Abstract
Herpes zoster is characterized by unilateral grouped vesicles along the distribution of a single dermatome. Disseminated herpes zoster usually is defined as a generalized eruption of more than 20 extra-dermatomal vesicles occurring within a week of the onset of classic dermatomal herpes zoster. It occurs chiefly in old or debilitated individuals, and especially in patients with underlying malignancy, immunosuppressive therapy, or human immunodeficiency virus (HIV) infection. A 51-year-old man presented with segmental grouped vesicles on the left upper trunk and arm, and a varicella-like eruption over the entire body. Tzanck smear preparation and punch biopsy done on the vesicles of the trunk indicated a herpetic infection. Later, he was found to be HIV-positive. We report a rare case of HIV infection initially presenting with disseminated herpes zoster.
Herpes zoster classically occurs unilaterally within the distribution of a single cranial or spinal sensory nerve. It presents with a unilateral radicular pain and a vesicular eruption which is limited to a dermatome innervated by that nerve. Depending on which dermatome is affected, many clinical variations are possible: (herpes) zoster ophthalmicus, zoster myelitis, disseminated zoster, zoster duplex bilateralis or unilateralis, and zoster multiplex1,2. Disseminated herpes zoster, defined as at least 20 lesions in multiple dermatomes, occurs in 2~10% of unselected patients with localized zoster, most of whom have immunologic defects (underlying malignancy, immunosuppressive therapy, or human immunodeficiency virus (HIV) infection)3. Also, systemic dissemination to the lung, brain, and liver, and subsequent death in disseminated herpes zoster have been documented4. Disseminated herpes zoster in HIV-seropositive individuals is less commonly reported and may be the initial manifestation of HIV infection5,6, as it was in the case we are about to present: disseminated herpes zoster with HIV infection, which has not yet been reported in the Korean literature.
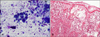
A 51-year-old homeless man presented with a 5-day history of painful vesicles. Initially, 5 days before coming in, he recognized lesions on the left trunk and upper arm (T2 dermatome) as several grouped vesicles with a pricking pain. Four days later, he developed multiple scattering erythematous vesicular rashes with mild pruritus over the entire body, and more ulcerative wounds associated with sharp pain on the previous lesions (Fig. 1). His past medical and family history was unremarkable. On the visit, laboratory examinations including complete blood cell counts, routine urinalysis, liver function test, and chest X-ray, which were all unremarkable or within normal limits. Tzanck smear test was done on the vesicles of the left trunk, which demonstrated multinucleated giant cells, characteristic of herpetic infection (Fig. 2A). Skin biopsy of a vesicular lesion on the abdomen revealed intraepidermal vesicle with acantholysis and balloon cells (Fig. 2B). Serologically, VZV IgM antibody was reported as negative and VZV IgG antibody was reported as positive by enzyme immunoassay (EIA). In the hospital, the HIV ELISA test was noted to be positive. This was confirmed by a western blot analysis (Fig. 3). Based on the his statement, it was assumed that the patient had been infected by sexual intercourse with a prostitute, having denied any other possibility for HIV transmission, including operations, transfusion, drug abuse, and homosexuality. He was treated with an IV antiviral agent and then referred to the Department of Internal Medicine for the further evaluation and status of HIV infection. He refused the further evaluation and then escaped from hospital.
Herpes zoster is caused by reactivation of latent varicella zoster virus (VZV) which lies dormant in the ganglia. Although the mechanisms of VZV reactivation from latency are unclear, its association with immunosuppression and age suggests that an effective immune system maintains the viral genome in the latently infected cell and prevents viral replication4,7. Therefore, immunosuppression, especially organ transplantation, hematologic malignancy, and HIV infection, increase the rates of zoster occurrence. While typical herpes zoster is characterized by unilateral, segmental painful vesicles over certain affected dermatomal region, herpes zoster in the immunosuppressed may be ulcerative and necrotic and may scar more severely. Also, multidermatomal involvement and disseminated infections are more common than they are in healthy individuals1. Disseminated herpes zoster is defined as more than 20 small widespread vesicles resembling varicella outside the area of the primary and adjacent dermatomes, and may or may not involve visceral organs. It has been mainly described in the elderly or persons with immunosuppression due to HIV infection, hematologic malignancy, or chemotherapy; in otherwise healthy individuals it is very rarely reported5,8,9. Therefore, a patient with disseminated herpes zoster, with no known co-factors (as noted above) deserves a complete work-up to elucidate any underlying malignancy or immunodeficiency3,4,10,11.
In this decade, HIV infection has been one of the most common causes of immunosuppression. Herpes zoster often occurs as the first manifestation of the compromised immune function of progressive HIV infection and often indicates a HIV infection with an increased probability of the subsequent development of acquired immune deficiency syndrome (AIDS)12,13. Friedman-Kien et al.14 in 1986 described that the incidence of herpes zoster in HIV-positive individuals is seven times greater than that of the general population. Thus, HIV infection should be considered in individuals who develop herpes zoster, and especially in those who develop disseminated herpes zoster associated with immunosuppression.
Cohen and Grossman6 reported clinical features of HIV-associated disseminated herpes zoster and compared it to those observed in HIV-seronegative immunosuppressed patients. They stated that systemic dissemination and subsequent death have been documented in 26% of HIV-seropositive patients. To compare with HIV-seronegative immunosuppressed patients, in these people there was an increased severity of cutaneous lesions noted, and as well, the course of disease could be prolonged or recurrent. Although our patient was not evaluated for the immune status precisely, the lesions quickly became necrotic and were associated with severe pain, thereby suggesting a considerable HIV-seropositive immunosuppressed state in our patient.
Most disseminated herpes zoster in HIV-seropositive patients have occurred in those who have had prior opportunistic infections associated with AIDS6. But, disseminated herpes zoster may be the first manifestation of HIV infection. Therefore, it is important to recognize this disease as having a high predictive value for HIV infection, and therefore perform necessary lab work to ascertain HIV status5,6,12. In our case, HIV seropositivity was incidentally found in the process of laboratory evaluation for systemic factors associated with disseminated herpes zoster without other AIDS-related manifestations. Prompt treatment with systemic antiviral agents is warranted in HIV-associated herpes zoster, because of the increased severity of cutaneous lesions and poor prognosis6,13.
To our knowledge, disseminated herpes zoster in HIV-seropositive patients has not yet been described in the Korean literature because HIV infection is a relatively uncommon entity in Korea, compared to some other region (i.e. Africa), where the prevalence of AIDS is high and the AIDS-related diseases have been frequently reported15. Thus we have reported a rare case of disseminated herpes zoster as being the first manifestation of HIV infection.
Figures and Tables
 | Fig. 1Grouped vesicles with hemorrhagic crusts on the side of trunk and upper arm and multiple scattering erythematous vesicular rashes on the whole body. |
References
1. Shin BS, Seo HD, Na CH, Choi KC. Case of herpes zoster duplex bilateralis. J Dermatol. 2009. 36:95–97.

