Abstract
Lichen planus pigmentosus-inversus is a rare variant of lichen planus pigmentosus. The eruption of lichen planus pigmentosus-inversus occurs mainly in the flexural regions and presents with brownish macules and patches. Here we describe the case of a 31-year-old Korean woman who presented with hyperpigmented lesions over her antecubital and popliteal area and groin. Physical examination revealed multiple brownish macules and patches on the intertriginous area without pruritis, and histologic findings showed a regressive pattern of lichen planus. These clinical and histological findings were consistent with a diagnosis of lichen planus pigmentosus-inversus.
Lichen planus pigmentosus (LPP)-inversus, a variant of LPP, is a rare disease that occurs mainly in the flexural areas1. Clinically it is characterized by the insidious onset of dark-pigmented macules and patches with or without pruritus. We now report a rare case of LPP-inversus in a 31-year-old woman. As far as we know, 17 cases have been reported in the world literature1-6.
A 31-year-old Korean woman presented with asymptomatic brown macules and patches of 5 years' duration located in the axillae, groin, and antecubital and popliteal fossae. The lesions initially began as a few small, asymptomatic macules clustered in the axilla, approximately 5 years prior to presentation. Over the last 2 years, the lesions increased in number and spread to affect the antecubital and popliteal fossae and groin. She denied any preceding erythema, pruritus, or vesicles before the appearance of hyperpigmentation. There was no previous history of medication use or trauma and no family history of pigmentary disorders.
On physical examination, there were multiple brownish macules and patches located in the intertriginous areas several millimeters to centimeters in diameter (Fig. 1). The larger lesions had a linear or annular configuration and the long axis of the linear lesions followed the lines of cleavage (Fig. 1A, B).
Biopsy of the macules in the antecubital fossae was done. Histologic examination revealed a regressive pattern of lichen planus with absent hyperkeratosis and hypergranulosis and a nearly atrophic epidermis. Hydropic degeneration of the epidermal basal layer was subtle but pigment incontinence was strongly expressed. The lymphocytic inflammatory infiltrate in the upper dermis was mild (Fig. 2).
Laboratory studies including a complete blood count, urinalysis, and liver and renal function tests were within normal limits.
LPP is an uncommon variant of chronic lichen planus that is characterized by hyperpigmented, dark-brown macules in sun-exposed areas and flexural folds that present both with and without pruritus. Kanwar et al.7 reported a study of 124 Indian patients with LPP wherein the face and neck were most commonly affected by hyperpigmentation. Flexural involvement including the axilla (8.9%), inframammary folds (6.5%), and groin (3.2%) was seen less frequently. Vega et al.8 published a clinicopathologic study of 11 cases of LPP describing distributions primarily in the face (73%) and trunk (45%). The axillary and inguinal folds were only affected in two patients. Several other studies have shown that the localization of LPP is typically not predominantly intertriginous9-11.
Pock et al.1 described seven central European Caucasians with LPP-inversus as a variant of LPP arising in intertriginous areas. The eruption of LPP-inversus occurs mainly in the flexural regions, including the axilla, infra-mammary, groin, popliteal and antecubital areas. Further, Kashima et al.3 recently reported two Japanese cases of LPP-inversus occurring in the axilla, groin, and popliteal fossae. The basic clinical and histologic data from reports of LPP-inversus are summarized in Table 11-6. Our case presented with asymptomatic brown macules and patches in the flexural areas showing a strong incontinence of pigment and a mild lymphocytic infiltrate in the upper dermis. Pock et al.1 proposed a possible morphogenesis of LPP-inversus wherein the lichenoid reaction occurs within a short period of time with dramatically intensive hydropic degeneration of basal keratinocytes. During this time, the compensatory increased proliferation of keratinocytes cannot develop as in typical lichen planus such that the papules transform quickly into brown macules. The predominant clinical lesion is macular and a histologic finding of intensive pigment incontinence is frequently identified. Our patient presented with chronic macular lesions that had been present for five years, which is likely why hydropic degeneration of the basal layer was subtle and the intensive lichenoid inflammatory reaction was absent.
The differential diagnosis includes ashy dermatosis and pigmented contact dermatitis. In the past, ashy dermatosis was thought to be the same condition as LPP. However, Vega et al.8 reported clinical differences between ashy dermatosis and LPP including the presence or absence of pruritis and lesion color. Pigmented contact dermatitis is a non-eczematous variant of contact dermatitis, characterized clinically by hyperpigmentation caused by common allergens such as fragrances, preservatives and deodorants. Our patient had no medication history and no reported contact of flexural areas with common allergens. The treatment of LPP-inversus is unknown. Some authors reported that the lesions gradually disappeared without medication within several months3. The paraneoplastic nature of LPP was described previously12. But there have been no reports of LPP-inversus associated with internal malignancy.
In conclusion, we have described a rare case of LPP-inversus in a Korean patient with diagnosis based on intertriginous location and histologic findings.
Figures and Tables
Fig. 1
Multiple annular or linear hyperpigmented macules and patches with a smooth surface. Some of the lesions followed the lines of cleavage. (A) Lesions on the axillae and antecubital fossae. (B) Lesions on the groin. (C) Lesions on the popliteal fossae.

