Abstract
Background
Although molluscum contagiosum (MC) resolves spontaneously, there are several reasons to treat this dermatological disorder.
Objective
To evaluate the safety and efficacy of 5% imiquimod cream versus 10% potassium hydroxide (KOH) solution in treating MC, and to propose the mechanism of cure by observing the histological findings.
Methods
Imiquimod or KOH were applied by the patient or a parent 3 days per week until all lesions cleared. The number of MC lesions was counted and side effects were evaluated at 5 points during the treatment (the initial visit, week 2, week 4, week 8, and week 12). Histological changes were compared between 2 patients of each group, before and after the 2 weeks of application.
Results
In both group, the mean lesion counts decreased all through to week 12, and the reduction in number of lesions were statistically significant in both groups (p <0.005). Over 40% of each group developed local side effects, and no systemic side effects were noted in either group. Before treatment, histological findings showed little or no dermal infiltrates. After treatment, specimens showed dense lymphocytic infiltrates, especially T cells, around the lesions which had resolved.
Molluscum contagiosum (MC), the most common viral skin infections (2~8%) in children, is a self-limiting epidermal papular condition caused by the Molluscipox virus1. Although spontaneous resolution of the lesions occurs, there are several reasons to treat them2. Firstly, the lesions are cosmetically unattractive. As well, 10% of patients develop a pruritic, eczematous dermatitis around the MC lesions. Lastly, the lesions are numerous and recurrent with no other coexisting immunological problem, in about 4% of children with MC and therefore aide in resolution results in an end to recurrence of the lesions. Therefore we evaluated and compared the efficacy and safety of 2 topical and painless agents to treat MC: 5% imiquimod cream and a 10% potassium hydroxide (KOH) solution. Imiquimod cream is an immune response modifier that functions via induction of IFN-α and TNF-α, and also stimulates cell-mediated immunity3. KOH, on the other hand, resolves MC by dissolving keratin and destroying the skin4.
In order to assess the mechanism of cure, we compared the histological findings of MC after 2 weeks of treatment with each agent to the histological findings before the treatments.
After giving standard information and education to the patients or their guardians and signed informed consent was attained, 30 subjects between the ages of 1 and 36 who presented with clinical features of MC were included in the study, which took place between December 2008 and September 2009. The inclusion criterion was the presence of a minimum of 5 lesions in patients who were willing to return for follow-up visits. Patients with eyelid involvement, secondary infection, pregnancy and history of hypersensitivity to imiquimod were excluded. History, regarding age, sex, disease duration, anatomical location, accompanied symptom, and previous treatment taken was noted for each subject.
Out of a total of 30 patients, 15 patients were randomly assigned to the imiquimod group and the rest to the KOH group. Imiquimod and KOH were applied by the patient or a parent 3 times per week until the lesions disappear completely. Both agents were applied at night to the lesional skin only and were then washed off in the morning. Imiquimod was applied directly on the lesion, while KOH was applied with a cotton swab. At the initial visit and at the end of week 2, week 4, week 8, and week 12, the number of MC was counted and a photographic assessment was done. At week 12, tolerability was evaluated by asking about local (erythema, itching, burning, pain, erosion, crusting) and systemic (fever, influenza-like illness, diarrhea, headache, myalgia) side effects. If the lesions cleared early, the treatment period could be less than 12 weeks.
For all the statistical analyses, we used the Korean version, SPSS version 12.0 for Windows, and MedCalc for Windows version 9.6.4.0. A p-value <0.05 was considered statistically significant. We compared efficacies of the 2 treatments using the Mann-Whitney U test, and to compare the number of lesions at different weeks we used the Wilcoxon rank sum test.
Histological changes were evaluated and compared between 2 patients of each group, before and after the 2 weeks of application of each agent. To see the nature of the infiltrated inflammatory cells, CD3+ staining was done.
