Abstract
Perifollicular fibroma (PFF) is a very rare proliferative lesion of the perifollicular sheath. A flesh-colored, dome-shaped papulonodule is usually located on the face or the neck. These papulonodules may be single or multiple. Histologically, the lesion consists of a concentric arrangement of cellular fibrous tissue around a normal hair follicle. We describe here an unusual case of PFF in a 41-year-old female who had an asymptomatic small skin colored papule on the scalp, and this is an uncommon location for PFF.
Perifollicular fibroma (PFF) is a rare cutaneous hamartoma that shows differentiation in the connective tissue sheath of hair follicles1. It can occur as a solitary papule or as multiple lesions2. Multiple PFF lesions have been linked to adenomatous colonic polyps and they may be inherited as an autosomal dominant trait3. Histologically, the lesion consists of a concentric arrangement of cellular fibrous tissue around a normal hair follicle4. To the best of our knowledge, most reports have described multiple PFF lesions involving the scalp. A solitary PFF lesion on the scalp is a very rare phenomenon1,5.
We herein report on a case of a solitary PFF lesion arising from the scalp of a 41-year-old female.
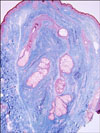
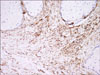
A 41-year-old woman presented with an asymptomatic dome-shaped cutaneous papule on the scalp, and she'd had this lesion for 5 years. The lesion had started as a tiny papule that had slowly enlarged. Her past medical and family history was unremarkable. On physical examination, a 0.5×0.5 cm sized, single, soft flesh colored papule was noted on the scalp (Fig. 1). An excision biopsy was taken. Histopathologic examination of the excised specimen showed concentric layers of fibrous connective tissues around a well-formed hair follicle and a mild mononuclear infiltrate in the perifollicular area (Fig. 2). Masson's trichrome staining showed its marked perifollicular sheath (Fig. 3). The perifollicular spindle cells were positive for CD34 (Fig. 4). The elastic tissue staining was negative. The diagnosis of PFF was made based on these findings. No evidence of recurrence was noted after a follow-up period of 10 months.
Perifollicular fibroma (PFF) was first described by Burnier and Rejsek6 in 1925. It is characterized by skin-colored, dome-shaped, smooth, firm, 1 to 5 mm sized papules7. They mostly present on the face and neck region1. Multiple PFFs may be associated with Birt-Hogg-Dubé syndrome and internal diseases such as colonic polyps, polyposis and cancer. The lesion in our case was a solitary small, soft, skin-colored papule located on the scalp. PFF is a very rare disease whether it presents as a single lesion or multiple lesions1. This is an interesting case because the diagnosis could have been missed. Solitary PFF usually presents on the face and neck, and involvement of the scalp is extremely rare5.
The etiology is currently unclear, but several hypotheses have been proposed. Zackheim and Pinkus2 suggested a neoplastic origin. Freeman and Chernosky8 observed the ultrastructure of a PFF that was present at birth in a male infant and this supported the hypothesis of a tumor derivation as opposed to a reactive etiology. But the possibility that a PFF may simply represent a fibroblastic response to previous follicular inflammation can not be excluded.
Headington9 described that some PFFs represent an exaggerated response to inflammation or irritation. Balfour and Smoller5 also supported the theory of reactive fibroplasia.
Histopathologically, PFF shows concentric proliferations of collagen fibers surrounding a normal hair follicle. The differential diagnoses include fibrofolliculoma, trichodiscoma, fibrous papule, dermatofibroma and neurofibroma10,11. In contrast to PFF, a distorted hair follicle in fibrofolliculoma is surrounded by a fibrous stroma. Multiple thin, anastomosing bands of follicular epithelium extend into the stroma. Trichodiscoma and fibrous papule do not show a concentric arrangement of perifollicular collagen12. Dermatofibroma is comprised of spindle cells that show no predilection for the follicle, and dermatofibroma lacks an epithelial component11. Neurofibroma exhibits a collection of bland spindle cells with elongated, wavy nuclei and wavy collagenous strands, and this lesion shows no particular association with the hair follicle11. Meticulous assessment of serial sections of the specimen is important to arrive at a definitive diagnosis for suspected cases because the histologic features of PFF do not encompass uniform changes in all hair follicles7,13.
Elastic stain could help to determine the origin of the lesion. It has been suggested that reduced elastic fibers with collagenous overgrowth can represent a neoplastic process5. The immunohistochemical features of PFF, which consist of CD34-positive spindle cells and factor XIIIa-positive dendritic cells within the connective tissue component, could be associated with preceding inflammatory conditions in PFF7. In our case, we could not identify any preceding events that could have led to inflammation, and the histology showed an accentuated perifollicular sheath and a marked decrease in elastin. These findings may represent a tumor derivation rather than a reactive etiology.
We report here on a rare case of solitary PFF that occurred on the scalp of a 41-year-old Korean woman.
Figures and Tables
Fig. 2
The hair follicle is surrounded by a dense concentric fibrous sheath (A: H&E, ×40, B: H&E, ×100).

References
3. Sasai S, Takahashi K, Tagami H. Coexistence of multiple perifollicular fibromas and colonic polyp and cancer. Dermatology. 1996. 192:262–263.

4. Junkins-Hopkins JM, Cooper PH. Multiple perifollicular fibromas: report of a case and analysis of the literature. J Cutan Pathol. 1994. 21:467–471.

5. Balfour E, Smoller BR. Exogenous trauma simulating perifollicular fibromas. Am J Dermatopathol. 2005. 27:42–44.

6. Burnier MM, Rejsek P. Fibromas sores-cutaneus peripilaries multiples die. Corr Bull Soc Franc Dermatol Syphiligr. 1925. 32:46–49.
7. Ogawa E, Okuyama R, Tagami H, Aiba S. Perifollicular fibroma: a case successfully diagnosed with deeply cut sections. J Dermatol. 2008. 35:126–128.

9. Headington JT. Tumors of the hair follicle. A review. Am J Pathol. 1976. 85:479–514.
11. Collins GL, Somach S, Morgan MB. Histomorphologic and immunophenotypic analysis of fibrofolliculomas and trichodiscomas in Birt-Hogg-Dube syndrome and sporadic disease. J Cutan Pathol. 2002. 29:529–533.

12. Ahmed TSS, Priore JD, Seykora JT. Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Tumor of the epidermal appendages. Lever's histopathology of the skin. 2009. 10th ed. Philadelphia: Lippincott Williams & Wilkins;851–909.
13. Lee DW, Park JS, Choi SW, Cho BK. A case of perifollicular fibroma. Korean J Dermatol. 1993. 31:999–1002.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download