Abstract
A 6-day-old infant presented with a deeply bluish cystic mass below the right medial canthus. She had been born healthy. Under the impression of a hemangioma brain computed tomography was conducted. As a result, a diagnosis of congenital dacryocystocele was made. We present this case to show that it is important for a dermatologist to correctly identify congenital dacryocystoceles and appropriately refer the infant to a pediatric ophthalmologist prior to performing invasive measures.
A bluish, cystic and firm mass below the medial canthus presenting shortly after birth is the classic presentation for a dacryocystocele1. Infants showing such skin lesions without any other systemic symptoms present to a dermatologist first, so an awareness of this condition and its potential complications is important.
We present a case of congenital dacryocystocele presented as a bluish cystic mass on the face.
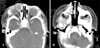
A 6-day-old infant presented with a 0.5×0.5 cm-sized ill-demarcated bluish cystic mass below the medial canthal area (Fig. 1). She had been born healthy, and any other systemic diseases had not been presented yet. She had no systemic symptoms such as irritability, poor oral intake or respiratory grunting. Under the impression of a hemangioma brain computed tomography was conducted. On the right medial canthal area, a well-defined cystic mass extending to the nasal cavity along by lacrimal duct was found (Fig. 2). As a result, a diagnosis of congenital dacryocystocele was made. She was referred to an ophthalmologist and was prescribed antibiotic drops. Gentle lacrimal sac massage was performed and two weeks later the size of the mass has been markedly shrunk (Fig. 3). She has not had any associated complications so far. Now she is being followed up every other week to prevent any complications from arising.
Congenital dacryocystocele is a relatively common disease among neonates and infants. The frequency is reported from 1.25% to 12.5% according to authors2. In Korea the frequency has been reported 6.25%3. Congenital dacryocystoceles typically present in the first week or month of life and result from the blockage at the distal end of the nasolacrimal system at the valve of Hasner and the functional proximal obstruction at the junction of the common canaliculus and the sac4. The result is distension of the lacrimal sac below the medial canthal tendon, which may appear as a mass. It is likely that a combination of dissolved mesoderm, mucus, amniotic fluid, tears, and bacterial colonization cause the distension of the lacrimal system seen in dacryocystoceles5.
It is important to differentiate dacryocystoceles from other conditions. Encephaloceles, nasal gliomas, hemangiomas, dermoids, sebaceous cysts, and mucoceles can also present similarly lesions and must be considered in the differential diagnosis5. Inspection and palpation is important for the differential diagnosis. Dermatological diseases such as hemangiomas, dermoids, and sebaceous cysts are more superficial and less firm on palpation6. If clinical manifestations like difficulty with breathing or difficulty with breast feeding are present, congenital nasolacrimal obstructions should be considered. Radiological examination such as brain computed tomography and magnetic resonance imaging could be conducted to rule out neurological problems. A bluish cystic mass without any associated symptoms is usually difficult to differentiate from hemangiomas. Hemangiomas leave the lacrimal passage patent6; therefore, sonography or lacrimal duct examination should be undertaken. Dacryocystoceles can be easily diagnosed by sonography, and be confirmed by probing the lacrimal duct4. The ultrasound is a simple and non-invasive method that can reliably distinguish dacryocystoceles from other pathological conditions7.
The management of a congenital dacryocystocele is conservative, and it includes gentle massage on the lacrimal sac, which can facilitate decompression and drainage of the contents into the nose6. Antibiotic drops may also be used prophylactically before infection occurs6. The resolution rate after a short course of topical antibiotics, warm compresses and massage has been reported to be 76%5. Probing can be performed when resolution is lacking. Probing and irrigation of nasolacrimal system has been shown to effectively ameliorate the obstruction5. Significant controversy exists as to the preferred management and timing of intervention for infants with congenital dacryocystoceles. After confirming the diagnosis by lacrimal excretion test and radiological examination, the outcome of appropriate surgical treatment should be successful4.
As possible complications, dacryocystitis can develop within a few days or weeks and requires intravenous antibiotics to prevent life-threatening sepsis5. Another serious complication is respiratory compromise, which occurs when there is a large intranasal cystic mass causing blockage of the nasal cavity5. There are several important structures around or in the medial canthus such as lacrimal canaliculi and lacrimal sac. Therefore, performing a skin biopsy of the mass inferior to medical canthal area is very risky before dacryocystoceles ruled out.
We present this case to show that it is important for a dermatologist to correctly identify congenital dacryocystoceles and appropriately refer the infant to a pediatric ophthalmologist before performing invasive measures and life-threatening complications such as sepsis or respiratory compromise arising. The cooperation with an otorhinolaryngologist and an ophthalmologist could lead to the proper diagnosis of dacryocystoceles and sufficient treatment without serious complications.
Figures and Tables
References
2. Noda S, Hayasaka S, Setogawa T. Congenital nasolacrimal duct obstruction in Japanese infants: its incidence and treatment with massage. J Pediatr Ophthalmol Strabismus. 1991. 28:20–22.
3. Lee SY, Chung HS, Kim HB, Namgung R, Han DG. The incidence of congenital nasolacrimal duct obstruction in Korean neonates. J Korean Ophthalmol Soc. 1989. 30:5–8.
5. Wong RK, VanderVeen DK. Presentation and management of congenital dacryocystocele. Pediatrics. 2008. 122:e1108–e1112.

6. Robb RM. Albert DM, Miller JW, Azar DT, editors. Lacrimal system abnormalities. Albert & Jakobiec's principles & practice of ophthalmology. 2008. 3rd ed. Philadelphia: Elsevier Saunders;4195–4199.

7. Cavazza S, Laffi GL, Lodi L, Tassinari G, Dall'Olio D. Congenital dacryocystocele: diagnosis and treatment. Acta Otorhinolaryngol Ital. 2008. 28:298–301.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download