Abstract
Blastomycosis-like pyoderma is a rare, vegetating skin lesion that is an unusual exaggerated tissue reaction possibly to prolonged primary or secondary bacterial infection. We report a case of blastomycosis-like pyoderma in a man with Down syndrome, diabetes mellitus and hypothyroidism who responsed poorly to conventional therapies, including antibiotics and correction of predisposing factors for a long time, but experienced dramatic improvement after 3 months of acitretin treatment.
Blastomycosis-like pyoderma is an unusual, exaggerated, tissue reaction and usually only occurs in patients who are locally or systemically immunocompromised1. The lesion consists of large, indurated, verrucous plaques. Histopathologically, the lesion is characterized by pseudoepitheliomatous hyperplasia and intraepidermal, subepidermal neutrophilic microabscesses1. Although bacteria are likely to play a major role, response to antibiotics varies greatly2. We report a case of blastomycosis-like pyoderma responding poorly to classic treatment, but responsed dramatically to treatment with acitretin. It may be thought that acitretin provides healing through anti-proliferative and anti-inflammatory action. Acitretin should be considered a good adjuvant modality for the treatment of blastomycosis-like pyoderma.
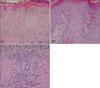
A 33 year-old man presented to our clinic in December 2008 with verrucous cutaneous plaques on both ankles. He had been treated many times with occlusive dressing using topical steroid, antihistamines, antibiotics and antifungal agents by several dermatologists for 2 years before admission. These therapies resulted in some improvement but eventually the lesion deteriorated and spreaded. The patient's past medical history included diabetes mellitus and hypothyroidism since the age of 23 and 28 years, respectively. He also suffered mental retardation due to Down syndrome since birth. There was no history of trauma, consumption of bromides, and tuberculosis. Dermatologic examination revealed pruritic, irregular, lichenified verrucous plaques on both ankles and the right foot dorsum (Fig. 1). The lesion had elevated borders, extremely thick scales and excoriated hemorrhagic ulcers focally. Histopathologic examination of the biopsy specimen taken from verucous plaque showed pseudoepitheliomatous hyperplasia, neutrophil exocytosis, and papillary dermal microabscesses (Fig. 2A, B). In addition, perivascular and interstitial inflammatory infiltrates composed of lymphocytes, histiocytes, neutrophils, plasma cells, and eosinophils were observed in the dermis (Fig. 2C). No fungal elements were detected with periodic acid-Schiff stain. Bacterial culture of the tissue specimen revealed Staphylococcus aureus. Fungal and mycobacterial cultures were negative, and repeated KOH examinations of the scales at 1-month interval showed no hyphae or spores. On the basis of these findings, blastomycosis-like pyoderma was diagnosed after excluding other diseases, such as lichen simplex chronicus, deep fungal and mycobacterial infections, bromoderma and neutrophilic dermatoses.
The patient was treated with antihistamines and daily oral antibiotics. There was no clinical response after 8 weeks and antibiotics were stopped. He was then given a daily oral dose of acitretin 20 mg, mequitazine 10 mg, bepotastine 20 mg, and gamma linoleic acid 80 mg with topical application of urea cream. After 3 months of therapy, the lesion resolved and only a mild scar was visible (Fig. 3). The total duration of treatment was 8 months, and there were no adverse events associated with the treatment regimen, or evidence of recurrence for 9 months.
Blastomycosis-like pyoderma most likely represents vegetating hyperinflammatory tissue reaction in a cutaneous environment with reduced immunological capacity2. This disease of unknown etiology is believed to be associated with an excessive inflammatory reaction in response to bacterial infections, tattoos, foreign body reaction, halogens and immunodeficiency3-5, such as diabetes mellitus, malnutrition, alcoholism, malignancy, HIV infection, and ulcerative colitis4-6.
In the skin lesions of the patients with blastomycosis-like pyoderma, Staphylococci, Streptococci, Pseudomonas, Escherica coli, anaerobes and Candida species can be cultured7. Among them, S. aureus is the most common8. Some authors believe that the microbiological agent is not primarily responsible for the condition and the infection develops secondary to immune dysfunction8,9. The condition fails to respond to antibiotic treatment alone, which supports this theory8,10.
The characteristic lesions are large, crusted, verrucous plaques with pustules and well-defined and raised borders11. These lesions are usually localized in the face, scalp, axilla, trunk, and distal extremities.
The histopathologic hallmarks of blastomycosis-like pyoderma are pseudo-epitheliomatous hyperplasia, intraepidermal, subepidermal microabscesses and dense dermal inflammatory infiltration11,12. There is usually no granuloma formation.
The diagnostic criteria for blastomycosis-like pyoderma have been proposed as follows13: 1) large verrucous plaques with multiple pustules and elevated borders, 2) pseudoepitheliomatous hyperplasia with abscesses in tissue biopsy specimens, 3) growth of at least one pathogenic bacterium, 4) negative cultures for deep fungi and mycobacteria, 5) normal serum bromide levels. Our patient met all these criteria. Serum halogen levels were not performed because there was no suggestion of halogen exposure in the history.
The differential diagnoses of the disease include North American blastomycosis, chromoblastomycosis, pyoderma gangrenosum, pemphigus vegetans, tuberculosis verrucosa cutis, halogenoderma, and squamous cell carcinoma3,12,14.
Numerous treatment modalities have been used, including topical and/or systemic antibiotics, retinoids, dapsone, cyclosporine, systemic corticosteroids, intralesional steroids, surgical excision, cryosurgery and carbon dioxide laser15. There is no standard treatment modality. In Korean dermatological literatures, Choi et al.16 reported that treatment of blastomycosis-like pyoderma includes early bacterial culture with proper antibiotics, dressing with copper sulfate or aluminium subacetate, triamcinolone intralesional injection, zinc oxide, and disodium chromoglycate. Our treatment options can be summarized as follows: correction of the underlying disease, apply appropriate supportive wound care, administer specific antimicrobial, antihistamines and systemic retinoid therapy. Antibiotics were ineffective despite bacteria were isolated from tissue cultures, similar to previous reports of variable or poor response to antibiotics2,17. There are reports of acitretin being used for treatment of blastomycosis-like pyoderma2,18. Acitretin showed remarkable therapeutic effect and our patient's lesions resolved after 3 months of therapy. Acitretin is a second generation retinoid and has specific biological activities that resemble those of vitamin A, such as anti-proliferative and anti-inflammatory activities2,19.
We reported the therapeutic efficacy of acitretin in blastomycosis-like pyoderma unresponsive to antibiotics and topical steroids. Moreover, on the basis of the favorable adverse-effect profile of low-dose acitretin treatment, we recommend acitretin as the drug of choice for the treatment of blastomycosis-like pyoderma.
Figures and Tables
Fig. 1
(A) Lichenified verrucous plaques with hemorrhagic ulcers on both ankles and right foot dorsum. (B) Close up view.

