Abstract
In this study, we examined a case where lung cancer metastasized to the vulvar area. A 79-year-old woman that was a heavy smoker was referred to our department with a short (two-week) history of dyspnea, and with a painful nodule on her right labium majora, which she had noticed almost three years earlier. Histopathologically, the specimen appeared as a poorly differentiated squamous cell carcinoma. The chest X-ray, chest computerized tomography scan, and percutaneous transthoracic needle biopsy via bronchoscopy revealed squamous cell carcinoma in the right upper lobe of the lung. Based on these clinical and histopathological findings, we concluded that her condition was skin metastasis at the right labium majora from the lung cancer, which occurs very rarely.
The single most important process characterizing cancer is the ability to produce secondary distant metastasis. Lung cancer metastasizes to almost every organ. However, cutaneous metastasis from lung cancer is rare. Various types of lung cancers have lead to cutaneous metastasis in only 1.5~2.6% of cases1. Cutaneous metastasis from lung cancer has appeared in every area of the skin, but the most common locations are the anterior chest, head, neck, abdomen, and back. However, skin metastasis to the genital area and the extremities is very uncommon. Clinically, lung cancer may be signaled only by cutaneous metastasis, because the primary lung lesion often remains quiescent. In general, skin metastasis is a poor prognostic marker and the patient's medium survival rate is very short.
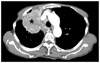
A 79-year-old woman that was a heavy smoker with a short (two-week) history of dyspnea was referred to our department due to a painful nodule on her right labia majora, which the patient had noticed almost three years earlier. Her general condition was good. A cutaneous examination at the time showed a painful erythematous nodule on the right labia majora. The lesion was 3×3 cm is size, round, firm, raised, hemispherical, and covered by an intact epidermis. The adjacent skin contained signs of inflammation, with erythema, oozing, and discharge (Fig. 1). The punch biopsy specimen of the vulvar lesion was shonw to be poorly differentiated squamous cell carcinoma (Fig. 2). After the skin biopsy, she was referred to a pulmonologist for evaluation of dyspnea. A chest X-ray revealed a right upper lobe mass with mediastinal lymphadenopathy. A subsequent computerized tomography scan showed the presence of an ill-defined 7.5×7 cm round hypodense mass in the right upper lobe at low-contrast heterogenous enhancement. In addition, mediastinal and both hilar nodal involvement was also observed (Fig. 3). Pleural effusion was present. A bronchoscopic biopsy showed a moderately differentiated squamous cell carcinoma. Immunohistochemical examination showed lung squamous cell carcinoma and metastatic skin cancer, with the following results: P63, ERCC-1, and cytokeratin 7 immunoreactivity. Moreover, the specimens were negative for transcriptional factor-1. Positron emission tomography scanning using 18F-labeled fluorodeoxyglucose confirmed the presence of a pulmonary lesion, contralateral mediastinal lymph node metastasis, and vulvar metastasis. The patient was diagnosed as having had stage 4 lung cancer. She did not receive chemotherapy and radiotherapy, and only conservative treatment for skin lesion. She expired after six months with no signs of improvement.
Lung cancer, the leading cause of cancer-related deaths in Korea, metastasizes to the skin in only 1.5~2.6% of cases1.
Although any area of the skin can be involved, metastasis occurs primarily near the primary tumor. Common sites of cutaneous metastasis are the anterior chest, head, neck, abdomen, and back; and occurrences on the genital area and the upper and lower extremities are rare2. There have been no case of lung cancer that metastasized to the genital area in Korea, although two cases of metastasis to the perianal area were reported in other countries.
Cutaneous metastasis, as a first sign of internal malignancy, occurs infrequently. Clinically, it manifests as a nodule, ulceration, cellulitis-like lesion, bullae, or fibrotic process. The nodular type is the result of hematogenous metastasis, and is likely to be the most common type3. The lesion observed in this study was the nodular type, but it was a solitary lesion.