Out of 30 patients, 3 patients were noncompliant and did not follow-up. Fourteen patients in the imiquimod group and 13 patients in the KOH group completed the study. The age of the patients ranged from 1 to 36 years. The mean age of patients in the imiquimod and KOH groups were 3.70 years and 5.86 years, respectively. In the imiquimod group, 6 cases were males and 8 cases females. In the KOH group, 3 cases were males and 10 cases females. The minimum duration of disease was 21 days, and the maximum duration was 2 years. The mean duration of treatment was 4.29 months for the imiquimod group and 4.59 months for the KOH group. Out of 30 patients, 17 had lesions over the whole body, while 13 patients had localized lesions only. That is to say, 5 patients had lesions on the face (including neck and scalp), 4 patients on the trunk, 2 patients on the inguinal area (including the genital area), and 2 patients on the legs. Fifteen patients had pruritis resulting in scratching and autoinoculation. In these cases, a systemic anti-histamine was also prescribed. Four patients had eczematous lesions around the molluscum papules. One of them had atopic dermatitis, 1 had xerotic eczema, and 2 had molluscum dermatitis. Before they were included in this study, 23 patients were advised to "wait and see" at the local clinic. However, they searched for a therapeutic approach, as the number of lesions gradually increased, or the lesions affected their social activities. Four patients were treated with topical antibacterial ointments. Two patients underwent curettage, which removed the lesions rapidly and effectively, however, when the lesions recurred, these patients refused to be re-treated, due to pain and fear. The last patient was treated with herbal medicine, which had no noted effect.
We found complete clearance of lesions in 8 (57%) out of 14 patients with imiquimod, of which 7 patients were cleared of lesions by 4 weeks, and 1 by 8 weeks. However, 2 patients showed no responses until week 12. We observed a total clearance of lesions in 10 (77%) out of 13 patients with KOH. Out of these 10 patients, 6 were cleared of lesions by 4 weeks and the other 4 patients by 8 weeks. However, 1 patient showed no response until week 12.
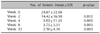
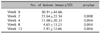
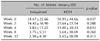
In both groups, the mean lesion counts decreased all throughout the follow-up period (Fig. 1, 2 and Table 1, 2). In addition, the reduction in number of lesions at the end of week 4, week 8, and week 12 were statistically significant in both groups (p-value<0.005) (Table 1, 2). We observed a decrease of lesions counted at week 2, but it was not statistically significant. Further, the differences of the number of lesions between the 2 groups at week 2, week 4, week 8 and week 12 were not statistically significant (Table 3).
At week 12, 6 (46%) out of 13 patients in the imiquimod group and 6 (42%) out of 14 patients in the KOH group experienced side effects. The side effects were observed on the site of application and included erythema, ulceration, scaling and hyperpigmentation. In most cases, the side effect was transient and tolerable, however, 2 patients in the imiquimod group and 1 patient in the KOH group discontinued the treatment because they could not tolerate the local irritation. Systemic adverse effects such as flu-like symptoms were not observed in either groups.
Before the treatment, histological findings of MC from 4 cases showed many epidermal cells containing large, intracytoplasmic inclusion bodies. The surrounding dermis shows little or no inflammatory reaction (Fig. 3). In contrast, histological findings after 2 weeks of application of imiquimod showed increased lymphocytic infiltrates around and into the lesions (Fig. 4A, B). By use of CD3 stains, T cell lymphocyte markers and cells around the MC were stained (Fig. 4C, D). Similarly, histological findings after 2 weeks of application of KOH showed increased lymphocytic infiltrates around and into the lesions (Fig. 5A, B). The infiltrated lymphocytes were stained with CD3 (Fig. 5C, D).
According to our study, the most commonly chosen treatment method of MC is "wait and see", including topical antibiotics in Korea, because MC usually resolve spontaneously. However, the lesions take between 6 and 18 months to resolve and are a source of great embarrassment, often limiting social activity5. Therefore many patients visit another doctor to attain treatment of MC that has persisted or is spreading6. Unfortunately some patients express anger towards their doctors because they were told the lesions would go away without treatment.
