Abstract
Granuloma annulare (GA) is a common, benign, chronic inflammatory disorder, which is characterized by grouped papules in an enlarging annular shape. It has been described in several clinical subtypes, including localized, generalized, subcutaneous, perforating, and erythematous types. Even though generalized, subcutaneous, and perforating types of GA are unusual, there are several reports of those types. However, erythematous or patch GA, has not been reported yet in the Korean literature. Herein, we report a 42-year-old woman with pruritic erythematous patches, which occurred on the extremities without preceding event, and showed typical clinical and histopatologic findings of erythematous GA.
Granuloma annulare (GA) is an idiopathic, chronic inflammatory disorder found in all ages. The lesion is characterized by grouped papules in an enlarging annular shape, with color ranging from flesh-colored to erythematous. The unusual variants of GA include generalized, perforating, erythematous, and subcutaneous GA1. Erythematous GA appears as erythematous to brownish patches, with or without scales, which may or may not have an annular configuration on the trunk and extremities2.
In contrast to several reports of generalized, perforating, and subcutaneous GA, no case of erythematous GA has been reported in the Korean literature. Herein, we report the first case of GA presenting as erythematous patches in the Korean literature.
A 42-year-old woman presented with an 1-year history of pruritic lesions on the both legs and left forearm. The lesions began as small erythematous patches. Prior to visiting our hospital, the patient was treated with oral antihistamine and topical corticosteroid. When the lesions were small, they responded well to the therapy and showed complete remission. But when the lesions recurred, they increased in diameter and number and did not respond to the previously administered therapy any more.
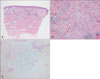
The physical examination showed five, round to oval, erythematous patches on the both lower legs and left forearm (Fig. 1). The patient was otherwise in good health. The biopsy sample from the left lower leg revealed a moderate superficial and mid-dermal interstitial infiltrate of both lymphocytes and histiocytes, and mucin deposition between the collagen fibers. Alcian blue (pH 2.5) staining revealed mucin deposition among the degenerated collagen fibers (Fig. 2). Based upon the clinical and histopathological findings, a diagnosis of erythematous GA was made. The patient was treated with oral antihistamine, topical corticosteroid, and intralesional injection of triamcinolone acetonide. After 6 weeks, all lesions improved but did not disappear completely.
GA is a common skin disorder in which smooth papules are arranged as annular forms. There are several clinical variants of GA: localized, generalized, subcutaneous, perforating, and erythematous or patch types. Usually, there is overlap between subtypes and more than one morphologic type may be seen in the same patient3. Our patient had a rare, recently described GA variant, named erythematous GA. It appears as asymptomatic erythematous to brownish patches, with or without scales, which may or may not have an annular configuration on the trunk and extremities. However, there may be some mild pruritus. Female predominance has been reported, as with other forms of GA2. Our female patient had several pruritic, round to oval, erythematous patches, without scales on the extremities.
The exact etiology and pathogenesis of GA have not been fully elucidated. Several predisposing factors have been implicated. These include insect bite4, sun exposure5, BCG vaccination6, and herpes virus infection7. There is also a possible association with some drugs, such as allopurinol, diclofenac, quinidine, intranasal calcitonin, and amlodipine8. In this case, the patient denied any medication history, recent vaccination history, and insect bite history, and had no problem, except the skin lesions.
Histopathologically, GA shows infiltrate of histiocytes and perivascular infiltrate of lymphocytes. The histiocytes may be present in an interstitial pattern, both between and around collagen bundles, and around blood vessels or in palisades surrounding areas with prominent mucin. Increased mucin, which is highlighted by both colloidal iron and Alcian blue stains, is the hallmark of GA. In cases related to drug reactions, eosinophils and some lichenoid changes at the dermal-epidermal interface are observed2. The various types of GA share similar histopathologic findings and the interstitial pattern predominates in the erythematous or patch variants, as seen in our case9,10.
Clinically, the erythematous GA can be mistaken for other skin conditions, such as morphea, erythema annulare centrifugum, and parapsoriasis. In our case, hypersensitivity reaction and eczema were diagnostic considerations at the time of biopsy. Histopathologically, the interstitial type of GA can be confused with xanthoma, drug reaction, and rarely, with Mycobacterium marinum infection. In our case, the absence of foamy histiocytes, interface changes, and neutrophils, allowed us to exclude those conditions from the diagnosis.
Erythematous GA was reported to respond to the same treatment as other types of GA2. The attempted treatments include topical and oral glucocorticoids, cryotherapy, hydroxychloroquine, dapsone, niacinamide, cyclosporine, chlorambucil, isotretinoin, and PUVA photochemotherapy11,12. Our patient was treated with oral antihistamine, topical corticosteroid, and intralesional injection of triamcinolone acetonide, and showed improvement after 6 weeks. However, the lesions did not disappear completely.
Figures and Tables
Fig. 2
(A) A moderate superficial and mid-dermal interstitial and perivascular infiltrate of mononuclear cells (H&E, ×40). (B) An interstitial infiltrate of lymphocytes and histiocytes, and mucin deposition between the collagen bundles (H&E, ×200). (C) Alcian blue pH 2.5 staining showed the deposition of increased bluish material between the degenerated collagen fibers (×100).
References
2. Coelho R, Carvalho R, Rodrigues A, Afonso A, Cardoso J. Patch-type granuloma annulare. Eur J Dermatol. 2009. 19:285–286.

3. Prendiville JS. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Granuloma annulare. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;369–373.
5. Stankler L, Leslie G. Generalized granuloma annulare. A report of a case and review of the literature. Arch Dermatol. 1967. 95:509–513.

6. Houcke-Bruge C, Delaporte E, Catteau B, Martin De Lassalle E, Piette F. Granuloma annulare following BCG vaccination. Ann Dermatol Venereol. 2001. 128:541–544.
7. Shideler SJ, Richards M. Granuloma annulare arising after herpes zoster. J Am Acad Dermatol. 1986. 15:1049–1050.

8. Sanli HE, Koçyiğit P, Arica E, Kurtyüksel M, Heper AO, Ozcan M. Granuloma annulare on herpes zoster scars in a Hodgkins disease patient following autologous peripheral stem cell transplantation. J Eur Acad Dermatol Venereol. 2006. 20:314–317.

9. Lim AC, Hart K, Murrell D. A granuloma annulare-like eruption associated with the use of amlodipine. Australas J Dermatol. 2002. 43:24–27.

10. Ogino A, Tamaki E. Atypical granuloma annulare. Transition from erythema to multiple type. Dermatologica. 1978. 156:97–100.
11. Gamo Villegas R, Sopena Barona J, Guerra Tapia A, Vergara Sanchez A, Rodríguez Peralto JL, Iglesias DIez L. Pustular generalized perforating granuloma annulare. Br J Dermatol. 2003. 149:866–868.

12. Morita K, Okamoto H, Miyachi Y. Papular elastolytic giant cell granuloma: a clinical variant of annular elastolytic giant cell granuloma or generalized granuloma annulare? Eur J Dermatol. 1999. 9:647–649.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download