Abstract
Chronic bullous disease of childhood (CBDC) is an autoimmune blistering disease that is characterized by Immunoglobulin A (IgA) deposits at the basement membrane zone. IgA autoantibodies (aAbs) from the serum of patients with CBDC react with antigens of 97 kDa (LABD97) and 120 kDa (LAD-1), and both of which are fragments of the extracellular domain of bullous pemphigoid 180 (BP180, type XVII collagen). The CBDC sera reacts with the immunodominant NC16a domain of BP180, which is the major region recognized by IgG aAbs in patients with bullous pemphigoid. A five-year-old boy presented with multiple pruritic tense blisters on the umbilical and inguinal areas for six weeks. The direct immunofluorescence of the perilesional area demonstrated linear deposits of IgA at the basement membrane zone. Using immunoblotting and an enzyme linked immunosorbent assay (ELISA), we identified the IgA aAbs reactive to antigens with a molecular weight of 120 kDa (LAD-1), which is a fragment of the extracellular domain of BP180.
Chronic bullous disease of childhood (CBDC) is a rare bullous disorder that is characterized by linear deposits of Immunoglobulin A (IgA) at the basement membrane zone1-9. CBDC sera contain IgA autoantibodies (aAbs) against two different dermal and epidermal associated antigens that have molecular weights of 285 kDa and 97/120 kDa, respectively1. IgA aAbs from CBDC sera react with antigens of 97 kDa (LABD97) and 120 kDa (LAD-1), and both of which are fragments of the extracellular domain of bullous pemphigoid 180 (BP180, type XVII collagen). CBDC sera react with the immunodominant region of BP180NC16a, which is a major target of IgG aAbs produced by patients with bullous pemphigoid (BP)10,11. Immunoblotting analysis of this patient's sera revealed a corresponding antigen with a molecular weight of 120 kDa. In addition, the sera also reacted with the NC16a domain of BP 180 according to enzyme linked immunosorbent assay (ELISA). Here, we report on a case of CBDC that was reactive to 120 kDa antigens (LAD-1).
A five-year-old boy presented with multiple pruritic tense blisters on the umbilical and inguinal areas for the previous six weeks. The skin lesions were present for several days and then they ruptured spontaneously. There was no family history of cutaneous disease and no history of upper respiratory tract infections or drug intake prior to the onset of blistering. The physical examination revealed that the bullae developed on an erythematous base at the umbilicus and inner thigh in clusters of tense bullae (Fig. 1). The lesions initially developed on the umbilicus and they subsequently spread to the inner thigh. The hairs, nails and mucous membranes were intact. The abnormal laboratory results included eosinophilia (7.5%, normal range: 0~5), lymphocytosis (54.9%, normal range: 20~40) and an elevated white blood cell count (12,900 cells/mm3, normal range: 4,800~10,800). Other tests, including the renal and liver function tests, urine analysis, chest X-ray and complement tests (C3, C4), were within the normal limits.
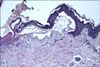
Histopathology from the skin of a vesicle showed subepidermal blisters and mild inflammatory cellular infiltrates in the upper dermis (Fig. 2). Direct immunofluorescence (IF) study of the perilesional area demonstrated linear deposits of IgA at the dermoepidermal junction and no deposits of IgG or C3 (Polyclonal rabbit anti-human IgA, IgG and C3c/FITC; Dako, Glostrup, Denmark). The indirect IF test using human foreskin as a substrate (incubated in 1M NaCl to induce separation of the tissue through the lamina lucida) showed IgA aAbs bound only to the epidermal side of the lamina lucida, at a titer of 1:20 (Fig. 3). Immunoblotting analysis of the sera using epidermal extracts showed IgA antibodies (Polyclonal rabbit anti human IgA/HRP; Dako, Glostrup, Denmark) bound to 120 kDa antigens (Fig. 4). ELISA was conducted to identify the circulating aAbs reactive to the NC16a domain of BP180. The ELISA was positive (19.032 U/ml) against the antigens for the recombinant proteins of BP180NC16a (BP180NC16a ELISA kit, Medical and Biological Laboratories, Nagoya, Japan), but ELISA was otherwise negative with BP230, Dsg1 and Dsg3 (BP230 ELISA kit, MESACUP Desmoglein TEST "Dsg 1" and "Dsg 3"; Medical and Biological Laboratories, Nagoya, Japan).
The patient was initially treated with dapsone 50 mg and prednisolone 10 mg daily. The doses were gradually decreased over three weeks. The lesions completely resolved within three weeks of starting treatment, but they recurred three months after discontinuation of the drugs. Over the next 10 months following treatment, the lesions recurred three times despite administration of additional oral medication.
CBDC is a chronic acquired subepidermal blistering disease of childhood that is characterized by homogeneous linear deposits of IgA at the epidermal basement membrane1-9. It is the most common acquired immunobullous diseases in children with an onset usually before five years of age; it most frequently remits by six to eight years of age.
LAD-1 is one target antigen among several potential antigens associated with CBDC10-13. In this case, we used IF, immunoblotting assay and ELISA to identify the target antigen of this patient and this all revealed that the serum was reactive to LAD-1. CBDC is considered a type of linear IgA bullous dermatosis (LABD) of childhood3. IgA aAbs from the sera of patients with LABD react with 97 kDa (LABD97) and 120 kDa (LAD-1) antigens, and both are degradation products of the extracellular domain of BP180.
BP180 was first identified as a major antigen target of IgG aAbs produced by patients with BP. The amino-terminal domain of BP180 is localized in the cytoplasm whereas the carboxy-terminus projects to the extracellular space and spans the lamina lucida of the basement membrane zone10,11. The NC16a domain of BP180 is the major region recognized by IgG aAbs in patients with BP. It is the major non-collagenous extracellular domain located downstream from the transmembrane domain.
In patients with LABD, antigens are distributed beneath the hemidesmosome or just on the lamina densa and/or beneath it10-14. LABD has been associated with two major binding patterns with regard to a patient's IgA aAbs. Indirect IF on NaCl-split skin has shown that most LABD sera of the lamina lucida type react with the epidermal side, and some LABD sera of the sublamina densa type react with the dermal side. Most patients with the lamina lucida type of LABD demonstrate IgA aAbs against the LABD97 and LAD-112-14. This patient had linear deposits at the epidermal side on the indirect IF with using NaCl-split skin, and this was consistent with the findings common to LABD.
Immunoblotting assay showed that the IgA aAbs were bound only to the 120 kDa antigens. In addition, the ELISA, which is a more sensitive assay, was positive for the recombinant antigen proteins of BP180NC16a and it was negative for BP230, Dsg1 and Dsg3. These findings suggest that the 120 kDa antigen in the immunoblotting assay was a fraction of the BP180, which was positive on the ELISA. In other hand, there is a report of CBDC that was reactive not to NC16a, but only to the Col1513. If our case had showed a negative result to BP18016a, then we would evaluate the association with Col15.
The majority of patients with CBDC are treated with either sulfapyridine or dapsone therapy. Dapsone is started at 1~2 mg/kg per day and increased at weekly intervals until the symptoms are adequately controlled. The dose of dapsone should not exceed 3~4 mg/kg per day1. Our patient started with 2 mg/kg of dapsone per day and we gradually decreased the dose over three weeks. All the lesions resolved after treatment for three weeks. However, during 10 months of follow-up, the lesion recurred three times despite administration of oral medication.
We considered how the IgA aAbs to LAD-1 affect the prognosis of the patient because the skin lesions of this patient frequently recurred. One prior study reported that drug related LABD reactive to LAD-1 had a good prognosis after discontinuation of the offending drug and treatment with topical antiseptics15. However, the association of CBDC antigens and the correlation with the patient prognosis is not clear. Another study analyzed the aAbs in 50 patients with LABD and no correlation was seen between the presence of IgA aAbs to the NC16a domain and any major clinical features11. Further information on CBDC is needed to improve our understanding of the association between the prognosis and the identified aAbs.
We have reported here on a rare case of obstinate CBDC that was reactive to LAD-1, and this was confirmed by immunoblotting and ELISA.
Figures and Tables
Fig. 1
(A) Clustering of tense bullae and erythematous scaly patches on the right inner thigh. (B) Grouped blisters on the umbilicus with erythematous erosive patches.

