Abstract
Erythema nodosum is a common variant of panniculitis. It is characterized by tender erythematous nodule and plaque on the anterior aspect of the leg. The etiology is not fully understood. It may be associated with a variety of disorders, including infection, medication, autoimmune disorders, pregnancy, and malignancy. A 33-year-old Korean woman presented with 1 week history of painful erythematous plaques on both knees. She was 7 weeks pregnant with assisted reproductive therapy, and had been maintained on daily intramuscular progesterone injection for 4 weeks. Histological examination of the lesions revealed septal panniculitis without vasculitis. Two days after discontinuing progesterone injection, the symptoms and lesions started to resolve. Herein we present a case of erythema nodosum caused by progesterone injection for endometrial preparation.
Erythema nodosum is a common form of panniculitis. Typically, they are tender erythematous nodules and raised plaques on the anterior aspects of legs. The etiologic factors and pathogenesis are not yet fully understood. Erythema nodosum is associated with a variety of clinical conditions, including infection, medication, autoimmune disorders, pregnancy, and malignancy. It is well-known that the etiology of erythema nodosum is associated with female sex hormones - estrogen and progesterone1. As pregnancies conceived through assisted reproductive therapy increase, we predict that the incidence of erythema nodosum in women who underwent assisted reproductive therapy will increase. We herein report a case of erythema nodosum caused by progesterone injection for endometrial preparation.
A 33 year-old Korean woman presented with a 1-week history of painful erythematous plaques on both knees. Physical examination showed symmetric, tender, erythematous plaques on the anterior aspects of both knees (Fig. 1A). Pain was aggravated by exercise, particularly during walking. Although the lesions were warm, she had no fever. She was systemically well in the seventh week of her first pregnancy. She had never used oral contraceptives. She had become pregnant after undergoing assisted reproductive therapy. Intramuscular injection of progesterone (50 mg) had been administered daily for to enable endometrial preparation for 4 weeks. There was no history of upper respiratory infection before her presentation. She had only received hormonal assisted reproductive therapy. We noted thickened septa with infiltrated inflammatory cells without evidence of vasculitis (Fig. 2A). There were also inflammatory cells in the periseptal areas of the fat lobules (Fig. 2B).
We diagnosed our patient with erythema nodosum following histopathological evaluation. Intramuscular progesterone therapy was ceased and instead she began to receive vaginal topical progesterone (Crinone gel®). Two days after discontinuing intramuscular progesterone injection, clinical improvement was observed (Fig. 1B). The lesions started to resolve, and the color of lesions became darker and more brown. We added acetaminophen treatment. Progesterone continued to be administered for endometrial preparation in the following manner: 4 weeks intramuscularly and 3 weeks topically to the vagina. At the time of preparing this publication, there has been no evidence of recurrence.
Erythema nodosum is the most frequent clinicopathologic variant of septal panniculitis2. Since first described in 1798, various etiologic factors have been identified: streptococcal infections, sarcoidosis, autoimmune disorders, inflammatory bowel diseases, drugs such as oral contraceptives3 and malignancy1,4. Nevertheless, the etiology cannot be confirmed in 37 to 60% of cases of erythema nodosum4.
In a prospective study of 132 patients diagnosed with erythema nodosum, hormonal factors during pregnancy and oral contraceptives were the causes of 10% of cases1. This is not the only evidence to suggest that female sex hormone is related to erythema nodosum. After puberty, erythema nodosum follows a female predominance, but before puberty, the sex incidence is approximately equal4. In addition, there are cases of erythema nodosum in the course of hormone replacement therapy in postmenopausal women5 and after aromatase inhibitor administration in breast cancer patients6.
If then, which factor of female sex hormones could cause erythema nodosum? The concentrations of these hormones are thought to be critical in the development of erythema nodosum7. There was no report of erythema nodosum associated with high-dose estrogen salvage therapy for metastatic breast cancer, while low-dose hormone replacement therapy in postmenopausal women can cause erythema nodosum5. Furthermore, erythema nodosum commonly occurs during the first trimester of gestation, but not in the third trimester. In addition, erythema nodosum has been observed in breast cancer patients treated with aromatase inhibitors, which suppresses plasma estrogen levels6. This presented case demonstrates that sole progesterone therapy can cause erythema nodosum. The fact that skin lesions began to resolve after commencing topical progesterone, which led to reduction in serum progesterone concentration although not measured clinically, is consistent with this hypothesis. Therefore, we suggest that the concentration of progesterone or the ratio between estrogen and progesterone is more important in the pathogenesis of erythema nodosum than the concentration of estrogen alone.
Keratinocytes from overlying epidermis in erythema nodosum lesions were negative for both estrogen and progesterone receptors, like other normal human skin8. However, the expression levels of progesterone receptor in other tissues of erythema nodosum patients remain unknown. It has not been confirmed whether the effect of progesterone in erythema nodosum is direct or indirect. Further studies will be needed to address these questions. Progesterone is critical in the process of endometrial preparation to maintain pregnancy. Either insufficient progesterone concentration or insufficient progesterone response may lead to pregnancy loss. A recent study shows that normal endometrium is highly sensitive to very low levels of progesterone9. Furthermore, no statistically significant benefit has been observed in intramuscular progesterone administration over topical administration to vagina10. Since the quantity of hormones in oral contraceptives has been decreased after the 1980s, erythema nodosum caused by oral contraceptive is now rare. Nowadays, the use of assisted reproductive therapy has become popular. The advancement of related technology will hopefully lead to reduced dosage of progesterone required for endometrial preparation, and consequently lessen the incidence of erythema nodosum, as was the case with oral contraceptives.
To our knowledge, assisted reproductive therapy-induced erythema nodosum has never been reported. However it should be considered as a possible adverse event in assisted reproductive therapy.
Figures and Tables
 | Fig. 1(A) Symmetric, tender, erythematous plaques on the anterior aspects of both knees. (B) Two days after discontinuing intramuscular progesterone injection, the color of the lesions became darker and then started to resolve. |
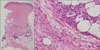 | Fig. 2(A) Scanning power view showing thickened and edematous septa of the subcutaneous tissue with inflammatory infiltrate, and the infiltrate extends to the periphery of the adjacent fat lobules (Lt. knee, H&E, ×40), (B) Higher magnification shows aggregations of small histiocytes (Lt. knee, H&E, ×400). |
References
1. Psychos DN, Voulgari PV, Skopouli FN, Drosos AA, Moutsopoulos HM. Erythema nodosum: the underlying conditions. Clin Rheumatol. 2000. 19:212–216.

3. Foldes EG. Pharmaceutical effect of contraceptive pills on the skin. Int J Clin Pharmacol Ther Toxicol. 1988. 26:356–359.
5. Yang SG, Han KH, Cho KH, Lee AY. Development of erythema nodosum in the course of oestrogen replacement therapy. Br J Dermatol. 1997. 137:319–320.
6. Jhaveri K, Halperin P, Shin SJ, Vahdat L. Erythema nodosum secondary to aromatase inhibitor use in breast cancer patients: case reports and review of the literature. Breast Cancer Res Treat. 2007. 106:315–318.

7. Bombardieri S, Munno OD, Di Punzio C, Pasero G. Erythema nodosum associated with pregnancy and oral contraceptives. Br Med J. 1977. 1:1509–1510.

8. Im S, Lee ES, Kim W, Song J, Kim J, Lee M, et al. Expression of progesterone receptor in human keratinocytes. J Korean Med Sci. 2000. 15:647–654.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download