Fig. 2
Histologically, pigment incontinence is diffusely expressed and lymphocytic infiltrate in the upper dermis is mild (H&E, ×100).
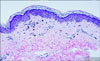
Table 1
Summary of clinical and histologic data for patients with LPP-inversus

LPP-inversus: lichen planus pigmentosus-inversus, A: incontinence of pigment is strongly expressed, B: inflammatory infiltrates with lymphocytes and histiocytes in the upper dermis were slight, C: inflammatory infiltrates with lymphocytes and histiocytes in the upper dermis were moderate, D: hydropic degeneration of the basal layer of epidermis, E: intensive lichenoid inflammatory reaction.
References
1. Pock L, Jelínková L, Drlík L, Abrhámová S, Vojtechovská S, Sezemská D, et al. Lichen planus pigmentosus-inversus. J Eur Acad Dermatol Venereol. 2001. 15:452–454.

2. Kim BS, Aum JA, Kim HS, Kim SJ, Kim MB, Oh CK, et al. Coexistence of classic lichen planus and lichen planus pigmentosus-inversus: resistant to both tacrolimus and clobetasol propionate ointments. J Eur Acad Dermatol Venereol. 2008. 22:106–107.

3. Kashima A, Tajiri A, Yamashita A, Asada Y, Setoyama M. Two Japanese cases of lichen planus pigmentosus-inversus. Int J Dermatol. 2007. 46:740–742.

4. Muñoz-Pérez MA, Camacho F. Pigmented and reticulated plaques of folds. A case of lichen planus pigmentosus-inversus? Eur J Dermatol. 2002. 12:282.
5. Bennàssar A, Mas A, Julià M, Iranzo P, Ferrando J. Annular plaques in the skin folds: 4 cases of lichen planus pigmentosus-inversus. Actas Dermosifiliogr. 2009. 100:602–605.

6. Kim BS, Park KD, Chi SG, Ko HC, Lee WJ, Lee SJ, et al. Two cases of lichen planus pigmentosus-inversus arising from long-standing lichen planus-inversus. Ann Dermatol. 2008. 20:254–256.

7. Kanwar AJ, Dogra S, Handa S, Parsad D, Radotra BD. A study of 124 Indian patients with lichen planus pigmentosus. Clin Exp Dermatol. 2003. 28:481–485.

8. Vega ME, Waxtein L, Arenas R, Hojyo T, Dominguez-Soto L. Ashy dermatosis and lichen planus pigmentosus: a clinicopathologic study of 31 cases. Int J Dermatol. 1992. 31:90–94.

9. Ozden MG, Yildiz L, Aydin F, Senturk N, Canturk T, Turanli AY. Lichen planus pigmentosus presenting as generalized reticulate pigmentation with scalp involvement. Clin Exp Dermatol. 2009. 34:636–637.

10. Namazi MR. Lichen planus pigmentosus presenting as diffuse facial melanosis. J Drugs Dermatol. 2004. 3:436–437.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download