Fig. 2
Histology of the vesicles shows subepidermal blisters with a mild inflammatory cellular infiltration in the bulla and upper dermis (H&E, ×100).
References
2. Jabłońska S, Chorzelski TP, Rosinska D, Maciejowska E. Linear IgA bullous dermatosis of childhood (chronic bullous dermatosis of childhood). Clin Dermatol. 1991. 9:393–401.

3. Chorzelski TP, Jablonska S. IgA linear dermatosis of childhood (chronic bullous disease of childhood). Br J Dermatol. 1979. 101:535–542.

4. Hwang YJ, Yang HY, Lee CW, Kim JH. A case of linear IgA bullous dermatosis. Ann Dermatol. 1993. 5:51–55.

5. Park KB, Cho KH, Lee YS. A case of linear IgA bullous dermatosis. Korean J Dermatol. 1986. 24:707–711.
6. Kim HJ, Kim YK, Pyo HC, Lee CW. Linear IgA bullous dermatosis. Korean J Dermatol. 1987. 25:525–530.
7. Park SL, Ihm CW. A case of fulminant linear IgA bullous dermatosis in an adult. Korean J Dermatol. 1995. 33:748–754.
8. Lear JT, Smith AG. Multiple blisters in a young boy. Linear IgA disease of childhood (LADC). (Chronic bullous dermatosis
of childhood). Arch Dermatol. 1998. 134:625. 628.
9. Chin HW, Jang HS, Jo JH, Kim MB, Oh CK, Kwon KS. A case of linear IgA bullous dermatosis probably caused by vancomycin. Korean J Dermatol. 2005. 43:416–418.
10. Zillikens D, Giudice GJ. BP180/type XVII collagen: its role in acquired and inherited disorders or the dermal-epidermal junction. Arch Dermatol Res. 1999. 291:187–194.

11. Zillikens D, Herzele K, Georgi M, Schmidt E, Chimanovitch I, Schumann H, et al. Autoantibodies in a subgroup of patients with linear IgA disease react with the NC16A domain of BP1801. J Invest Dermatol. 1999. 113:947–953.

12. Ishii N, Ohyama B, Yamaguchi Z, Hashimoto T. IgA autoantibodies against the NC16a domain of BP180 but not 120-kDa LAD-1 detected in a patient with linear IgA disease. Br J Dermatol. 2008. 158:1151–1153.

13. Schumann H, Baetge J, Tasanen K, Wojnarowska F, Schäcke H, Zillikens D, et al. The shed ectodomain of collagen XVII/BP180 is targeted by autoantibodies in different blistering skin diseases. Am J Pathol. 2000. 156:685–695.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download