Abstract
Background
Pincer nail is a nail deformity characterized by transverse overcurvature of the nail plate. Pincer nail can affect a patient's quality of life due to its chronic, recurrent course; however, there have been no clinical studies on the pincer nail condition in Korean patients.
Objective
The purpose of this study was to characterize the clinical findings and treatment of pincer nail. In addition, possible etiological factors were considered, and treatment efficacy was evaluated.
Methods
The medical records and clinical photographs of 35 patients (12 males, 23 females) who were diagnosed with pincer nail between August 1, 2005 and July 31, 2009 were studied.
Results
Patient age ranged from 10 to 77 (52.09±17.26) years, and there was a predominance of female (23 out of 35 patients, F:M=2:1). The mean duration of the disorder was 7.45 years (range 0.25~40); 85% had pincer nail for at least 1 year. In addition, 40% had a history of previous treatment and recurrence. There were 82.8% patients with the common type of pincer nails. The most commonly involved nails were both great toenails. Among 35 patients, nail grinding was started in 30 patients, and 25 patients showed clinical improvement with nail grinding. The width index increased and the height index decreased after treatment. The mean follow up period was 8.42 months (range 1~27), and 7 patients showed recurrence after 8.8 months (range 2~20). Among 35 patients, 5 patients were treated with nail extraction with matricectomy, and the symptoms resolved immediately. The mean follow up period was 7.6 months (range 0~19), and recurrence was not observed. Onychomycosis was also present in 37.1% of patients, and itraconazole pulse therapy for 3 months was added.
Conclusion
The results of this study demonstrate the clinical features of pincer nail in Korean patients. The findings show that the common type of pincer nail was most common, and nail grinding as a conservative treatment greatly improved pincer nails despite a risk of recurrence. When onychomycosis was also present, oral antifungal therapy added to nail grinding resulted in a more rapid change in nail thickness and clinical improvement.
Pincer nail is a nail dystrophy characterized by an increase in the transverse curvature along the longitudinal axis of the nail. Pincer nail was first reported in 1950 by Frost1, using the term "incurvated nail". Cornelius and Shelley2 introduced the term "pincer nail" in 1968. Although ingrown nails are confused with pincer nails, the pincer nail is differentiated from ingrown nails by its abnormal shape of decreasing width and increasing height of the nail plate; the ingrown nail has a normal shape3.
The etiology of pincer nails is unknown. There are various reports of pincer nails, including hereditary and acquired cases4. Poorly fitting shoes has been suggested as one of the most common causes of pincer nails5. Tumors of the nail apparatus or tinea unguium may also lead to pincer nails6-8. Pincer nail deformities can occur with systemic or other skin disease9-11. However, the mechanism explaining the association is not clearly understood.
There is no standard treatment for pincer nail. Several treatment methods, including conservative approaches and surgical methods, are used. Surgical therapy can produce a satisfactory result in cases with severe deformity; however, that invasive approach may cause severe discomfort. Conservative therapy requires a longer treatment period but causes less discomfort. Among the conservative procedures including application of urea, placement of a plastic brace, and grinding of the nail plate, nail grinding was preferred as the initial therapeutic choice in this study. The rate of response was evaluated by measuring the width and height index.
Although pincer nails often have a chronic course and can interfere with quality of life, there have been no clinical studies on this nail deformity in Korea. Therefore, the clinical features and treatments of patients with pincer nails were retrospectively reviewed in this study.
Patient information was collected retrospectively from medical records between August 1, 2005 and July 31, 2009 at the Nail clinic of Yeouido St. Mary's Hospital, Catholic University of Korea. Thirty-five patients diagnosed with pincer nail and their photographs were included in the review.
The patients were grouped into three clinical types proposed by Baran et al.5: the common type, the plicated type, and the tile type (Fig. 1). First, the common type is characterized by an increase in the transverse curvature from the proximal to distal nail, which may form a trumpet or omega shape. Second, the plicated type presents with the lateral edges sharply vented to form a vertical sheet. The lateral edges can press into the lateral nail groove and produce granulation tissue, mimicking an ingrown nail. Third, the tile type is rare and characterized by an even greater increase in the transverse curvature along the longitudinal axis of the nail plate, forming a tile shape.
Possible etiologic factors were evaluated by reviewing the medical record. In addition, patients were divided by treatment methods: nail extraction or nail grinding. Nail grinding was performed for symptomatic patients with pincer nail. The entire nail surface, except for the margin, was abraded with a high-speed grinder (Sae Yang Machinery Co. Gwangju, Korea) until the nail became flexible. Nail grinding was performed every one or two months until the symptoms resolved with flattening of the plate (end of treatment). Nail extraction and matricectomy was performed only when the patient complained of severe pain with inflammation or when the nail grinding had failed. In addition, when onychomycosis was also present, oral antifungal therapy (pulse therapy with itraconazole for three months) was added to the treatment at the same time.
