Abstract
Hand-foot-mouth (HFM) disease is primarily a disease of children, although it can be seen in immunocompromised adults. We describe a case of HFM disease in a 35-year-old immunocompetent male. He presented with multiple, 1~2 mm sized, erythematous vesicular papules on both hands and feet. Histopathological findings of a skin biopsy showed superficial perivascular lymphocytic infiltration, focal keratinocyte necrosis, and reticular degeneration. Because delayed diagnosis can cause spread of the disease to children, dermatologists should be aware that HFM disease can occur in adults with intact immune systems.
Hand-foot-mouth (HFM) disease is a highly infectious disease characterized by multiple vesicles on the hands and feet and in the oral cavity. It usually occurs in children in the summer. Coxsackievirus A16 is the most common virus causing HFM disease; other causative viruses include coxsackieviruses A5, A7, A9, A10, B2, B5, and enterovirus 711. Clinically, the onset is characterized by fever and the appearance of papules on the hands, feet, and in the oral cavity, which progress to vesicles. Symptoms usually subside within 7 to 10 days2. Although several cases of HFM disease have been reported, it has been rarely reported in immunocompetent adults.
A 35-year-old Korean male presented with multiple peripheral vesicles which had begun to appear on the palms of his hands 3 days previously, and which progressed to the interdigital areas, soles, and dorsum of the feet. He had no past history of medical problems and was not taking medications. His 2-year-old son had been recently diagnosed with HFM disease, presenting with lesions on the palms, soles of the feet, and in the oral cavity, approximately 5 days before the onset of the patient's skin lesions. The patient complained of general weakness and tender, pruritic skin lesions. Physical examination revealed multiple erythematous papules and vesicles on the palms, soles and dorsum of the feet (Fig. 1). The oral cavity and other areas such as face and trunk were spared. Laboratory findings, including complete blood counts and blood chemistries, were within normal limits.
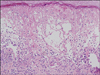
Histologically, a skin biopsy from the foot displayed superficial lymphocytic infiltration on perivascular area and dermo-epidermal junction, focal keratinocyte necrosis, and reticular degeneration of epidermal cells. There were no inclusion bodies or multinucleated giant cells (Fig. 2).
The diagnosis of HFM disease was made based on history as well as typical clinical findings, including distribution of skin lesions. The patient was treated symptomatically with antihistamines, and the lesions resolved spontaneously without complications.
HFM disease is a highly contagious disease mainly caused by enteroviruses. The initial presentation includes erythematous papules on the palms, feet, and in the oral cavity, accompanied by prodromal symptoms such as myalgia, mild fever, and abdominal pain. The lesions usually evolve into vesicles and then spontaneously resolve within 1 or 2 weeks3. Lesions are usually asymptomatic, but in some cases, pressure and touch can provoke pain. Children are the most susceptible, and immunocompromised adults can also be affected. However, HFM disease is especially very rare in immunocompetent adults.
Oral lesions usually appear simultaneously with or precede cutaneous lesions, but the simultaneous occurrence of lesions on the hands, feet, and in the oral cavity in adults is very infrequent4. In addition, oral lesions may occur without cutaneous lesions5, and HFM disease without oral mucosal lesions has also been reported in an immunocompromised adult6. In this report, the diagnosis of HFM disease was done based on the typical cutaneous features, histology, serology, and polymerase chain reaction (PCR) results, despite the lack of definite oral lesions. Therefore, the diagnosis of HFM disease without the appearance of oral lesions might remain doubtful in our case, because PCR testing, which has high sensitivity and specificity for the diagnosis of HFM disease, was not performed. However, considering that the patient's son showed typical clinical manifestations of HFM disease before the onset of cutaneous lesions in the patient, and that the histologic features of the patient's skin biopsy included reticular and ballooning degeneration of the epidermis, we presume that the lesions on his hands and feet are consistent with HFM disease. Oral lesions could have been overlooked or have already disappeared. Although viral culture is considered the best method for accurate diagnosis, the diagnosis is usually made based on clinical presentation7. Characteristic histological findings of the skin lesions include reticular and ballooning degeneration of the epidermis with no inclusion bodies or multinucleated giant cells8.
HFM disease usually occurs in the summer, from June to October, although it has been also reported in the winter9. Coxsackievirus belongs to picornavirus family (small RNA viruses) together with echovirus, enterovirus, and poliovirus. Humans are thought to be the only natural host of coxsackievirus. Because it is highly infectious and transmitted by oral-oral or fecal-oral routes, education regarding hygienic precautions is very important.
Treatment is symptomatic, and the disease resolves spontaneously without complications within 7 to 10 days. However, there have been rare reports of severe complications such as pneumonia, cardiomyositis10, and aseptic meningitis11. Since HFM disease is highly contagious, and elderly people, pregnant women, and immunocompromised adults may develop severe complications, early diagnosis and isolation are necessary. Because HFM disease is especially rare in immunocompetent adults, early detection and accurate diagnosis are very difficult. In conclusion, to prevent the infection from spreading to children and vulnerable adults, dermatologists should be aware that HFM disease can occur in an immunocompetent adult.
Figures and Tables
References
1. Robinson CR, Doane FW, Rhodes AJ. Report of an outbreak of febrile illness with pharyngeal lesions and exanthem: Toronto, summer 1957; isolation of group A Coxsackie virus. Can Med Assoc J. 1958. 79:615–621.
2. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1867–1869.
4. Johnston JM, Burke JP. Nosocomial outbreak of hand-foot-and-mouth disease among operating suite personnel. Infect Control. 1986. 7:172–176.

5. McKinney RV. Hand, foot, and mouth disease: a viral disease of importance to dentists. J Am Dent Assoc. 1975. 91:122–127.

6. Faulkner CF, Godbolt AM, DeAmbrosis B, Triscott J. Hand, foot and mouth disease in an immunocompromised adult treated with aciclovir. Australas J Dermatol. 2003. 44:203–206.

7. Tsao KC, Chang PY, Ning HC, Sun CF, Lin TY, Chang LY, et al. Use of molecular assay in diagnosis of hand, foot and mouth disease caused by enterovirus 71 or coxsackievirus A 16. J Virol Methods. 2002. 102:9–14.

8. Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's histopathology of the skin. 2008. 10th ed. Philadelphia: Lippincott Williams & Wilkins;658.
9. Higgins PG, Warin RP. Hand, foot, and mouth disease. A clinically recognizable virus infection seen mainly in children. Clin Pediatr (Phila). 1967. 6:373–376.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download