Abstract
Orofacial granulomatosis (OFG) is a term used to describe swelling of the orofacial area, mainly in the lips, secondary to an underlying granulomatous inflammatory process. OFG has been reported in association with systemic conditions such as sarcoidosis and Crohn's disease (CD). OFG may precede gastrointestinal disease, such as CD, by several years and may be the only obvious focus of the disease. Herein, we report a patient with OFG and non-symptomatic ulcerations of the ileocecal valve. The patient received intralesional triamcinolone injections every 2 weeks. After 6 weeks, all oral lesions showed marked improvement. The favourable treatment response of this patient suggests that intralesional triamcinolone can be used as a treatment option for patients with CD that have oral lesions. In addition, patients presenting with OFG should be carefully evaluated for gastrointestinal signs and symptoms.
Orofacial granulomatosis (OFG) is a term used to describe swelling of the orofacial area, mainly in the lips, secondary to an underlying granulomatous inflammatory process1. Cheilitis granulomatosa (CG) is the histopathological description of such inflammation occurring in the lips and surrounding tissues1. CG has been reported in association with systemic conditions such as sarcoidosis and Crohn's disease (CD)2. We report a rare case of OFG associated with CD that showed a favorable response to intralesional injections of triamcinolone.
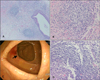
A 51-year-old woman presented with a 6-month history of progressive swelling of the upper and lower lips and buccal mucosa. Physical examination showed marked swelling of the upper and lower lips, with cobble-stone like appearance of the buccal mucosa and sublingual space (Fig. 1A-C). Biopsy samples from the buccal mucosa and sublingual space showed a non-caseating granuloma with scattered perivascular chronic inflammatory cells (Fig. 2A and B). History and examination, including chest X-ray, excluded tuberculosis and sarcoidosis. Routine histopathological examination together with PAS and AFB stain excluded tuberculosis and foreign body inclusions. According to the clinical and histopathological findings, a diagnosis of OFG was made. The patient received intralesional injections of triamcinolone every 2 weeks. After 6 weeks, all oral lesions showed marked improvement (Fig. 1D). In addition, there was no clinical worsening in the patient 6 months after three sessions of treatment.
Based on the findings of previous reports2, although the patient had no intestinal symptoms, a colonoscopy was performed. The colonoscopy showed minor ulcerations and erosions around the ileocecal valve (Fig. 2C). Mucosal biopsies from the terminal ileum revealed aphthous ulcerations and infiltration by inflammatory cells (Fig. 2D). Although the patient did not require active treatment for the colon lesions, being asymptomatic, the impression was early CD. The patient planned to follow-up with a gastroenterologist in order to monitor the state of the intestinal lesions.
OFG is a rare granulomatous disorder, characterized by persistent enlargement of the soft tissues of the oral and maxillofacial region3. Recurrent facial swelling, with/without intraoral manifestations, was the single most common presentation at onset4.
The nomenclature of OFG lacks specificity3. Recently, a question has been posed to determine whether OFG is a manifestation of a separate and specific inflammatory bowel disease5. Other authors also suggested that OFG is a descriptive term and the specific cause of these lesions is unknown6. Bogenrieder et al.6 reported that OFG is not an entity but is rather a generic name applied as a provisional diagnosis for orofacial lesions in patients where the associated systemic or local disease process has not yet been identified. OFG may precede gastrointestinal disease by several years and may be the only obvious focus of disease6,7. In this regard, Scully et al.8 found that 37% of patients, having no intestinal symptoms but with clinical evidence of oral CD, had demonstrable intestinal disease. Sanderson et al.5 also found that endoscopic and histologic intestinal abnormalities were common in patients with OFG and without gastrointestinal symptoms. Therefore, dermatologists should consider the presence of an OFG as a possible early sign suggestive of another inflammatory intestinal disorder, such as CD.
Several prior studies have suggested different treatment modalities for oral CD, ranging from the use of mouthwash with corticosteroids to intravenous infusions of an infliximab9. Consistent with the findings of previous reports10, a favourable outcome in our patient, using intralesional triamcinolone, is suggestive that this can be used as a treatment option for patients with CD that have oral lesions. The symptoms associated with CD usually show a clinical course that waxes and wanes. If patients with CD complain of symptoms associated with these oral lesions during the course of their disease, treatment of the oral lesions with intralesional triamcinolone can improve the quality of life of the patients by ameliorating associated disease symptoms.
In conclusion, patients presenting with an OFG should be carefully evaluated for gastrointestinal signs and symptoms such as diarrhea, hematochezia and abdominal pain. Even in cases with no presenting gastrointestinal symptoms, intestinal disease might exist on closer examination, thus investigation of the GI tract is highly suggested. Intralesional triamcinolone injections can be successful in relieving symptoms associated with oral lesions in a CD patient.
Figures and Tables
Fig. 1
(A) Marked swelling of upper and lower lips. (B, C) Cobble-stone like appearance of the buccal mucosa and sublingual space (asterisk=the site of biopsy). (D) Six weeks after intralesional triamcinolone injections every 2 weeks, the oral lesions showed marked improvement.

Fig. 2
(A, B) Biopsy samples from the buccal mucosa showed non-caseating granuloma with scattered perivascular chronic inflammatory cells (A: H&E, ×100, B: H&E, ×400). (C) The colonoscopic findings showed minor ulceration around the ileocecal valve (black arrow). (D) Mucosal biopsies from the terminal ileum revealed aphthous ulcerations and infiltration by inflammatory cells (H&E, ×400).
References
1. Triantafillidis JK, Valvi FZ, Merikas E, Peros G, Galitis ON, Gikas A. Granulomatous cheilitis associated with exacerbations of Crohn's disease: a case report. J Med Case Reports. 2008. 2:60.

2. Wiesen A, David O, Katz S. Cheilitis granomatosa: Crohn's disease of the lip? J Clin Gastroenterol. 2007. 41:865–866.
3. Grave B, McCullough M, Wiesenfeld D. Orofacial granulomatosis--a 20-year review. Oral Dis. 2009. 15:46–51.
4. Al Johani K, Moles DR, Hodgson T, Porter SR, Fedele S. Onset and progression of clinical manifestations of orofacial granulomatosis. Oral Dis. 2009. 15:214–219.

5. Sanderson J, Nunes C, Escudier M, Barnard K, Shirlaw P, Odell E, et al. Oro-facial granulomatosis: Crohn's disease or a new inflammatory bowel disease? Inflamm Bowel Dis. 2005. 11:840–846.

6. Bogenrieder T, Rogler G, Vogt T, Landthaler M, Stolz W. Orofacial granulomatosis as the initial presentation of Crohns disease in an adolescent. Dermatology. 2003. 206:273–278.

7. William T, Marsch WC, Schmidt F, Kreft B. Early oral presentation of Crohn's disease. J Dtsch Dermatol Ges. 2007. 5:678–679.

8. Scully C, Cochran KM, Russell RI, Ferguson MM, Ghouri MA, Lee FD, et al. Crohn's disease of the mouth: an indicator of intestinal involvement. Gut. 1982. 23:198–201.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download