Abstract
Elastosis perforans serpiginosa (EPS) is a rare reactive perforating dermatosis that is characterized by the transepidermal elimination of abnormal elastic fibers. Penicillamine, which is one of the clear triggers for EPS, is a heavy metal chelator that is primarily used for disorders such as cystinuria and Wilson's disease. It may cause alterations in the dermal elastic tissue such as pseudo-pseudoxanthoma elasticum, acquired cutis laxa, EPS and anetoderma. Herein we present a case of cutis laxa and EPS in a 34-year-old man who was previously on a long-term, high-dose of penicillamine for Wilson's disease. The combination of EPS and cutis laxa induced by penicillamine has rarely been reported and we report the first such case in Korea.
Elastosis perforans serpiginosa (EPS) is a rare reactive perforating dermatosis that is characterized by the transepidermal elimination of abnormal elastic fibers1. Although D-penicillamine appears to be a clear trigger for EPS2, penicillamine-induced EPS has been rarely reported. Penicillamine is a copper chelator that is used at high dosages for patients with Wilson's disease, and the cutaneous reactions to this drug can be classified into three groups: hypersensitivity reactions, autoimmune conditions and a spectrum of cutaneous elastotic and collagen disorders3. The third group includes pseudoxanthoma elasticum (PXE),EPS, cutis laxa and anectoderma4,5. They may be caused by penicillamine affecting the function of copper-dependent lysyl oxidase, which is an enzyme involved in crosslinking between elastin molecules6.
Herein we report a case illustrating the clinical and histological findings of EPS and cutis laxa in a patient who was on a long-term high-dose penicillamine for Wilson's disease. The combination of EPS and cutis laxa induced by penicillamine has rarely been reported7 and we report the first such case in Korea.
A 34-year-old man, who had been treated with D-penicillamine for 20 years for Wilson's disease, visited the clinic for progressive cutaneous lesions of the neck that he'd had for the past 1 year. He had been taking penicillamine at a dose of 500~1,250 mg daily for 20 years since 14 years of age. He had not shown any cutaneous side effects during the early period of penicillamine intake. However, 2 years previously, the skin folds over both elbows and knees started to become markedly loose (Fig. 1). But, the lesions had not been evaluated or treated at that time.
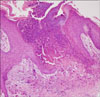
In 2009, he came to see us with new lesions on the neck that had been present for the previous 1 year. Clinical examination revealed multiple match head-sized keratotic papules on an annular erythematous base on the nape and lateral neck (Fig. 2). A 3-mm punch biopsy specimen from a papule on the neck demonstrated a perforating channel from the dermis through the epidermis with a surrounding inflammatory infiltrate and multinucleate giant cells (Fig. 3). Verhoeff-van Gieson staining of the specimen revealed abnormal elastic fibers in the upper dermis and transepidermal elimination of those abnormal elastic fibers (Fig. 4A). And the 'bramble-bush' appearance that means thickened elastic bundles with prominent lateral protrusions is well shown (Fig. 4B).
According to the clinical and histological findings of the patient, we diagnosed him as having cutis laxa and elastosis perforans induced by penicillamine. After a consultation with the patient's neurologist, the penicillamine was discontinued and trientine dihydrochloride, an alternative copper chelator, was commenced. We first used a CO2 laser to resurface the lesions. Thereafter, we advised him to use topical tretinoin 0.025% cream and the lesions showed partial regression.
Penicillamine is an efficient copper chelator that is used for the treatment of Wilson's disease, cystinuria, rheumatoid arthritis, scleroderma and primitive biliary cirrhosis8. Most of the adverse effects of D-penicillamine are cutaneous and they occurring in 25~50% of patients. These adverse effects can be classified into three groups3, including early onset morbilliform and urticarial hypersensitivity reactions and later onset bullous and lupus-like autoimmune reactions9. The third group of dermopathies is a spectrum of cutaneous elastotic and collagen disorders3 such as PXE, EPS, cutis laxa and anectoderma4,5.
The underlying mechanism for how penicillamine disrupts elastin production or remodeling remains uncertain. One proposed mechanism involves the copper-dependent enzyme lysyl oxidase. This enzyme is required for the cross-linkage of elastic and collagen fibers in the dermis. The indirect inhibition of the enzyme activity by removal of copper from the tissues by penicillamine causes abnormal elastic fiber accumulation9. An alternate or complementary mechanism is direct drug inhibition of the deamination of the lysine residues that are necessary for elastin and collagen maturation10.
The clinical features seen in penicillamine-induced EPS and cutis laxa are similar to those seen in the idiopathic heritable forms of the diseases8. As illustrated in this case, EPS is characterized by the development of annular or serpiginous hyperkeratotic papules, and most frequently on the lateral neck and upper limbs.
The characteristics and specific histological changes of penicillamine-induced elastic fiber damage are thickened elastic bundles with prominent lateral protrusions giving the so-called 'bramble-bush' appearance11. In contrast to the calcification of the shortened, curled basophilic elastic fibers in the inherited forms of PXE, calcification of elastic fibers in penicillamine-induced elastosis is considered to be unusual12. As was present in this case, a variable degree of granulomatous inflammation is often observed in the dermis11,12. Transepidermal elimination of abnormally large and tortuous eosinophilic 'bramble-bush' elastic fibers is an additional feature of penicillamine-induced EPS13.
Many treatment modalities have been described in the medical texts because of the difficulty to manage this condition and there is no "gold standard" therapy. The moderately effective treatments include cryotherapy, cellophane tape stripping and oral isotretinoin. There have been some recent reports of successful outcomes after using tazarotene gel14 and imiquimod cream15. We have used various methods, including a CO2 laser to resurface the lesions and a tretinoin cream, but those induced only a partial resolution of the lesions.
Furthermore, discontinuation of penicillamine therapy does not guarantee the prevention of further development of the dermatosis. Multiple case reports have described the abrupt onset or recurrence of EPS months to years after stopping penicillamine therapy9,14,16. This is likely related to the cumulative dose and the slow clearance of the drug with the remaining effects on the elastic tissue9.
In summary, we report here on a case that illustrates the clinical and histological characteristics of EPS and cutis laxa in a patient who was on long-term high-dose penicillamine for Wilson's disease. We hope that this case will help physicians become aware of the adverse dermatologic effects of long-term penicillamine therapy.
Figures and Tables
References
1. O'Donnell B, Kelly P, Dervan P, Powell FC. Generalized elastosis perforans serpiginosa in Down's syndrome. Clin Exp Dermatol. 1992. 17:31–33.

2. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;566–567.

3. Breathnach SM. Champion RH, Burton JL, Burns AD, Breathnach SM, editors. Drug reactions. Rook/Wilkinson/Ebling textbook of dermatology. 1998. 6th ed. Oxford: Blackwell Science;3450–3452.

4. Pass F, Goldfischer S, Sternlieb I, Scheinberg IH. Elastosis perforans serpiginosa during penicillamine therapy for Wilson disease. Arch Dermatol. 1973. 108:713–715.

6. Mehta RK, Burrows NP, Payne CM, Mendelsohn SS, Pope FM, Rytina E. Elastosis perforans serpiginosa and associated disorders. Clin Exp Dermatol. 2001. 26:521–524.

7. Amichai B, Rotem A, Metzker A. D-penicillamine-induced elastosis perforans serpiginosa and localized cutis laxa in a patient with Wilson's disease. Isr J Med Sci. 1994. 30:667–669.

8. Poon E, Mason GH, Oh C. Clinical and histological spectrum of elastotic changes induced by penicillamine. Australas J Dermatol. 2002. 43:147–150.

9. Lewis BK, Chern PL, Stone MS. Penicillamine-induced elastosis of the mucosal lip. J Am Acad Dermatol. 2009. 60:700–703.

10. Price RG, Prentice RS. Penicillamine-induced elastosis perforans serpiginosa. Tip of the iceberg? Am J Dermatopathol. 1986. 8:314–320.

11. Bardach H, Gebhart W, Niebauer G. "Lumpy-bumpy" elastic fibers in the skin and lungs of a patient with a penicillamine-induced elastosis perforans serpiginosa. J Cutan Pathol. 1979. 6:243–252.

12. Sahn EE, Maize JC, Garen PD, Mullins SC, Silver RM. D-penicillamine-induced elastosis perforans serpiginosa in a child with juvenile rheumatoid arthritis. Report of a case and review of the literature. J Am Acad Dermatol. 1989. 20:979–988.

13. Mehregan AH. Elastosis perforans serpiginosa: a review of the literature and report of 11 cases. Arch Dermatol. 1968. 97:381–393.

14. Outland JD, Brown TS, Callen JP. Tazarotene is an effective therapy for elastosis perforans serpiginosa. Arch Dermatol. 2002. 138:169–171.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download