INTRODUCTION
Lichen nitidus (LN) is an unusual chronic inflammatory disease that commonly begins in childhood and early adulthood1. The cause has not been revealed. It is generally asymptomatic and LN is characterized by tiny, discrete, flesh-colored, shiny, flat-topped or dome-shaped papules. The sites of predilection are the genitalia, trunk and extremities2, although the eruption can be generalized3. LN occurring on the palms, soles, nails and mucous membranes has been infrequently reported4-8.
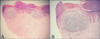
Diseases that can be considered in the differential diagnosis of LN include keratosis pilaris, lichen planus, follicular eczema and verruca plana, and histopathological evaluation is helpful to confirm the diagnosis. The histopathologic findings in LN are very characteristic. Each papule of LN consists of a circumscribed collection of lymphocytes and epitheloid histiocytes in a widened dermal papilla that is closely attached to the lower surface of the epidermis. Surrounding this infiltrate is epidermal hyperplasia with elongation of the rete ridges. These findings are classically referred to as a 'claw clutching a ball pattern'. Other reported findings are flattening of the epidermis overlying the infiltrate with focal parakeratosis8.
We report here on a rare case of palmar LN that showed clinical features similar to pompholyx, and we review the relevant medical literature.
CASE REPORT
A 53-year-old Korean man presented with multiple pruritic eruptions on his right palm that he'd had for 2 years. He had no previous skin and medical problems. There was no history of chronic trauma to the right palm. On the examination, the skin lesion consisted of grouped, 2~3 mm sized, erythematous to flesh colored vesicles and papules (Fig. 1). The skin lesion was clinically similar to pompholyx or chronic eczema. A skin punch biopsy was performed. The histopathological examination revealed hyperkeratosis and parakeratosis in the epidermis and well circumscribed, dense inflammatory cellular infiltrates in the papillary dermis. Acanthotic rete ridges surrounded the papillary dermal infiltrate. The characteristic 'claw clutching a ball pattern' was seen, which was consistent with LN (Fig. 2). The patient was treated with oral azelastine and topical diflucortolone valerate for 3 weeks with improvement of the pruritus. But the skin lesion did not respond to the treatment and they have remained for 18 months, until now.
DISCUSSION
There have been a few reported cases of LN involving the palm, yet most of the previous cases were associated with lesions of the more typical sites, including the trunk and extremities4. Palmar involvements of LN tend to be accompanied with plantar lesions. The lesions of LN confined to the palm are rare and, to the best of our knowledge, there are only 2 such reported cases in the English literature4,6 and a case in the Korean literature9 (Table 1). Two of the 3 reported cases were localized to the unilateral side, like in our case. Palmar LN can cause diagnostic confusion because it differs from classical LN not only in its localization, but also in the clinical appearance of the lesions10.
LN is more prevalent in children and young adults, but the reported cases of palmar LN presented at a relatively old age and the mean age at onset of the four cases, including this case, was 45 years (age range: 37~52)4,6,9. The 2 of the 3 reported cases showed pompholyx-like skin lesions that were similar to those of this patient. The typical skin lesions of the common LN, which are described as skin colored, flat topped papules, were not prominently shown by this patient. LN is usually asymptomatic, but it can be pruritic. This patient complained of moderate pruritus on the palmar lesion. Of the 3 reported cases of palmar LN, pruritus was present in one case.
LN is self-limiting and it eventually resolves spontaneously after months to 1 year in most of the patients3. It has been reported that topical steroid, topical tacrolimus, oral astemizole or phototherapy can be effective in LN11. However, palmar LN has shown chronic courses and it can be refractory to treatments. The mean duration of the reported three cases was 18.3 years and the duration of this patient was 2 years. For this patient of our report, the skin lesion did not respond to oral antihistamine and topical steroid treatment, yet the pruritus was improved.
We report here on an additional case of palmar LN and we think that more additional case reports will reveal the clinical features and progression of palmar LN. LN confined to the palm is rare and it can present as a clinical feature mimicking pompholyx. Physicians should keep in mind the possibility of palmar LN when a patient presents with palmar skin lesions that mimic pompholyx and these lesions are unilaterally distributed.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download