Abstract
Precalcaneal congenital fibrolipomatous hamartomas (PCFHs) are characterized clinically by the presence of unilateral or bilateral, asymptomatic nodules in the medial precalcaneal plantar region of the heel. They are skin colored and usually painless nodules. In most patients, the lesions appear within the first few months of life, but they may also be present at birth. Generally PCFHs are benign, but they can grow in proportion to the growth of the infants. Here, we report the case of a 4-month-old boy with a solitary, localized skin-colored nodule on the precalcaneal plantar region of his right heel, diagnosed as a PCFH.
Precalcaneal congenital fibrolipomatous hamartomas (PCFHs) are skin-colored, asymptomatic, subcutaneous nodules on the plantar region of the heel. They may be present at birth or develop during infancy. PCFHs are considered to be uncommon and, to our knowledge, none has been reported to date in Korea. We describe here the case of a 4-month-old boy with a PCFH on the medial, plantar aspect of the right heel and discuss its pathogenesis and differential diagnosis.
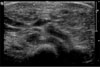
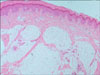
A 4-month-old male infant was referred to us with a soft, asymptomatic, skin-colored nodule on the medial aspect of his right heel. This nodule had been present at birth and became larger in size in proportion to the infant's growth. The child was born by cesarean section at gestational age 36 weeks. His birth weight was 1,760 g, but he had no abnormalities at that time except for the physiologic jaundice of newborns. He subsequently showed normal developmental growth. There was no significant family history of PCFHs. Skin examination showed a small, soft, mobile, non-tender, skin-colored nodule, about 1 cm in diameter, located on the medial, plantar aspect of his right heel, and covered with normal overlying skin (Fig. 1). Ultrasound examination of the plantar region showed a 0.7×0.6 cm ill-defined, homogeneous, slightly hyperechoic lesion near the subcutaneous layer (Fig. 2). There was no infiltration into the underlying structure. Histopathology of a biopsy specimen taken from the right heel showed multiple, lobulated mature adipose tissues protruding into the dermis and separated by collagenous fibrous sheaths (Fig. 3). The nodule was diagnosed as a PCFH and the parents were reassured accordingly.
Since the first description of PCFH in 19901, there have been several case reports of them, mostly in the pediatric dermatology literature. Other names for PCFH include bilateral congenital adipose plantar nodules2, benign anteromedial plantar nodules of childhood3, bilateral congenital fatty heel pads4, and hypertrophic infantile pedal papules5. Although PCFH had been considered to be rare, it may also have been underreported.
PCFH usually occurs in otherwise healthy children, but its incidence and inheritance have not been determined. To date, most cases have been sporadic, but PCFH may show a familial pattern6. This condition is either present at birth or develops over the first few months after birth. Clinically, these lesions are characterized by asymptomatic nodules with normal overlying skin, and they are typically noticed by parents incidentally. Although PCFHs are usually bilateral and symmetrical, they can also be unilateral, as in our patient. PCFHs may become larger in proportion to the growth of the infant or they may maintain the same size. They usually occur on the anteromedial aspect of the heel, but they can also extend onto the heel area. Histologic examination of these lesions shows mature adipose tissue enveloped in collagenous fibrous sheaths. Ultrasound examination of a PCFH reveals a homogeneous mass that shows similar echogenicity as subcutaneous tissue. The natural history of PCFH is difficult to determine because most reports have described changes that occur during the first few years of life, without determining long-term outcomes. In most patients, the lesions persisted without significant changes1,6, although in some they disappear at 2~3 years of age7. There have been no reports of malignancy or gait disturbance caused by PCFH1.
The etiology of PCFH is unclear, but there have been several hypotheses. The first hypothesis suggests that PCFH is associated with a developmental alteration. The fibroconnective trabecular system of the sole develops in the fetal stage and is completely formed during the last months of pregnancy or in the first months after birth1. The fetal heel has been observed to exhibit physiologic hypodermic hypertrophy, indicating that a PCFH may result from incomplete regression of fetal tissue8. Another hypothesis is that PCFH is caused by fat herniation through defects in the plantar fascia4, but these defects have not been observed consistently and the nodules are not reducible. A third hypothesis proposes that PCFH is due to an underlying genetic mechanism caused by autosomal dominant or X-linked inheritance6. Larger studies are needed to determine whether there is a genetic mechanism involved and, if so, the mechanism of inheritance.
The differential diagnosis of PCFH includes piezogenic papules, juvenile plantar fibromatosis, nevus lipomatosus superficialis, calcified nodules, congenital solitary histiocytoma, focal dermal hypoplasia, and congenital hemangioma9. Piezogenic papules are pressure-induced lesions caused by herniation of fat tissue and are only apparent when patients stand. In contrast, the PCFH nodules are present from birth and experiencing them is not related to gravity. The lesions of juvenile plantar fibromatosis are more indurated than those of PCFH, and histologic examination of the former shows fibrous tissue attached to the plantar fascia. The lesion in nevus lipomatosus superficialis are usually distributed linearly on the thigh or hip. Calcified nodules are caused by repeated insertion of needles in the heel to draw blood during the neonatal period. These nodules can be painful, and they show dystrophic cutaneous calcification.
Treatment, other than reassurance, is not required, especially for bilateral nodules. Children with unilateral nodules should be scheduled for re-evaluation after 6 month to determine whether the nodule is getting larger or becoming symptomatic10. Ultrasonography may also be performed during the evaluation. The nodule can be excised surgically if tenderness occurs, although this is rare.
In conclusion, PCFH is a benign condition that does not affect normal activities and usually does not require treatment. Recognition of this condition can avoid unnecessary surgical treatment of the infant and relieve parents' anxieties. Additional case reports and studies are needed to determine the pathologic mechanism and prevalence of PCFH.
Figures and Tables
Fig. 1
Photograph of a solitary, 1 cm, soft, skin-colored nodule on the right medial plantar heel surface in a 4-month-old boy.

References
1. Larralde de Luna M, Ruiz León J, Cabrera HN. Pedal papules in newborn infants. Med Cutan Ibero Lat Am. 1990. 18:9–12.
2. España A, Pujol RM, Idoate MA, Vázquez-Doval J, Romaní J. Bilateral congenital adipose plantar nodules. Br J Dermatol. 2000. 142:1262–1264.

3. Jacob CI, Kumm RC. Benign anteromedial plantar nodules of childhood: a distinct form of plantar fibromatosis. Pediatr Dermatol. 2000. 17:472–474.

4. Livingstone JA, Burd DA. Bilateral congenital fatty heel pads. Br J Plast Surg. 1995. 48:252–253.

5. Conde-Taboada A, Mayo E, González B, Pardavila R, De la Torre C, Cruces M. Hypertrophic infantile pedal papules. Pediatr Dermatol. 2007. 24:339–340.

6. Fangman WL, Prose NS. Precalcaneal congenital fibrolipomatous hamartomas: report of occurrence in half brothers. Pediatr Dermatol. 2004. 21:655–656.

7. Flann S, Munn SE. Precalcaneal congenital fibrolipomatous hamartoma. Clin Exp Dermatol. 2009. 34:495–496.

8. Larregue M, Vabres P, Echard P, Cambazard F. Precalcaneal congenital fibrolipomatous hamartoma. Presented at the Fifth International Congress of Pediatric Dermatology. 1996. 09. Rotterdam, Netherland.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download