Abstract
Congenital syphilis occurs when Treponema pallidum crosses the placenta during pregnancy or from contact with an infectious genital lesion during delivery. Cutaneous manifestations of congenital syphilis are relatively common, occurring in approximately 30% to 70% of patients. Maculopapular lesions, vesiculobullous lesions, condylomata lata lesions, annular lesions, and erythema multiforme-like targetoid lesions have been reported. We report on a premature newborn with congenital syphilis who presented with generalized bullous and pustular eruption and desquamation at birth.
Congenital syphilis occurs when Treponema (T.) pallidum crosses the placenta during pregnancy or through contact with an infectious genital lesion during delivery1. Congenital syphilis can be detected and treated successfully; however, it continues to be a serious healthcare problem, particularly in developing nations2. Clinical manifestations of congenital syphilis are quite varied and familiarity with the sometimes subtle, nonspecific clinical findings is important. We describe a generalized bullous and pustular eruption in a premature newborn with congenital syphilis, confirmed by polymerase chain reaction (PCR) for T. pallidum.
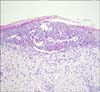
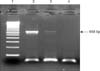
A premature female newborn with a gestational age of 31 weeks (birth weight 1,740 g, height 41 cm) was taken to the neonatal intensive care unit due to respiratory distress and generalized skin eruption, which developed soon after birth. Due to hypoxemia and tachypnea, she required emergent intubation and mechanical ventilator care. Physical examination showed a distended abdomen and hepatosplenomegaly. Multiple discrete yellowish bullae and pustules on the face, trunk, and extremities and generalized desquamation were observed (Fig. 1). The mother was a 20-year-old secundigravida who had not received regular prenatal care. She denied any history of viral infection, drug use, or exposure to teratogens during pregnancy. The clinical differential included bullous impetigo and herpes simplex. Initial laboratory studies demonstrated leukocytosis (41,410/µl; normal, 4,000~10,000/µl), anemia (hemoglobin 11.0 g/dl; normal, 12~16 g/dl), elevated C-reactive protein (1.86 mg/dl; normal, 0~0.3 mg/dl), and raised levels of alanine aminotransferase (57 IU/L; normal, 10~40 IU/L) and direct bilirubin (0.61 mg/dl; normal, 0.05~0.5 mg/dl). Urine analysis revealed hematuria and proteinuria. Serological studies for TORCH (acronym for toxoplasmosis, other agents, rubella, cytomegalovirus, and herpes simplex) infections showed negative results. Results of PCR for herpes simplex virus and varicella-zoster virus from pustules were also negative and pus culture showed no bacterial growth. Histopathologic findings of skin biopsy from the right forearm demonstrated an epidermal pustule filled with neutrophils and eosinophils (Fig. 2). Syphilis serologic studies revealed a reactive Venereal Disease Research Laboratory (VDRL) titer of 1:256, T. pallidum Latex Agglutination (TPLA), and Fluorescent Treponemal Antibody-Absorption test (FTA-ABS) IgM. Cerebrospinal fluid (CSF) examinations showed lymphocytosis (WBC 12/µl, lymphocytes 74%) and elevated protein (240 mg/dl). Immunohistochemistry using primary polyclonal antibodies against T. pallidum (Biocare Medical, Concord, CA, USA) was performed on formalin-fixed paraffin embedded tissues, but spirochetes were not detected. However, PCR for T. pallidum using the gene encoding the 47 kDa major membrane immunogen with pus material showed a faint band of the 658 bp PCR product specific for T. pallidum (Fig. 3). Diagnosis of congenital syphilis was made and parents were examined for syphilis. Both the father and mother had reactive serologic tests for syphilis without clinical manifestations of syphilis (mother - VDRL of 1:32, TPLA-positive, IgM FTA-ABS- negative; father - VDRL of 1:4, TPLA-positive, IgM FTA-ABS-negative). The patient and both of her parents were negative for HIV antibody. Additional evaluations of the patient were subsequently performed; abdominal sonography revealed hepatosplenomegaly with minimal ascites and radiography of the femur showed diffuse bilateral periostitis along the diaphyses.
The patient was treated with intravenous aqueous crystalline penicillin G (50,000 unit/kg) for 14 days. The lesion subsided substantially during the treatment period and there were no neurologic events. Six weeks after treatment with penicillin, the VDRL titer decreased to 1:4. There has been no evidence of recurrence after 6 months of follow up.
Congenital syphilis is an age-old disease that continues to cause substantial morbidity in countries with poor resources. The World Health Organization (WHO) estimates that between 715,000 and 1,575,000 pregnant women are infected with syphilis each year, and a serious adverse pregnancy outcome has been reported in up to 80% of cases2. Congenital syphilis is caused by T. pallidum infection acquired from a mother with untreated or inadequately treated syphilis and it can occur following maternal infection at any stage of a pregnancy1. Estimated rates of vertical transmission in untreated women are 70~100% for primary syphilis, 67% for secondary syphilis, 40~83% for early latent syphilis, and 10% for late latent syphilis3,4.
Congenital syphilis has been divided into early (first 2 years) and late congenital syphilis (after 2 years). Early congenital syphilis can present at any time before 2 years of age; however, it usually presents during the neonatal period, and seldom later than 3~4 months of life. Up to 60% of affected infants are estimated to be asymptomatic at birth, with two-thirds presenting symptoms by 3~8 weeks of age1. Clinical manifestations show significant variation, including prematurity and low birth weight (10~40% of infants). Mucocutaneous lesions are present in as many as 70% of infants and the typical skin eruption consists of small copper-red maculopapular lesions5. They are usually found on the buttock, thighs, palms and soles, and all mucocutaneous lesions and discharge contain abundant spirochetes and are highly contagious. Other variable mucocutaneous manifestations of congenital syphilis have been reported, including vesiculobullous lesions6, condylomata lata lesions7, and annular8 and erythema multiforme-like lesions9. A rare bullous variant, known as syphilitic pemphigus, most commonly occurs on palms and soles, but may be generalized. Pustular eruption may appear on the fingers and toes, and at the angles of the mouth; however, generalized pustules are not common10. Skin lesions in our patient were different from those of syphilitic pemphigus in that initial lesions are generalized bullae and pustules at birth. In cases involving bullous and pustular eruption and histopathologic findings of neutrophilic infiltration, bullous impetigo should be considered for differential diagnosis. However, bacterial culture with bullous fluid was negative and the diagnosis of congenital syphilis could be made through serologic evaluations and PCR. Other findings of early congenital syphilis include hepatosplenomegaly, bone changes seen on X-ray, CSF abnormalities, anemia, jaundice, leukocytosis, respiratory distress, and pseudoparalysis5. Late congenital syphilis occurs in approximately 40% of untreated survivors. The late presentation consists of lesions of the bones (saddle nose, frontal bossing, and tooth malformations), cornea (interstitial keratitis), and central nervous system (seizures, tabes dorsalis), and many of these manifestations are not reversible with antibiotic treatment5.
Clinical examination is important; however, it can sometimes be subtle and nonspecific and many affected infants are asymptomatic at birth1. Therefore, the diagnosis of congenital syphilis can be made by direct identification of treponemes in clinical specimens or by a positive serologic test. Use of diagnostic tests, including enzyme immunoassays, immunoblotting for detection of specific IgM, and PCR have resulted in more sensitive and specific diagnosis of congenital syphilis. In general, bullous fluid contains an abundance of active treponemes and our patient showed positive results on PCR for T. pallidum using the 47 kDa protein gene with pus material.
Congenital syphilis can cause serious adverse effects during various stages of growth, development, and organogenesis of the fetus. Without early diagnosis and adequate antibiotic treatment, it can lead to significant sequelae and even mortality. It should be kept in mind that congenital syphilis may be considered in differential diagnosis of generalized bullous and pustular eruptions at birth and PCR can be a valuable confirmatory diagnostic tool. To the best of our knowledge, our case is the first reported case of congenital syphilis presenting with generalized bullae and pustules confirmed by PCR in pus.
Figures and Tables
References
1. Herremans T, Kortbeek L, Notermans DW. A review of diagnostic tests for congenital syphilis in newborns. Eur J Clin Microbiol Infect Dis. 2010. 29:495–501.

