Abstract
Background
Topical photodynamic therapy (PDT) with 5-aminolevulinic acid (ALA) was originally used for treating superficial skin tumors. The application of PDT to other inflammatory dermatoses like acne vulgaris, psoriasis, granuloma annulare, localized scleroderma and lichen sclerosus has recently been introduced. However, the underlying mechanisms are not well understood. We've previously reported the induction of tumor growth factor (TGF)-β1 and interleukin (IL)-10 after PDT with ALA and intense pulsed light (IPL) in cultured HaCaT cells.
Objective
The purpose of this study was to investigate the expressions of TGF-β1 and IL-10 in cultured fibroblasts after PDT with using ALA and IPL.
Methods
Cultured fibroblasts were treated with ALA-IPL PDT (1µmol/L of ALA; 0, 4, 8 and 12 J/cm2 of IPL). The expressions of TGF-β1 and IL-10 were investigated by reverse transcription-polymerase chain reaction and enzyme linked immunosorbent assay.
Photodynamic therapy (PDT) with 5-aminolevulinic acid (ALA) is a currently used therapeutic approach for the treatment of superficial skin tumors and it is under investigation in clinical studies for the treatment of inflammatory dermatoses like acne vulgaris, psoriasis, granuloma annulare, localized scleroderma and lichen sclerosus1. Various light sources are available for PDT, including blue lights, red lights, incoherent lamps and light emitting diodes. The recent studies using intense pulsed light (IPL) as a light source have shown therapeutic effects for photoaging and acne vulgaris2.
Depending on the light dose and the concentration of the photosensitizer used for PDT, either cytotoxic effects resulting tumor destruction or immunomodulatory effects that improve inflammatory conditions will occur. With low density PDT, cell viability may be maintained while other traits such as the signaling activity and the cytokine expression may be altered3. We've previously reported the induction of interleukin (IL)-10 and tumor growth factor (TGF)-β1 in cultured keratinocytes (HaCaT cells) after performing PDT with 5-ALA and IPL at sublethal doses4. Thus, we assumed that the induction of IL-10 may contribute to the anti-inflammatory effect, which explains the therapeutic benefit of PDT for inflammatory dermatoses, and the induction of TGF-β1 may be related to the improvement of psoriasis after PDT4.
The purpose of this study was to examine the expressions of TGF-β1 and IL-10 in cultured fibroblasts after performing PDT with ALA-IPL at sublethal doses.
Normal human fibroblasts from neonatal foreskin were seeded at 3×105 cells/dish in a 35×10 mm dish (Falcon, USA) and they were cultivated in Dulbecco's modified Eagle's medium supplemented with 10% fetal bovine serum, 50µl/ml penicillin and 50µg/ml streptomycin (GIBCO BRL, Gaithersburg, MD, USA) to subconflence. The cells were cultured in a 5% CO2 incubator at 37℃. The cells at passage 2~10 were used for all the experiments. A dose-response curve of PDT for fibroblasts was evaluated to determine the appropriate sublethal doses of ALA and IPL. After application of the medium containing ALA at 0.01, 0.1, 1, 10, 100, 1,000 or 10,000 µmol/L and IPL at 0, 4, 8, 12 or 16 J/cm2, the cell viability was measured and the conditions resulting in <10% cell death were determined. At 1 µmol/L of ALA, less than 10% cell death occurred at up to 16 J/cm2 of IPL.
When the fibroblasts had grown to subconfluence, the cells were incubated with serum-free medium containing ALA (1µmol/L) for 6 hours. Before and after the incubation with ALA, the cells were rinsed twice with phosphate buffered saline (PBS). After removing the PBS, irradiation of the ALA-treated cell culture was performed with a Vascular Applicator Type (VL-2; emission wavelength λem 555~950 nm) of I2PL (Ellipse FLEX®) at 0, 4, 8 or 12 J/cm2 (pulse time: 14 ms, 1 pulse). Culture medium was added after the irradiation and the cells and the culture medium were harvested at 48 hours after the irradiation. All the processes were performed in a dark room under a Wood's light.
The culture medium that was harvested at 48 hours following irradiation was evaluated. The TGF-β1 and IL-10 ELISA kits and the monoclonal antibodies against these molecules were obtained from R&D systems (USA). Each enzyme-linked immunosorbent assay (ELISA) was performed in triplicate.
The total RNA was isolated from cells using an easy-BLUE™ total RNA extraction kit (iNtRON, Korea). The total RNA was stored at -80℃ until use for reverse transcription-polymerase chain reaction (RT-PCR) analysis. RT-PCR was performed with the TGF-β1 primers 5'-CCA GATC CTG TCC AAG CTG-3' (sense) and 5'-CCC TCA ATT TCC CCT CCA-3' (antisense), yielding a PCR product of 495 bp, or with the GAPDH primers 5'-TGA TGA CAT CAA GAA GGT GGT GAA G-3' (sense) and 5'-TCC TTG GAG GCC ATG TGG GCC AT-3' (antisense), yielding a PCR product of 240 bp. The Reverse Transcription System (Promega, USA) and the GoTaq® polymerase system (Promega) were used for reverse transcription and amplification, respectively. The completed samples were run on ethidium bromide/1.5% agarose gel. Bands were identified and quantified photofluorometrically by Quantity One® (Bio-Rad Laboratory, 2000, USA) and they were normalized to GAPDH in order to correct for loading errors.
The measured values were converted into fold changes as compared with the untreated control group, which was treated with serum-free medium without ALA for 6 hours and received no light irradiation. Independent experiments were performed at least in duplicate. The data values are expressed as means±standard error of the mean from triplicate determinations of at least two independent experiments for each case. Statistical significance was evaluated by paired analyses using Student's paired t-test. SPSS for windows (version 12.0; SPSS Inc., Chicago, IL, USA) was used for all the analyses and p values <0.05 were deemed statistically significant.