The next commonly used therapy is curettage. This focuses on the treatment of visible lesions, leaving the surrounding subclinical MC lesions as areas of possible occurrence of new lesions or transmission7. As a result, in a recent study, the treatment of MC by curettage is associated with a high risk of relapse, especially in cases with numerous lesions, numerous number of involved anatomical sites and concomitant atopic dermatitis7. In addition, curettage may be associated with scarring and is not well tolerated by children if performed repeatedly, owing to pain and fear8.
For these reasons various topical treatments are tried. Those include immune-modulating therapies like imiquimod, and keratolytic agents such as KOH, lactic acid, glycolic acid, salicylic acids, and the vesicant cantharidin, as well as topical retinoids such as tretinoin, tazarotene, and adapalene2,9. Among them, we chose 5% imiquimod cream and 10% KOH solution which are both easily obtainable in Korea.
Open-label trials and some case reports have suggested that imiquimod might be beneficial for MC8,10. One double-blind, placebo controlled trial involving 23 children found a significant decrease in the number of molluscum lesions within 12 weeks of imiquimod being applied three times per week, compared to placebo11. In these studies, the adverse reactions to imiquimod cream are reactions at the site of application, including erythema, ulceration, edema and scaling.
Romiti et al.4 suggested 10% KOH solution as a safe, effective and inexpensive, noninvasive treatment of MC. The only defect of KOH treatment was local side effects which included a stinging sensation around the site of application, and hyper-or hypopigmentation. For this reason they had tried 5% KOH solution and consequently had less irritation12.
In our study, both 10% KOH solution and 5% imiquimod cream are effective in the treatment of MC. There was no significant difference in their effectiveness. Our study shared similar results with Metkar et al.13's report, which compare 5% imiquimod cream to 10% KOH solution in the treatment of MC13. Our results, however, showed a higher rate of complete clearance than did the previous report of Metkar et al.13 (57% vs 44% in imiquimoid group, 77% vs 42.1% in KOH group). We observed faster clearance of lesions in the KOH group compared to the imiquimod group, but there was no statistic significance. The relatively long time to see the effect of imiquimod may be due to cell mediated immune response with imiquimod14.
Both treatments were almost safe. Over 40% of patients experienced a local irritation but most of them were tolerable. A few patients, however, discontinued the treatment due to the local irritation. No systemic adverse effects were observed.
The histological features of MC are: lobulated, endophytic hyperplasia of keratinocytes which contain a very large intracytoplasmic inclusion, and there are usually no dermal infiltrates1. Interestingly, the biopsy specimens of MC treated with both agents showed dense lymphocytic infiltrates, especially T cells, around the lesions which were resolved.
Some viruses, such as rubeola and HIV, have an ability to evade or suppress the host's immune response. In doing so they can spread themselves efficiently or establish a persistent infection15,16. In our opinion, MC may have a similar ability to suppress the host's immune response, so that there are usually no dermal infiltrates around intact MC lesions. In particular, T cells, which take a central position in antiviral defense, maybe the predominant target of MC-induced immunosuppression. In this situation, the application of imiquimod induces innate and cell-mediated immune response that inhibit MC-induced immunosuppression and eliminate the infection of MC. Similarly, KOH, which is strongly alkaline, can digest keratin and destroy the skin, in doing so causing inflammatory reactions that may break MC-induced immunosuppression and cure MC.
There are some limitations to this study. First, our study design did not take spontaneous clearing of MC lesions into consideration. Secondly, the number of clinical cases is too small so we used the Mann-Whitney U test rather than student T test. These results are preliminary, so we'll collect more cases. Third, more histological and molecular studies are required to establish the mechanism of cure.
In conclusion, both 10% KOH solution and 5% imiquimod cream are effective and safe treatments of MC. On top of that, they have an advantage over curettage because they are less traumatic, less painful, and easier to administer (at home). These characteristics make them particularly helpful in the treatment of MC in children. Considering the low cost and faster clearance of lesions using KOH solution, it could be a better option in the treatment of MC.
Figures and Tables
Fig. 1
Decreased lesions in patients treated with 5% imiquimod cream, (A) before treatment, (B) after 1 month of treatment.

