a psoriasiform eruption. However, our patient had no history of medication that could exacerbate or trigger psoriasis, and the time interval was long after the previous chemotherapy. Paraneoplastic dermatosis10 was also not considered a cause of the skin eruption, because there was no evidence of breast cancer recurrence. Because the previous factors were unsatisfactory as a cause for the unilateral psoriasis, we speculated that the prolonged lymphedema could have led to the development of the psoriasis. Tissue biology changes occur in a state of chronic lymphatic edema, including increases in cytokines, growth factors, and cutaneous structures11. Hyperkeratosis, spongiosis, and edema in the epidermis and elongation of the dermal papillae are observed. In addition, there is remarkable cell infiltration with fibroblasts, histiocytes, and neutrophils in the dermis. Although no case associated with chronic lymphedema has been described, such changes could cause a change in the local tissue milieu and result in an ipsilateral, unilateral distribution. Alternatively, mild damage to the postsurgical peripheral nervous system1,5 could have resulted in the unilateral distribution of psoriasis.
We hereby report a rare case of unilateral psoriasis associated with ipsilateral, post-mastectomy lymphedema.
Figures and Tables
References
1. Reyter I, Woodley D. Widespread unilateral plaques in a 68-year-old woman after neurosurgery. Arch Dermatol. 2004. 140:1531–1536.
2. Ben-Yosef R, Soyfer V, Vexler A. Radiation therapy in cancer patients with psoriasis. The fractionated daily dose and the Koebner phenomenon. Radiother Oncol. 2005. 74:21–23.

3. Menni S, Restano L, Gianotti R, Boccardi D. Inflammatory linear verrucous epidermal nevus (ILVEN) and psoriasis in a child? Int J Dermatol. 2000. 39:30–32.

4. Gudjonsson JE, Elder JT. Wolff K, Goldsmith LA, Katz SJ, Gilchrest BA, Paller AS, Leffell DJ, editors. Psoriasis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;180–181.
5. Joseph T, Kurian J, Warwick DJ, Friedmann PS. Unilateral remission of psoriasis following traumatic nerve palsy. Br J Dermatol. 2005. 152:185–186.

6. Collin B, Zaki I. Koebnerized psoriasis masquerading as recurrent breast cancer. Clin Oncol (R Coll Radiol). 2003. 15:506.

7. Martín JM, Conde A, Pinazo I, García L, Sánchez AL, Pinazo J, et al. Reverse koebnerization after radiotherapy in a woman with a mastectomy for a breast carcinoma. J Am Acad Dermatol. 2006. 55:5 Suppl. S90–S91.
8. Menni S, Grimalt R, Caputo R. Unilateral eruptive psoriasis and lichen striatus. Pediatr Dermatol. 1991. 8:322–324.

9. Cho SG, Park YM, Moon H, Kim KM, Bae SS, Kim GB, et al. Psoriasiform eruption triggered by recombinant granulocyte-macrophage colony stimulating factor (rGM-CSF) and exacerbated by granulocyte colony stimulating factor (rG-CSF) in a patient with breast cancer. J Korean Med Sci. 1998. 13:685–688.

10. Gregoriou S, Korfitis C, Alestas T, Christofidou E, Koumantaki E. Should novel psoriasiform eruptions be considered a paraneoplastic sign of invasion in patients with breast cancer? J Eur Acad Dermatol Venereol. 2007. 21:285–286.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download