According to the numerical method proposed by Kosaka et al. (Fig. 2)12, the width, height, and length of the nail plate were measured at each visit. From that data, the following indices were calculated: (1) width index [width of the nail tip/width of the nail root ×100] and (2) height index [height of the nail tip/width of the nail tip ×100]. Although the normal range of those indices is not known, a width index closer to 100 percent indicates wider nails, whereas values approaching 0 percent indicate more tapered nails. In addition, a height index of 0 percent indicates flatter nails, whereas higher values indicate curved nails. Among 35 patients, only 11 patients had complete records of the width and height index. To analyze the therapeutic response to nail grinding treatment in 11 patients, the change of width and height index after treatment was compared. The relationship between changes of indices after treatment and total grinding numbers to get those changes were analyzed to check if it was possible to standardize the efficacy of nail grinding treatment. Also, in comparing the treatment efficacy, to eliminate the bias introduced by thickening of the nail plate from onychomycosis, patients were subdivided by whether they had onychomycosis or not.
All of the analyses were performed using the statistics program SAS system ver. 9.1 (SAS Institute, Cary, NC, USA). Overall changes of width/height index after grinding treatment were analyzed by the paired t test. In addition, a coefficient of correlation was calculated using the Spearman correlation to identify whether the total number of grinding treatments in each patient correlated with the amount of differences in the width/height indices in each patient. Significance was defined as p values <0.05.
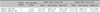
Patient age ranged from 10 to 77 (52.09±17.26) years, with a predominance of females (23 of 35 patients, F:M =2:1). The mean age at diagnosis of pincer nail was 42.83±10.47 years (male) and 45.61±40.77 years (female). The mean duration was 7.45±8.5 years; 30 patients had pincer nail for at least one year, and 14 were previously treated for pincer nail (including 10 patients treated with simple nail extraction and 4 patients treated with nail grinding) and had a recurrence. Among 35 patients with pincer nail, 29 had the common type, five had the plicated type and one had the tile type. The most commonly involved nails were both great toenails. Reviewing the nail charts, 13 patients had onychomycosis in addition to pincer nails, nine patients had a history of poorly fitting shoes, two patients had psoriasis, and one patient had an osteophyte of the distal phalanx (Table 1).
Nail grinding treatment significantly improved the signs and symptoms of pincer nail (Fig. 3). Nail grinding was started in 30 (85.7%) patients, and four of them were lost to follow up. Among 26 patients, one patient did not respond to grinding therapy and was treated with nail extraction. Twenty-five (96.1%) patients showed clinical improvement with nail grinding, and only 11 of them had complete records of the width and height indices of the nail plate before and after treatment. Statistical analysis of those 11 patients showed that the width index increased (p<0.05) after treatment, whereas the height index decreased (p<0.05) after treatment in each of the patients (Table 2). The mean follow up period was 8.42 months (range 1~27), and 7 (28%) patients showed recurrence after a mean period of 8.8 months (range 2~20). Nail extraction and matricectomy was initially performed in five (24.3%) patients who presented with severe discomfort and required immediate relief from pain. The symptoms resolved immediately after nail extraction. The mean follow up period was 7.6 months (range 0~19), and recurrence was not observed in this period.
Pincer nail with onychomycosis responded faster to the concurrent therapy of nail grinding and oral antifungal agents than pincer nail without onychomycosis. We analyzed width and height indices of 11 patients who had complete records before and after treatment. Among those 11 patients, seven had additional onychomycosis and four did not. In patients with onychomycosis, the initial mean width and height indices were 71.4±15.7 and 71.3± 27.6. In patients without onychomycosis, the initial mean width and height indices were 75.1±7.6 and 37.1±17.8 (Fig. 4A). The mean grinding numbers to reach the end of treatment were 3±1.4 in patients with onychomycosis and 3.3±0.5 in patients without onychomycosis (Fig. 4B). The mean width differences after treatment in the patients with onychomycosis and those without onychomycosis were 16.0±12.8 and 12.5±6.9, respectively. The mean height differences in those with onychomycosis and those without onychomycosis were 41.7±20.8 and 17.4±11.6, respectively. Those findings show a relatively higher height index difference with statistical significance (p<0.05) in patients with onychomycosis compared to the patients without onychomycosis (Table 3). Those results show that the change of thickness with grinding was greater in patients with onychomycosis than without onychomycosis. We can assume that the difference may be caused by combined antifungal therapy.
