Dear Editor:
Warts are also known as verrucae, and these are benign proliferative lesions of the epidermis that are caused by human papilloma virus (HPV) infections1. There are many treatment modalities for warts, which implies that no single modality is uniformly effective. The choice of treatment depends on the location, size, number and type of wart, as well as on the patient's age and cooperation. Irrespective of the treatment modality, a host immune response is the key to achieving complete clearance. As such, immune-compromised individuals may never achieve wart clearance2. In other words, wart eradication can be achieved if the HPV-specific immunity can be stimulated. We report here on a case of a rapidly regressed wart following biopsy without any additional treatment.
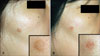
A 50-year-old woman presented to our clinic with a complaint of a papule located on her right cheek. The lesion was flesh to light brown in color and about 1 cm in diameter. It appeared more than 6 months prior to her presentation as a small pimple-like lesion, which had been slowly growing (Fig. 1A) without any associated pain or itching sensation. Its clinical appearance resembled seborrheic keratosis or other benign papules. A 2 mm-punch biopsy was taken at the center of the lesion without suturing. The histopathological findings were hyperkeratosis and papillomatosis, with elongated rete ridges and koilocytes. Immunohistochemical staining for CD3, CD4, CD8, CD20, CD56 and cytotoxic T cell intracellular antigen-1 (TIA-1) was performed. The dermal lymphocytes were predominantly CD3 and CD4-positive T-cells. The intraepidermal exocytotic cells were mildly positive for CD8 and TIA-1. The staining for CD20 and CD56 was negative. A diagnosis of wart was made. The lesion rapidly regressed within one week of the biopsy (Fig. 1B) and it had completely disappeared when the patient presented for follow-up after one month.
The role of immunity in HPV infection is not completely understood3,4. The decreasing trend of the prevalence of wart with age suggests that resistance to HPV infection develops over time, and much of this phenomenon may be immunological2. Individuals with impaired cell-mediated immunity are particularly susceptible to HPV infections, and these individuals' warts are recalcitrant to treatment5.
There are instances in which treatment of one or more warts leads to complete clearance in immune-competent individuals. Children with warts may not require treatment since spontaneous regression is common as their immunity develop1. One report has suggested that specific cell-mediated immunity against viral infected keratinocytes took place in the process of spontaneous plane wart regression6. Another study demonstrated CD4-positive lymphocytes predominated in regressing genital wart7. Our case could also be interpreted in a similar context. Tissue biopsy might have exposed viral antigens to the host immune system, which subsequently triggered HPV-specific immunity. The immunohistochemical staining for TIA-1 was positive in the epidermis, which also means there was an activated cytotoxic T-cell infiltration.
It is also possible that this patient had already developed HPV-specific cell-mediated immunity prior to the biopsy, and without the intervention the verruca could have remained as a solitary papule. The biopsy may have then exposed viral antigens and induced a delayed hypersensitivity reaction, which led to rapid regression of the lesion. A cutaneous wart management guideline has proposed curettage and light cautery for facial warts2. This was the similar course of action we took for our patient.
There have been many cases of warts with spontaneous regression, but there has been no report of wart regression following a small biopsy. In conclusion, wart regression requires an immune reaction to viral antigens. Therefore, inducing and mounting such a response are critical for the management of warts.
Figures and Tables
References
1. Elliot J, Androphy DRL. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Warts. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1914–1922.
2. Sterling JC, Handfield-Jones S, Hudson PM. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001. 144:4–11.

3. Malejczyk J, Majewski S, Jablońska S. Cellular immunity in cutaneous and genital HPV infections. Clin Dermatol. 1997. 15:261–274.

5. Berkhout RJ, Bouwes Bavinck JN, ter Schegget J. Persistence of human papillomavirus DNA in benign and (pre)malignant skin lesions from renal transplant recipients. J Clin Microbiol. 2000. 38:2087–2096.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download