PDT with 5-ALA was originally used for treating superficial nonmelanoma skin cancers and their precursors. The application of PDT to other inflammatory dermatoses like acne vulgaris, psoriasis, granuloma annulare, localized scleroderma and lichen sclerosus has recently been introduced1. However, the underlying mechanisms of PDT are not well understood.
TGF-β1 is known to be a potent stimulus for fibrosis, and it stimulates fibroblast proliferation and increases the production of collagen and other extracellular matrix proteins, while it inhibits the degradation of these matrix proteins by reducing metalloproteinase (MMP) synthesis. Localized scleroderma is an inflammatory disorder that manifests itself as excessive sclerosis of the skin. It is generally accepted that dermal fibroblasts are the key in the pathogenesis of skin sclerosis by synthesizing increased amounts of collagen type I and III and lesser amounts of collagen degrading enzymes such as MMP-1, MMP-2 and MMP-35. Patients with localized scleroderma and who receive topical PDT with ALA showed a reduction in skin tightness, suggesting this therapy reduces skin sclerosis6. In addition, the levels of MMP-1 and MMP-3 protein and mRNA were increased and the mRNA levels of type I collagen were decreased when normal or scleroderma fibroblasts were treated with ALA-PDT in an in vitro study; this was interpreted as being due to the antisclerotic effects of ALA-PDT5. In this study, we present experimental evidence that ALA-IPL reduced the TGF-β1 expression in human dermal fibroblasts, and this was assumed to be related to the increase of MMPs and the decrease of type I collagen level, as was previously reported5. Further, we also think that the therapeutic effect of PDT on scleroderma would be better after ALA-IPL than that after IPL treatment only because the reduction of TGF-β1 was more prominent after ALA-IPL treatment (the data for the IPL treatment only is not shown).
However, there have been conflicting findings on the effect of ALA-PDT on the expression of MMPs and collagen fibers when PDT was used for photorejuvenation of photoaged skin. Marmur et al.7 showed, by conducting an ultrastructural analysis, that ALA-IPL induced an increase of type I collagen fibers in photodamaged skin. Additionally, the expressions of MMP-1, -3 and -12 were decreased and the immunoreactivity for TGF-β as well as for the TGF-β type II receptor in the epidermis was significantly increased after ALA-PDT8.
We think that the expression of TGF-β may differ between keratinocytes and fibroblasts because we also found the increase of TGF-β1 after PDT in the cultured HaCaT cells in a previous report4. In addition, more complicated mechanisms besides the influence of TGF-β1 would be implicated in the control of the expressions of MMPs and collagen fibers. Karrer et al.9 demonstrated the in vitro paracrine activation of MMP-1 and MMP-3 production in dermal fibroblasts was mediated by soluble factors, particularly IL-1α and TNF-α, which were released by the PDT-treated epidermal keratinocytes. Furthermore, different treatment parameters such as the incubation time of ALA, the laser and light source used and the fluence employed may alter the biochemical and immunological responses.
IL-10 is an anti-inflammatory cytokine that inhibits cytokine production in activated T cells and antigen-presenting cells. Gollnick et al.10 reported that the IL-10 expression was markedly induced in the skin of mice exposed to PDT with using porfirmer and a 630 nm argon dye laser at doses that strongly inhibited contact hypersensitivity, suggesting that the enhanced IL-10 expression plays a role in the suppression of cell-mediated responses after PDT. So, we think that the induction of IL-10 may also play a part in the therapeutic effect of PDT for inflammatory dermatoses, and we previously reported the induction of IL-10 after PDT in culture HaCaT cells4, even though the induction of IL-10 was not superior to that after IPL treatment only. In this study, we observed the induction of IL-10 after PDT in the cultured fibroblast, which indicates that IL-10 may contribute to the anti-inflammatory effect of PDT, at least in part.
To summarize, TGF-β1 mRNA and protein were reduced down to 0.52- and 0.63-fold, respectively, after PDT. The reduction of TGF-β1 may be related to the anti-sclerotic effect of PDT observed in vivo6. This reduction was more prominent after PDT as compared to that after IPL treatment, and so a better antisclerotic effect can be expected with PDT than with IPL treatment. IL-10 protein was increased up to 2.74-fold after PDT. The induction of IL-10 may contribute to the anti-inflammatory effect, which explains the therapeutic benefit of PDT for inflammatory dermatoses. Despite the fact that this is an in vitro study with limited variables and the IL-10 induction after PDT was statistically insignificant, we believe that these findings may contribute to a better understanding of the immunologic effects of PDT.
Figures and Tables
Fig. 1
The expressions of tumor growth factor (TGF)-β1 and interleukin (IL)-10 protein after aminolevulinic acid (ALA)-intense pulsed light (IPL) measured by enzyme-linked immunosorbent assay. The data represents the mean±SEM from triplicate determinations of at least two independent experiments for each case. *A significant difference compared with the control that was treated with neither ALA nor IPL (p<0.05).

