Abstract
Background
Objective
Methods
Results
Figures and Tables
Fig. 1

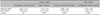
Table 1

Age and sex distribution between different therapeutic groups is shown here. Each p-value stands for the statistical significance level of the difference between the group that utilized the specific modality and the rest of the sample. For instance, the mean age of the group that received the combined therapy of cryotherapy and immunotherapy is 18.3 years old, and shows no statistically significant deviation from that of the patients who did not receive immunotherapy. Statistical evaluation was performed with the Student's t-test (p-value<0.05). M: male, F: female. 5FU: 5-Fluorouracil.
Table 2
Before adjusting for confounders (i.e. the number of wartsand the total treatment period), the patients who were also treated with immunotherapy paradoxically required more sessions of cryotherapy, but the difference was not statistically significant. After adjustment, the combined therapeutic group needed far less cryotherapy sessions (mean 3.58), compared with those without immunotherapy (mean 5.10) The adjustment was done with ANCOVA (*p-value<0.05). DPCP: diphencyclopropenone.
Table 3
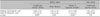
Before adjustment, the patients who applied 5FU/Salicylic acid with cryotherapy paradoxically required more cryotherapy sessions (mean 6.31) than the rest of the sample (mean 4.03). After adjusting for confounders, there was no statistical difference in the mean number of cryotherapy sessions between the investigated groups (*p-value<0.05). 5FU: 5-Fluorouracil.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download