2. Vu AQ, Radonich MA, Heald PW. Herpes zoster in seven disparate dermatomes (zoster multiplex): report of a case and review of the literature. J Am Acad Dermatol. 1999. 40:868–869.

3. Straus SE, Oxman MN, Schmader KE. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Varicella and herpes zoster. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1885–1898.
4. James WD, Berger TG, Elston DM. Andrews' diseases of the skin: clinical dermatology. 2006. 10th ed. Philadelphia: WB Saunders;379–384.
5. Cohen PR, Beltrani VP, Grossman ME. Disseminated herpes zoster in patients with human immunodeficiency virus infection. Am J Med. 1988. 84:1076–1080.

6. Cohen PR, Grossman ME. Clinical features of human immunodeficiency virus-associated disseminated herpes zoster virus infection--a review of the literature. Clin Exp Dermatol. 1989. 14:273–276.

7. Kennedy PG, Steiner I. A molecular and cellular model to explain the differences in reactivation from latency by herpes simplex and varicella-zoster viruses. Neuropathol Appl Neurobiol. 1994. 20:368–374.

8. Gupta S, Jain A, Gardiner C, Tyring SK. A rare case of disseminated cutaneous zoster in an immunocompetent patient. BMC Fam Pract. 2005. 6:50.

9. Burdett C, Mendoza N, Arora A, Bartlett B, Gewirtzman A, Tremaine AM, et al. A rare case of disseminated shingles in an immunocompetent patient following a 7-day treatment with oral valacyclovir. J Clin Virol. 2008. 43:233–235.

10. Singal A, Mehta S, Pandhi D. Herpes zoster with dissemination. Indian Pediatr. 2006. 43:353–356.
12. Petrozza JC, Monga M, Oshiro BT, Graham JM, Blanco JD. Disseminated herpes zoster in a pregnant woman positive for human immunodeficiency virus. Am J Perinatol. 1993. 10:463–464.

13. Gulick RM, Heath-Chiozzi M, Crumpacker CS. Varicellazoster virus disease in patients with human immunodeficiency virus infection. Arch Dermatol. 1990. 126:1086–1088.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download