Fig. 2
(A) Histologic examination shows hyperkeratosis, pseudoepitheliomatous hyperplasia and dense inflammatory infiltrates in upper dermis (H&E, ×40). (B) The magnified view shows papillary dermal microabscess and neutrophil exocytosis (H&E, ×200). (C) Periappendageal dense mixed inflammatory infiltration of plasma cells and a few eosinophils (H&E, ×200).
References
1. Dutta TK, James J, Baruah MC, Ratnakar C. Blastomycosis-like pyoderma in a case of chronic myeloid leukaemia. Postgrad Med J. 1992. 68:363–365.

2. Nguyen RT, Beardmore GL. Blastomycosis-like pyoderma: successful treatment with low-dose acitretin. Australas J Dermatol. 2005. 46:97–100.

3. Bianchi L, Carrozzo AM, Orlandi A, Campione E, Hagman JH, Chimenti S. Pyoderma vegetans and ulcerative colitis. Br J Dermatol. 2001. 144:1224–1227.

4. Harish K, Varghese T, Najeeba R, Harikumar R. Pyoderma vegetans and ulcerative colitis. J Postgrad Med. 2006. 52:302–303.
6. Brinkmeier T, Frosch PJ. Pyodermatitis-pyostomatitis vegetans: a clinical course of two decades with response to cyclosporine and low-dose prednisolone. Acta Derm Venereol. 2001. 81:134–136.

7. Sawalka SS, Phiske MM, Jerajani HR. Blastomycosis-like pyoderma. Indian J Dermatol Venereol Leprol. 2007. 73:117–119.

8. Adişen E, Tezel F, Gürer MA. Pyoderma vegetans: a case for discussion. Acta Derm Venereol. 2009. 89:186–188.
9. Skorepová M, Stuchlík D. Chronic pyoderma vegetans triggered by Trichophyton mentagrophytes. Mycoses. 2006. 49:143–144.

11. Vesić S, Bogdanovic A, Medenica L, Bremec T, Pavlović MD. Pyoderma vegetans in a patient with myelodysplastic syndrome. Int J Dermatol. 2009. 48:665–666.

12. Papadopoulos AJ, Schwartz RA, Kapila R, Samady JA, Ruszczak Z, Rao BK, et al. Pyoderma vegetans. J Cutan Med Surg. 2001. 5:223–227.

14. Konstantopoulou M, O'Dwyer EM, Steele JC, Field EA, Lewis MA, Macfarlane AW. Pyodermatitis-pyostomatitis vegetans complicated by methicillin-resistant Staphylococcus aureus infection. Clin Exp Dermatol. 2005. 30:666–668.

15. Su O, Demirkesen C, Onsun N. Localized blastomycosis-like pyoderma with good response to cotrimoxazole and cryotherapy. Int J Dermatol. 2004. 43:388–390.

16. Choi HU, Sung KH, Lee WW, Bae JH, Lee SK. A case of blastomycosis-like pyoderma. Korean J Dermatol. 2003. 41:936–939.
17. Rongioletti F, Semino M, Drago F, Blangetti MG, Rebora A. Blastomycosis-like pyoderma (Pyoderma vegetans) responding to antibiotics and topical disodium chromoglycate. Int J Dermatol. 1996. 35:828–830.

18. Lu XL, Zhao W, Xia YK, Chen J, Wang L, Zhou XW, et al. Good response of a combined treatment of acitretin and antibiotics in blastomycosis-like pyoderma. Eur J Dermatol. 2009. 19:261–262.

19. Pilkington T, Brogden RN. Acitretin. A review of its pharmacology and therapeutic use. Drugs. 1992. 43:597–627.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download