Abstract
Acupuncture and cupping have a public reputation as being safe even though these practices can lead to complications such as trauma or infection. We report here on a case of herpes simplex virus (HSV) infection secondary to acupuncture and cupping in a 56-year-old woman. The patient, who had a history of acupuncture and cupping on her left forearm for treating her myalgia, developed painful papules. Histologically, the biopsy specimen showed characteristic ballooning degeneration and inclusion bodies in the epidermis and mid-dermis. These clinical and histological findings were consistent with the diagnosis of HSV infection.
Acupuncture and cupping are traditional methods that are commonly practiced in Oriental medicine, and their origins date back thousands of years. Acupuncture with needles works under the principle that multiple, small needles inserted into the skin will contact tension points and thereby relieve the pain. It is believed that acupuncture can help alleviate back pain, neck pain, cramps, nausea and even help with conditions such as infertility and cancer. Cupping is based on the principle of suction and has been found to affect the body up to four inches deep into the tissue, causing a release of toxins, activation of the lymphatic system, clearance of colonic blockages and clearance of arteries, veins and capillaries. In the previous reports, the adverse effects secondary to acupuncture and cupping have been related to trauma and infection1-9.
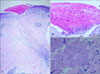
A 56-year-old woman presented with painful skin lesions on her left forearm and she had a history of pain and myalgia in that arm for several months. Three days prior to presentation, the patient had been treated with acupuncture and cupping for a painful left elbow. On the physical examination, multiple polygonal, erythematous papules were observed on the left forearm (Fig. 1). The patient had no personal or family history of recurrent cutaneous herpes. A skin biopsy of the left forearm showed characteristic ballooning degeneration and inclusion bodies in the epidermis and mid-dermis along the track left by the acupuncture needle (Fig. 2). The diagnosis of HSV infection secondary to acupuncture and cupping was made based on the patient's clinical history, the physical exam and the histologic features on the skin biopsy.
HSV is an enveloped, double-stranded DNA virus that contains a linear DNA core of approximately 150-kilobase pairs10,11. Herpes viral diseases are widespread and they affect nearly 80% of human adults. These infections often persist in latent form during the lifetime of the host. The HSV can be transmitted through direct exposure of mucous membranes or abraded skin to the lesions or from the mucosal secretions of an individual with an active primary or recurrent infection12,13. In fact, HSV type I can remain viable on skin, clothing or plastic for short periods of time, and this facilitates transmission through close contact such as kissing on the cheek or sharing equipment14,15. Clinically, the characteristic vesicular lesions or painful papular lesions can inoculate elsewhere on the body and recurrent infections can be triggered by stress, illness, ultraviolet radiation and physical trauma12.
The word "acupuncture" is derived from the Latin words "acus" meaning needle, and "pungere" meaning to prick. Acupuncture involves the insertion and manipulation of fine, filiform needles into specific points on the body with the aim of relieving pain and providing therapy. The practice originated in China and it dates back thousands of years. Other practices in traditional Chinese medicine include cupping (the application of glass cups on skin to create a vacuum), moxibustion (the burning of sticks or cones on acupuncture sites) and electropuncture. Acupuncture and cupping are currently widely used in Asia and they have a public reputation for being safe for the treatment of various pain-related conditions such as myalgia, arthralgia and postherpetic neuralgia.
However, significant and serious adverse events associated with acupuncture have been reported by clinicians. These complications can be classified into four categories; dermatologic complications (factitial panniculitis, prurigo pigmentosa, erythema nodosum, pseudolymphoma, basal cell carcinoma, mycobacterium infection and cutaneous herpes), trauma (pneumothorax, hemothorax, cardiac tamponade, deep vein thrombosis and pseudoaneurysm), infection (hepatitis B, HIV, auricular chondritis, endocariditi and meningitis) and miscellaneous events (collapse, seizure and asthma exacerbation) (Table 1)1-9.
Our patient had a recent history of acupuncture and cupping on the site that had developed the skin lesions, as was seen on the physical examination. Histologically, the skin biopsy showed typical viral inclusion bodies in the epidermis and mid-dermis following the placement of the acupuncture needle. We theorize that our patient acquired cutaneous herpes from direct viral inoculation via a contaminated acupuncture needle or reactivation of a cutaneous herpes viral infection due to mechanical trauma. According to the previous reports, the transmission of infection was by a septic needle and the allergic contact dermatitis was caused by an acupuncture needle containing gold, silver or copper. In this case, the possibility of allergic contact dermatitis was excluded by the characteristic histopathologic findings such as ballooning degeneration and viral inclusion bodies. We have described here a rare case of HSV infection secondary to acupuncture and cupping, and this was diagnosed on the basis of the clinical and histologic findings.
Figures and Tables
Fig. 1
Multiple polygonal, erythematous papules with the traces of the cupping and acupuncture done on the patient's left forearm. (A) Biopsy site (arrow). (B) Cupping site (double circles) and acupuncture site (arrows).

References
1. Brouard M, Kaya G, Vecchietti G, Chavaz P, Harms M. Basal cell carcinoma of the earlobe after auricular acupuncture. Dermatology. 2002. 204:142–144.

2. Chang TW. Letter: Activation of cutaneous herpes by acupuncture. N Engl J Med. 1974. 291:1310.
3. Inoue T, Katoh N, Kishimoto S. Erythema nodosum induced by the synergism of acupuncture therapy and flu-like infection. J Dermatol. 2005. 32:493–496.

4. Lee JS, Ahn SK, Lee SH. Factitial panniculitis induced by cupping and acupuncture. Cutis. 1995. 55:217–218.
5. Bork K. Multiple lymphocytoma at the point of puncture as complication of acupuncture treatment. Traumatic origin of lymphocytoma. Hautarzt. 1983. 34:496–499.
6. Ryu HJ, Kim WJ, Oh CH, Song HJ. Iatrogenic Mycobacterium abscessus infection associated with acupuncture: clinical manifestations and its treatment. Int J Dermatol. 2005. 44:846–850.

7. Saw A, Kwan MK, Sengupta S. Necrotising fasciitis: a life-threatening complication of acupuncture in a patient with diabetes mellitus. Singapore Med J. 2004. 45:180–182.
8. Tanii T, Kono T, Katoh J, Mizuno N, Fukuda M, Hamada T. A case of prurigo pigmentosa considered to be contact allergy to chromium in an acupuncture needle. Acta Derm Venereol. 1991. 71:66–67.
9. Kim KJ, Lee MW, Choi JH, Sung KJ, Moon KC, Koh JK. CD30-positive T-cell-rich pseudolymphoma induced by gold acupuncture. Br J Dermatol. 2002. 146:882–884.

10. Nadelman CM, Newcomer VD. Herpes simplex virus infections. New treatment approaches make early diagnosis even more important. Postgrad Med. 2000. 107:189–195. 199–200.
12. Fatahzadeh M, Schwartz RA. Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management. J Am Acad Dermatol. 2007. 57:737–763.

13. Simmons A. Clinical manifestations and treatment considerations of herpes simplex virus infection. J Infect Dis. 2002. 186:Suppl. 1. S71–S77.

14. Blondeau JM, Embil JA. Herpes simplex virus infection: what to look for. What to do! J Can Dent Assoc. 1990. 56:785–787.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download