In 11 patients with complete records of the width and height indices, the relationship of the numbers of grinding procedures and the extent of index changes were analyzed. Because the sample size was small, we did not divide those 11 patients according to whether onychomycosis was combined or not. The Spearman correlation coefficient calculated for the width difference and numbers of grinding procedures was -0.01758 (p>0.05); the positive correlation was without statistical significance. The Spearman correlation coefficient for the height difference and grinding numbers was -0.12808 (p>0.05); that negative correlation was without statistical significance. That result shows that responses to grinding therapy between patients were variable, and it is difficult to quantify the effect of each grinding session.
In this study, only two patients developed pincer nails in childhood. Both of them showed pincer nails of both great toenails. However, familial involvement, associated anomalies, or congenital diseases suggesting a hereditary pincer nail were all denied. All of other cases were pincer nails that sporadically occurred in adult patients. Onychomycosis, ill-fitting shoes, psoriasis, and an osteophyte of the distal phalanx were associated findings. Although there are some reports of hereditary pincer nails13,14, most of the cases of previously reported pincer nails are sporadic, consistent with the results of this study. Most cases of pincer nail are thought to be due to mechanical deformation of the nail plate. Ill-fitting shoes and osteophytes in this study could be classified as such mechanical factors. The thickening of the nail plate caused by onychomycosis may cause mechanical forces to develop a pincer nail. That is supported by the finding of a previous report that the pincer nail improved after oral antifungal therapy7. It is possible that the pincer nail caused the nail plate to be more susceptible to fungal infection; however, further study is needed to confirm this possibility. Psoriasis is known to cause various nail changes, including oil spots, onycholysis, and trachyonychia. However, whether psoriasis caused pincer nail or it was simply an associated finding requires confirmation.
Nail grinding significantly improved pincer nails in this study. Among 14 patients who had a history of previous treatment of pincer nails, ten were treated with simple nail extraction on repeat treatment. With regard to conservative or surgical treatments of pincer nails15-20, most recent reports have focused on new surgical techniques. Indeed, surgical techniques including nail matricectomy or correction of the nail bed show excellent long-term treatment outcome. Conservative methods can be difficult to use in cases of severe deformity; they require a long treatment period with high recurrence rate. However, many patients prefer non-invasive treatment, even if there is a risk of recurrence because of discomfort caused by surgery. In addition, conservative methods can be easily used without special equipment at local clinics. Nail grinding is one such non-invasive technique; nail grinding has been successfully used for pincer nails since 199016,17. Even though there have been reports of new surgical techniques with long lasting results19-21, many patients undergo simple nail extraction for repeat treatment. Those methods may relieve symptoms until the nail grows in again.
Patients with pincer nails and onychomycosis received oral antifungal therapy at the same time. The treatment response to nail grinding appeared to be faster than in patients without onychomycosis. Therefore, the patients were divided into groups with and without onychomycosis. The initial mean height index was about 1.5 times higher in the onychomycosis group compared to patients without onychomycosis, while the mean number of grinding procedures for complete improvement was lower in the onychomycosis group. Those results suggest that antifungal therapy enhanced the rate of improvement of pincer nails by possibly reducing the thickness of the nail plate. However, further study is needed for confirmation.
An increase in the width index and a decrease in the height index were observed in each patient after nail grinding with clinical improvement. However, that index did not correlate with the severity of symptoms among the patients. For example, patient 13 showed 20% of the width index and 260% of the height index; however, she had mild symptoms. On the other hand, patient 32 showed 85.7% of the width index and 28.6% of the height index; he complained of severe pain due to an ingrown nail plate. Therefore, as well as the numerical index, variable morphology should be considered when comparing patients with pincer nails. In addition, the attempts to quantify the efficacy of nail grinding showed that the correlation of the number of grinding procedures and the changes of the width and height index were not statistically significant.
In summary, the results of this study provide general clinical information about pincer nails in Korean patients. In addition, an objective measurement method was introduced. The method discussed can be easily used to follow patients in the clinical setting.
Figures and Tables
Fig. 3
(A) Improvement of pincer nail after three sessions of nail grinding, (B) Improvement of pincer nail after nail extraction with matricectomy.