2. The global elimination of congenital syphilis: rationale and strategy for action [Internet]. Sexual and reproductive health. cited 2010 Oct 10. Geneva (Switzerland): World Health Organization;Available from: http://www.who.int/reproductivehealth/publications/rtis/9789241595858/en/index.html.
3. Hollier LM, Harstad TW, Sanchez PJ, Twickler DM, Wendel GD Jr. Fetal syphilis: clinical and laboratory characteristics. Obstet Gynecol. 2001. 97:947–953.

4. Singh AE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev. 1999. 12:187–209.

5. Woods CR. Syphilis in children: congenital and acquired. Semin Pediatr Infect Dis. 2005. 16:245–257.

6. Vural M, Ilikkan B, Polat E, Demir T, Perk Y. A premature newborn with vesiculobullous skin lesions. Eur J Pediatr. 2003. 162:197–199.

7. Karthikeyan K, Thappa DM. Early congenital syphilis in the new millennium. Pediatr Dermatol. 2002. 19:275–276.

8. Agarwal US, Malpani S, Mathur NK. Annular lesions in congenital syphilis. Genitourin Med. 1992. 68:195–196.

9. Wu CC, Tsai CN, Wong WR, Hong HS, Chuang YH. Early congenital syphilis and erythema multiforme-like bullous targetoid lesions in a 1-day-old newborn: detection of Treponema pallidum genomic DNA from the targetoid plaque using nested polymerase chain reaction. J Am Acad Dermatol. 2006. 55:2 Suppl. S11–S15.

10. Sanchez MR. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Syphilis. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1955–1977.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download