Abstract
Erosive pustular dermatosis of the scalp (EPDS) is a rare disorder of the elderly characterized by multiple pustular lesions with erosions and crusting that result in scarring alopecia. EPDS typically develops in aged or sun-damaged skin with a history of trauma. Histopathologically, EPDS is nonspecific, showing atrophic epidermis and chronic inflammation. Bacteriological and mycological investigations of EPDS are generally negative. Although herpes zoster is a common disorder in elderly people, previously reported cases of EPDS were rarely associated with herpes zoster. We present a rare case of EPDS following herpes zoster treated successfully with topical tacrolimus.
Erosive pustular dermatosis of the scalp (EPDS) is a rare chronic disorder characterized by erosive, crusting and pustular lesions on the scalp that lead to scarring alopecia1. This disorder mainly occurs in elderly patients with previous trauma to the scalp1,2. Less than 50 cases have been reported since its first description by Pye et al.1 in 1979. To our knowledge, only 3 cases of EPDS were associated with herpes zoster3-5. We report a case of EPDS following herpes zoster successfully treated with topical tacrolimus.
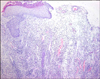
A 71-year-old man presented with a 1-week history of painful erythematous vesicular eruptions on the left occipital scalp. Tzanck smear from the vesicular lesions of the scalp revealed multinucleated giant cells. He was diagnosed with herpes zoster based on clinical findings and Tzanck smear test, and was initially treated with intravenous acyclovir. The lesions resolved completely 3 weeks later. One month later of resolution of the herpes zoster lesion, the patient revisited our clinic with erosions and crusted pustular lesions in an area identical to previous zoster lesions on the left scalp. Small painful pustules had appeared a week prior and continued to expand. The appearance of his scalp lesions suggested bacterial infection. Bacterial culture of the lesions grew mixed skin flora. Tzanck smear was negative. Debridement of the crusts and treatment with systemic and topical antibiotics failed to improve the lesions (Fig. 1A). Skin biopsy was taken with a suspected diagnosis of EPDS. Histopathological examination revealed ulcerated epidermis with parakeratosis and serum-crust, and a mixed dense dermal infiltrate consisting of lymphocytes, neutrophils and plasma cells (Fig. 2). Special staining and cultures for bacteria, fungi and atypical mycobacterium were negative. The final diagnosis of EPDS was therefore made. The patient was treated with topical 0.1% tacrolimus ointment twice daily, which resulted in significant lesion improvement within a week (Fig. 1B). Topical tacrolimus treatment was well tolerated. Two months later, the erosive and pustular lesions almost completely resolved (Fig. 1C). No signs of recurrence were observed during the subsequent 4-month follow-up without treatment.
Our case showed the features of partial scarring alopecia (PCA)6. PCA probably results from irreversible damage to the epithelial hair follicle stem cells in the area of the bulge7. The severity of inflammation in this area may therefore determine the degree of scarring alopecia. The clinical differential diagnosis of EPDS includes bacterial or fungal infection, pemphigus, squamous cell carcinoma and dermatitis artefacta. EPDS is a diagnosis of exclusion based on histopathologic and microbiologic examination. Histopathologically, EPDS is non-specific, showing atrophic epidermis and chronic inflammation consisting of lymphocytes, neutrophils, plasma cells and occasional foreign-body giant cells2. Various microorganisms have been identified in the lesions. However, these organisms represent secondary colonization rather than primary infection5.
Although the pathogenesis is not well known, predisposing factors such as actinic damage and recent or past local trauma have been reported5. Moreover, autoimmune disorders have been described in association with EPDS. Therefore, it has been suggested that physical trauma to the skin might cause auto-antibodies production against skin structures, resulting in a secondary inflammatory reaction8,9. The fact that EPDS responds to topical anti-inflammatory agents supports this hypothesis. In our patient, we consider that the tissue damage caused by herpes zoster might have induced subsequent EPDS. According to previous reports3-5, EPDS following herpes zoster outbreak begins in the same area as the initial injury, and remains unilateral. These published reports, along with our case, provide reliable evidence to support the assertion that herpes zoster can be a causative factor in EPDS.
The most commonly administered treatment for EPDS is potent topical steroids1. However, in view of worsening cutaneous atrophy, topical tacrolimus has been proposed as an alternative therapy10. Tacrolimus is a potent anti-inflammatory and immunosuppressive agent that has demonstrated to be effective in the management of chronic inflammatory dermatoses11. Recently, a few cases of successful treatment of EPDS with topical tacrolimus ointment have been reported10,12. After topical tacrolimus application, our case also showed rapid improvement.
In conclusion, herpes zoster is a common affliction in the elderly. Although EPDS associated with herpes zoster is rare, it is likely that more cases will be recognized if dermatologists are aware of this association.
Figures and Tables
References
1. Pye RJ, Peachey RD, Burton JL. Erosive pustular dermatosis of the scalp. Br J Dermatol. 1979. 100:559–566.

2. Burton JL, Peachey RD, Pye RJ. Erosive pustular dermatosis of the scalp--a definition. Br J Dermatol. 1988. 119:411.

3. Wollenberg A, Heckmann M, Braun-Falco O. Erosive pustular dermatosis of the scalp after zoster ophthalmicus and trauma. Hautarzt. 1992. 43:576–579.
4. Grattan CE. Erosive pustular dermatosis of the scalp following zoster ophthalmicus. J R Coll Gen Pract. 1988. 38:470–471.
5. Grattan CE, Peachey RD, Boon A. Evidence for a role of local trauma in the pathogenesis of erosive pustular dermatosis of the scalp. Clin Exp Dermatol. 1988. 13:7–10.

6. Olsen EA, Bergfeld WF, Cotsarelis G, Price VH, Shapiro J, Sinclair R, et al. Summary of North American Hair Research Society (NAHRS)-sponsored Workshop on Cicatricial Alopecia, Duke University Medical Center, February 10 and 11, 2001. J Am Acad Dermatol. 2003. 48:103–110.

7. Cotsarelis G. Epithelial stem cells: a folliculocentric view. J Invest Dermatol. 2006. 126:1459–1468.
8. Watanabe S, Takizawa K, Hashimoto N, Ishibashi Y. Pustular dermatosis of the scalp associated with autoimmune diseases. J Dermatol. 1989. 16:383–387.

9. Yamamoto T, Furuse Y. Erosive pustular dermatosis of the scalp in association with rheumatoid arthritis. Int J Dermatol. 1995. 34:148.

10. Laffitte E, Kaya G, Piguet V, Saurat JH. Erosive pustular dermatosis of the scalp: treatment with topical tacrolimus. Arch Dermatol. 2003. 139:712–714.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download