Fig. 4
Comparison of the initial mean width/height indices (A) and mean grinding numbers (B) in 11 patients with onychomycosis and without onychomycosis having complete records before and after therapy.

References
1. Frost L. Root resection for incurvated nail. J Natl Assoc Chiropodists. 1950. 40:1928.
3. Kosaka M, Kusuhara H, Mochizuki Y, Mori H, Isogai N. Morphologic study of normal, ingrown, and pincer nails. Dermatol Surg. 2010. 36:31–38.

4. Baran R, Dawber RPR. Diseases of the nail and their management. 2001. 3rd ed. Boston, MA: Blackwell Science;496–499.
5. Baran R, Haneke E, Richert B. Pincer nails: definition and surgical treatment. Dermatol Surg. 2001. 27:261–266.

6. Baran R, Broutart JC. Epidermoid cyst of the thumb presenting as pincer nail. J Am Acad Dermatol. 1988. 19:143–144.

7. Higashi N. Pincer nail due to tinea unguium. Hifu. 1990. 32:40–44.
8. Hwang SM, Lee SH, Ahn SK. Pincer nail deformity and pseudo-Kaposi's sarcoma: complications of an artificial arteriovenous fistula for haemodialysis. Br J Dermatol. 1999. 141:1129–1132.

9. Greiner D, Schöfer H, Milbradt R. Reversible transverse overcurvature of the nails (pincer nails) after treatment with a beta-blocker. J Am Acad Dermatol. 1998. 39:486–487.

10. Liao YC, Lee JY. Psoriasis in a 3-month-old infant with Kawasaki disease. Dermatol Online J. 2009. 15:10.
11. Kirkland CR, Sheth P. Acquired pincer nail deformity associated with end stage renal disease secondary to diabetes. Dermatol Online J. 2009. 15:17.

12. Kosaka M, Kamiishi H. New strategy for the treatment and assessment of pincer nail. Plast Reconstr Surg. 2003. 111:2014–2019.

13. Chapman RS. Letter: overcurvature of the nails--an inherited disorder. Br J Dermatol. 1973. 89:317–318.
14. Mimouni D, Ben-Amitai D. Hereditary pincer nail. Cutis. 2002. 69:51–53.
15. Kim KD, Sim WY. Surgical pearl: nail plate separation and splint fixation--a new noninvasive treatment for pincer nails. J Am Acad Dermatol. 2003. 48:791–792.

16. Maeda N, Mizuno N, Ichikawa K. Nail abrasion: a new treatment for ingrown toe-nails. J Dermatol. 1990. 17:746–749.

17. Roh DK, Lee DW, Cho BK. A case of heredetary pincer nail treated with nail grinding method. Korean J Dermatol. 1997. 35:971–974.
18. Arai H, Arai T, Nakajima H, Haneke E. Formable acrylic treatment for ingrowing nail with gutter splint and sculptured nail. Int J Dermatol. 2004. 43:759–765.

19. Lane JE, Peterson CM, Ratz JL. Avulsion and partial matricectomy with the carbon dioxide laser for pincer nail deformity. Dermatol Surg. 2004. 30:456–458.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download