Fig. 2
Decreased lesions in patients treated with 10% KOH solution, (A) before treatment, (B) after 2 weeks of treatment.

Fig. 3
(A~D) Before the treatment. Molluscum contagiosum showed many epidermal cells which contain large, intracytoplasmic inclusion bodies. The surrounding dermis shows little or no inflammatoty reaction (H&E, ×100).

Fig. 4
After 2 weeks of application of 5% imiquimod cream. (A, B) The lesions showed increased lymphocytic infiltrates around and into the lesions (H&E, ×100). (C, D) By use of CD3 stains, T cell markers, cells around the lesion were stained (CD3, ×100).

References
1. Grayson W, Calonge E, McKee PH. McKee PH, Calonje E, Granter SR, editors. Infectious diseases of the skin. Pathology of the skin: with clinical correlations. 2005. 3rd ed. Philadelphia: Elsevier Mosby;838–992.
2. Scheinfeld N. Treatment of molluscum contagiosum: a brief review and discussion of a case successfully treated with adapelene. Dermatol Online J. 2007. 13:15.

3. Callen JP. Callen JP, Horn TH, Mancini AJ, editors. Immunomodulators. Dermatology. 2008. 2nd ed. Philadelphia: Mosby Elsevier;1974–1989.
4. Romiti R, Ribeiro AP, Grinblat BM, Rivitti EA, Romiti N. Treatment of molluscum contagiosum with potassium hydroxide: a clinical approach in 35 children. Pediatr Dermatol. 1999. 16:228–231.

5. Gould D. An overview of molluscum contagiosum: a viral skin condition. Nurs Stand. 2008. 22:45–48.

6. Roberts S. Warts and molluscum: an impractical guide. Arch Dis Child Educ Pract Ed. 2007. 92:199–200.
7. Simonart T, De Maertelaer V. Curettage treatment for molluscum contagiosum: a follow-up survey study. Br J Dermatol. 2008. 159:1144–1147.

8. Bayerl C, Feller G, Goerdt S. Experience in treating molluscum contagiosum in children with imiquimod 5% cream. Br J Dermatol. 2003. 149:Suppl 66. 25–29.

9. Cathcart S, Coloe J, Morrell DS. Parental satisfaction, efficacy, and adverse events in 54 patients treated with cantharidin for molluscum contagiosum infection. Clin Pediatr (Phila). 2009. 48:161–165.

10. Barba AR, Kapoor S, Berman B. An open label safety study of topical imiquimod 5% cream in the treatment of Molluscum contagiosum in children. Dermatol Online J. 2001. 7:20.
11. Theos AU, Cummins R, Silverberg NB, Paller AS. Effectiveness of imiquimod cream 5% for treating childhood molluscum contagiosum in a double-blind, randomized pilot trial. Cutis. 2004. 74:134–138. 141–142.
12. Romiti R, Ribeiro AP, Romiti N. Evaluation of the effectiveness of 5% potassium hydroxide for the treatment of molluscum contagiosum. Pediatr Dermatol. 2000. 17:495.

13. Metkar A, Pande S, Khopkar U. An open, nonrandomized, comparative study of imiquimod 5% cream versus 10% potassium hydroxide solution in the treatment of molluscum contagiosum. Indian J Dermatol Venereol Leprol. 2008. 74:614–618.

14. Arany I, Tyring SK. Activation of local cell-mediated immunity in interferon-responsive patients with human papillomavirus-associated lesions. J Interferon Cytokine Res. 1996. 16:453–460.

15. Schneider-Schaulies S, Dittmer U. Silencing T cells or T-cell silencing: concepts in virus-induced immunosuppression. J Gen Virol. 2006. 87:1423–1438.

16. Wainberg MA, Mills EL. Mechanisms of virus-induced immune suppression. Can Med Assoc J. 1985. 132:1261–1267.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download