Abstract
Compared to cutaneous benign fibrous histiocytoma (BFH), deep-seated BFH is very rare and poorly recognized. Both cutaneous and deep-seated BFH are usually asymptomatic. We herein report a 25 year-old woman who presented with a painful mass in her foot that was poorly controlled by analgesics and associated with walking difficulty. After preoperative ultrasonographic evaluation, the mass was completely excised and histologic exam showed spindle cells loosely arranged in storiform architecture, with CD34-, desmin-, S-100-, focal CD68+, vimentin+, smooth muscle actin+, and factor XIIIa+. The patient was diagnosed with deep-seated BFH based on the histologic, radiologic and intraoperative findings.
Based on location, benign fibrous histiocytomas (BFH) are classified into cutaneous and deep tissue subtypes. Cutaneous BFH are common, while deep-seated BFH are rare and painful, deep-seated dermatofibroma is even more rarely reported.
When BFH is deep-seated and associated with pain, the diagnosis may be very difficult because of its clinical features1. As such, it is frequently confirmed histopathologically following local excision. We herein report a rare case of deep, penetrating, BFH associated with throbbing pain, discuss its histologic, radiologic and intraoperative findings, and perform a literature review.
A 25 year-old woman presented with a two-month history of a slow-growing, painful mass in her foot. She complained of difficulty in walking due to pain. On physical examination, a painful, erythematous nodule was observed on the right foot (Fig. 1A). It was initially considered an abscess for which antibiotics and analgesics were administered with little improvement.
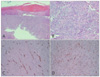
On ultrasonography, a well-circumscribed mass penetrating through the subcutaneous tissue to the fascia was identified (Fig. 1B). The lesion was completely excised under local anesthesia, and we observed intraoperatively that the mass was deep-seated and attached tightly to the fascia, compressing the adjacent tissue. Histopathology revealed typical bland morphology of benign fibrous histiocytoma, showing spindle cells loosely arranged in storiform architecture (Fig. 2A, B). Thickened collagen fibers were seen among cells and the skin appendages disappeared. Immunohistochemistry demonstrated CD34- and CD68+ focally (Fig. 2C, D), vimentin+, smooth muscle actin+, desmin-, S-100-, factor XIIIa+(Fig. 3). Based on the radiologic, histologic and intraoperative findings, we diagnosed deep penetrating BFH. The mass was completely excised and pain subsided gradually. She has been under follow-up without recurrence for 18 months.
Based on location, fibrous histiocytomas are divided into cutaneous and deep-seated subtypes2. Deep-seated BFH is uncommon and accounts for less than 1% of all benign fibrohistiocytomas3. Both cutaneous and deep-seated subtypes are usually asymptomatic. Approximately 5% of deep-seated BFH are associated with pain or tenderness. Although cutaneous BFH poses little diagnostic difficulty, lesions arising in subcutaneous or deep soft tissues are often poorly recognized and diagnosed2. It remains challenging to diagnose deep BFH clinically4, especially when pain coexists, because most BFH are asymptomatic. As such, the diagnosis of deep fibrous histiocytoma is frequently confirmed intraoperatively or on histopathologic examination after excision. We also found it challenging to establish a clinical diagnosis due to throbbing pain that was unresponsive to analgesics.
Preoperative imaging tools, such as ultrasonography, may aid diagnosis and surgery because it shows the location and character of the mass and the adjacent structures, thus minimizing the risk of intraoperative injury of nerves and vessels.
The most important differential diagnoses of BFH are the aggressive forms of fibrohistiocytic neoplasms, including dermatofibrosarcoma protuberans (DFSP), malignant fibrous histiocytoma, and leiomyosarcoma5-7. DFSP especially has very similar histopathologic features with BFH. DFSP is generally characterized by more uniform spindle cells and a more prominent storiform pattern. The epidermis overlying DFSP is usually attenuated or ulcerated, and the tumor has a more infiltrative pattern of growth, showing diffusely positive CD34 staining. Malignant fibrous histiocytoma and leiomyosarcoma exhibit cellular atypia and bizarre giant cells, which are not features of BFH. Further differential diagnoses in our case included dermatomyofibroma. But dermatomyofibroma usually reveals skin appendages, and prominent storiform pattern of tumor cells and thickened collagen bundles are not features of BFH. Specifically, dermatomyofibroma usually does not express factor XIIIa.
The pain of deep-seated dermatofibroma may be due to tumoral nerve invasion or mass effect on the nerve fibers. In our case, pain was thought to be secondary to the latter because the mass was separated from the underlying fascia and the pain gradually subsided after surgery.
Optimal treatment for BFH includes wide excision and continuous follow-up, because local recurrence or metastasis can occur in deep fibrous histiocytoma.
In summary, we report a very rare case of deep penetrating BFH associated with pain. The diagnosis was confirmed after successful surgical excision following preoperative ultrasonography.
Figures and Tables
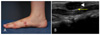 | Fig. 1(A) A painful erythematous nodule was found on the arch of the foot. (B) Well-circumscribed mass from subcutaneous tissue attached to the fascia and compressing the architecture under the fascia (mass: white arrow head, fascia: yellow arrow). |
References
1. Skoulakis CE, Papadakis CE, Datseris GE, Drivas EI, Kyrmizakis DE, Bizakis JG. Subcutaneous benign fibrous histiocytoma of the cheek. Case report and review of the literature. Acta Otorhinolaryngol Ital. 2007. 27:90–93.
2. Gleason BC, Fletcher CD. Deep "benign" fibrous histiocytoma: clinicopathologic analysis of 69 cases of a rare tumor indicating occasional metastatic potential. Am J Surg Pathol. 2008. 32:354–362.

3. Hannachi Sassi S, Trabelsi M, Abid L, Mrad K, Abbess I, Dhouib R, et al. Deep benign fibrous histiocytoma: a case report. Rev Chir Orthop Reparatrice Appar Mot. 2006. 92:809–812.
4. Mentzel T, Kutzner H, Rütten A, Hügel H. Benign fibrous histiocytoma (dermatofibroma) of the face: clinicopathologic and immunohistochemical study of 34 cases associated with an aggressive clinical course. Am J Dermatopathol. 2001. 23:419–426.

5. Calonje E, Mentzel T, Fletcher CD. Cellular benign fibrous histiocytoma. Clinicopathologic analysis of 74 cases of a distinctive variant of cutaneous fibrous histiocytoma with frequent recurrence. Am J Surg Pathol. 1994. 18:668–676.
6. Kaddu S, McMenamin ME, Fletcher CD. Atypical fibrous histiocytoma of the skin: clinicopathologic analysis of 59 cases with evidence of infrequent metastasis. Am J Surg Pathol. 2002. 26:35–46.
7. Fletcher CD. Benign fibrous histiocytoma of subcutaneous and deep soft tissue: a clinicopathologic analysis of 21 cases. Am J Surg Pathol. 1990. 14:801–809.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download