Fig. 2
Reverse transcription-polymerase chain reaction analysis of the mRNA expression of tumor growth factor (TGF)-β1 after aminolevulinic acid (ALA)-intense pulsed light (IPL).

Table 1
TGF-β1 and IL-10 expression (x-fold induction) after ALA-IPL
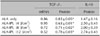
Data represent mean±SEM from triplicate determinations of at least two independent experiments for each case. *A significant difference compared with control that was treated with neither ALA nor IPL (p<0.05). TGF: tumor growth factor, IL: interleukin, ALA: aminolevulinic acid, IPL: intense pulsed light.
References
1. Babilas P, Karrer S, Sidoroff A, Landthaler M, Szeimies RM. Photodynamic therapy in dermatology--an update. Photodermatol Photoimmunol Photomed. 2005. 21:142–149.
2. Gold MH. Acne and PDT: new techniques with lasers and light sources. Lasers Med Sci. 2007. 22:67–72.

3. Hunt DW, Levy JG. Immunomodulatory aspects of photodynamic therapy. Expert Opin Investig Drugs. 1998. 7:57–64.

4. Byun JY, Choi HY, Myung KB, Choi YW. Expression of IL-10, TGF-β1 and TNF-α in cultured keratinocytes (HaCaT cells) after IPL treatment or ALA-IPL photodynamic treatment. Ann Dermatol. 2009. 21:12–17.

5. Karrer S, Bosserhoff AK, Weiderer P, Landthaler M, Szeimies RM. Influence of 5-aminolevulinic acid and red light on collagen metabolism of human dermal fibroblasts. J Invest Dermatol. 2003. 120:325–331.

6. Karrer S, Abels C, Landthaler M, Szeimies RM. Topical photodynamic therapy for localized scleroderma. Acta Derm Venereol. 2000. 80:26–27.

7. Marmur ES, Phelps R, Goldberg DJ. Ultrastructural changes seen after ALA-IPL photorejuvenation: a pilot study. J Cosmet Laser Ther. 2005. 7:21–24.

8. Park MY, Sohn S, Lee ES, Kim YC. Photorejuvenation induced by 5-aminolevulinic acid photodynamic therapy in patients with actinic keratosis: a histologic analysis. J Am Acad Dermatol. 2010. 62:85–95.

9. Karrer S, Bosserhoff AK, Weiderer P, Landthaler M, Szeimies RM. Keratinocyte-derived cytokines after photodynamic therapy and their paracrine induction of matrix metalloproteinases in fibroblasts. Br J Dermatol. 2004. 151:776–783.

10. Gollnick SO, Liu X, Owczarczak B, Musser DA, Henderson BW. Altered expression of interleukin 6 and interleukin 10 as a result of photodynamic therapy in vivo. Cancer Res. 1997. 57:3904–3909.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download