Generally, cutaneous metastasis is an early indicator of metastatic disease. At the time of diagnosis of internal malignancy, the incidence of cutaneous metastasis ranges from 0.7 to 9.0%4. Metastatic skin cancer can arise in any stage during the progress of primary cancer, but it usually arises in the terminal stage of the primary cancer1, which indicates poor prognosis. Mostly, metastatic cancer is not found before the primary cancer, but rather is found after or simultaneously with the primary cancer. Generally, skin metastasis of the primary cancer arises within 6~12 months after the primary cancer is found, and 90% of skin metastasis cases arise within five years2. Metastatic cancer may be the first clinical sign and can often be used to help find the primary cancer4. Many reviews by dermatologists noted that in approximately 20~40% of metastatic skin cancer cases, the primary complaint from patients was skin symptoms. Diagnosis may be delayed by several months, unless the skin lesion grows rapidly. Lung cancer, renal cell carcinoma, and ovary cancer are the occult types of primary cancer2. When metastatic cancer occurs in the terminal stage or in the course of treatment, it may be used to predict the prognosis of the patient or indicate that treatment of the primary cancer failed. Thus, we may change the treatment course. In our patient, the metastatic skin cancer was found before the primary cancer, which is rare.
The histological finding of the metastatic skin cancer is usually the same as that of the primary cancer, but occasionally, the differentiation of the metastatic cancer may be lower-grade5,6. In our case, the differentiation of the metastatic cancer was a lower-grade relative to the primary cancer. Skin cancer that has metastasized from the lung often has various histological signatures, including squamous cell carcinoma, adenocarcinoma, and undifferentiated carcinoma. The frequency of occurrence of metastatic skin cancer is usually the same as that of the primary cancer. The most common metastatic cancer in Korea is squamous cell carcinoma, followed by adenocarcinoma, small cell lung cancer, and large cell carcinoma. Park et al.7 and Jeong et al.8 reported that the most common metastatic skin cancer from the lung is squamous cell carcinoma, which occurs in 44% and 71% of cases. However, in other countries, the most common metastatic skin cancer from the lung is adenocarcinoma, followed by squamous cellcarcinoma, small cell lung cancer, and large cell carcinoma.
According to Coslett and Katlic9 and Terashima and Kanazawa10, the primary region on the lung where lung cancer metastasizes from is the upper lobe-i.e., in 65% and 88% of cases, respectively. The reason why most metastatic skin lesions of lung cancer come from the upper lobe is that cancer cells destined for the skin likely travel via the bloodstream. Perhaps the particular milieu in the upper lobes, which is the result of anatomical and gravitational differences that affect blood and lymphatic flow, favors such hematogenous metastasis. In our case, the metastatic skin cancer was determined to be from the upper lobe of the lung.
The prognosis for patients with lung cancer with skin metastasis is very poor because, in general, their disease is advanced and involves other sites such as the brain, liver, bone, and adrenal gland. The average survival period after diagnosis of skin metastasis of lung cancer ranges from 3 to 5 months9,10. In our case, the patient noticed a skin lesion three years earlier, but as she did not have other manifestations, she delayed her diagnostic evaluation, and was diagnosed with lung cancer and metastatic skin cancer at the same time when searching for the cause of her dyspnea, which had happened two weeks earlier. The patient expired six months after the diagnosis of metastatic skin cancer.
Biopsy specimens must be taken from all new skin lesions, particularly in individuals who smoke or who already have a history of lung cancer. Although skin metastasis of lung cancer is rare, dermatologists are likely to see metastatic skin cancers as originating from the lung and should be informed about this phenomenon.
Figures and Tables
Fig. 1
An erythematous nodule 3×3 cm in size on the right labia majora and the adjacent skin in a 79-year-old woman.

References
3. Lookingbill DP, Spangler N, Sexton FM. Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patients. J Am Acad Dermatol. 1990. 22:19–26.
4. Lee CN, You CE, Park HJ, Park CJ, Cho SH, Lee JY, et al. Metastatic cancer of the skin: clinical and histopathological study. Korean J Dermatol. 2002. 40:1212–1218.
7. Park YK, Lee SH, Choi JS, Lee SN, Park CI, Lim NI. Metastatic tumor of the skin. Clinical and histopathologic stury. Korean J Dermatol. 1981. 19:609–615.
8. Jeong SW, Lee SW, Chun JH, Cha SH, Jeong ET, Park SD. Clinicopathological studiesof 7 cases with cutaneous metastatic carcinomas from lung cancers. Korean J Dermatol. 1999. 37:1576–1582.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download