Abstract
We report here on an 11-year-old child with a pustulovesicular eruption on her whole body, including her palms, soles and oral mucosa, and this was accompanied with fever. A serologic test was positive for IgM varicella zoster antibody and coxsackievirus A16 antibody. The histopathologic examination from the palm revealed intraepidermal pustules that showed neither inclusion bodies nor multinucleated giant cells. We made the final diagnosis, according to the serologic tests and histopathologic findings, as varicella combined with hand-foot-mouth disease caused by coxsackievirus A16 in a previously healthy child.
Varicella is an acute, highly contagious exanthem that's caused by primary varicella-zoster virus infection1. The characteristic vesicular eruption starts from the face and this rapidly spreads to the trunk, with relative sparing of the extremities1. The rash can also develop on the palms and soles, which is an extremely rare presentation of varicella1-4. The distinctive features of varicella lesions are that they are a polymorphous eruption from rose-colored macules to papules, vesicles, pustules and crusts that rapidly progress1. Vesicles can also develop in the mucous membrane and these rapidly rupture into shallow ulcers 2 to 3 mm in diameter1,4.
Hand-foot-mouth disease is caused by enteroviruses, including coxsackievirus A16 and enterovirus 71, and this disease is a benign, self-limited viral exanthem that most frequently affects children less than 10 years5. The characteristic papulovesicular eruptions involve the mouth and the palms and soles5. As a difference from the vesicles on the palms and soles, the vesicles in the mouth quickly erode and form yellow to gray erosions surrounded by an erythematous halo5.
An 11-year-old girl presented with a pustulovesicular eruption that was accompanied by fever and a sore throat. Her history revealed no atopy or recurrent infection.
The eruption consisted of scattered vesicles and pustules that had begun on the face and trunk. The lesions then spread rapidly to her extremities, including both the palms and soles, over a period of one day. The lesions on the face and trunk, except those on the palms and soles, showed vesicles, pustules and focal crusts associated with intense pruritus (Fig. 1). However, the lesions on the palms and soles appeared to be at the same stage of evolution, and they were accompanied by tenderness (Fig. 2). The chest X-ray was normal. A serologic test at first presentation was positive for IgM varicella-zoster antibody and it was negative for IgG varicella-zoster antibody, and a Tzanck smear from fresh vesicles on the abdomen revealed multinucleated giant cells. At first we thought the girl suffered from vericella and we started treatment with intravenous acyclovir and supportive therapy, including oral antihistamine and acetaminophen. The pustulovesicles on the face and trunk became almost crusted with administering the antiviral therapy on the 3rd day, although the eruptions on both the palms and soles didn't response despite treatment.
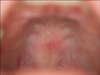
Atypical varicella, hand-foot-mouth disease, erythema multiforme and localized pemphigoid were considered as the differential diagnosis of the palmoplantar pustular eruption. Examination of the mouth revealed erosions covered with whitish membranes involving the buccal mucosa and hard palate (Fig. 3). An additional serologic test was positive (1:11) for the coxsackievirus A16 antibody titer (reference value: negative titer <1:4) and she was negative for enterovirus 71 antibody. The histopathologic examination from the pustular lesion on the palm revealed intraepidermal pustules with reticular degeneration that showed neither inclusion bodies nor multinucleated giant cells (Fig. 4). On the 7th day, the lesions on the palmoplantar area and oral mucosa became crusted and then they proceeded to heal spontaneously.
In our case, the distinctive features were the polymorphous eruption on the face and trunk, the monomorphous tender pustules on the palms and soles and the painful oral erosions. The skin lesions on the face and trunk showed multiple-staged papules, vesicles, pustules and crusts and these showed clinical improvement during the antiviral treatment. However, the tender pustules on the palms and soles were not improved or crusted 3 days later after starting antiviral treatment. The pustular eruption on the palmoplantar area was considered for making the differential diagnoses of atypical varicella, hand-foot-mouth disease, erythema multiforme and localized pemphigoid. We excluded localized pemphigoid because of its rare childhood presentation, its predilection for flexural areas and the subepidermal blisters that were without reticular degeneration6. In contrast to our case, erythema multiforme shows typical targetoid lesions on the extensor surface of the extremities and it is triggered by a preceding infection with herpes simplex virus or by drugs7,8. The histopathologic findings of erythema multiforme also exhibit spongiosis, vacuolar degeneration of the basal cell layer with satellite cell necrosis, and focal junctional and subepidermal cleft formation8.
The form of varicella that occurs most often in childhood is an acute, highly contagious exanthem that exists simultaneously with all stages of the skin lesions. The varicella with unusual clinical aspects and an unusual course is referred to as atypical varicella, and this is characterized by an unusual distribution and/or a prolonged course4,9. Atypical varicella has been associated with pre-existing factors such as an immunocompromised status, sun exposure, local injury and preexisting rash4,9. Our case was a healthy child without atopic dermatitis, recurrent infection or a history of trauma. The clinical features of our case were not consistent with varicella, and especially the painful oral erosion as well as the tender nonpruritic monomorphous pustules on the palms and soles. In contrast, Tzanck's test from the vesicles of the abdomen showed multinucleated giant cells, and the skin biopsy from the pustules of the palm showed only reticular degeneration without inclusion bodies or multinucleated giant cells. A serologic test was positive for IgM varicellazoster antibody and there was an elevated level of Coxsackievirus A16 antibody, although we didn't perform follow-up serologic testing. There was no clinical improvement of the palmoplantar lesions in contrast with that of the trunk and face. Based on the above evidence, we thought that our case was varicella coinfected with hand-foot-mouth disease.
Auvin et al4 have described atypical varicella with palm and sole involvement that showed the same stage of evolution with positivity for both IgM and IgG varicella-zoster antibodies and positivity for IgG B1-coxsackie antibody without IgM. They suggested that the intraepidermal lesions were caused by a pre-existing B1 coxsackie infection, meaning that subclinical hand-foot-mouth disease might explain the distal involvement in the cases of atypical varicella.
Our present case is a unique case that probably confirmed Auvin et al's explanation of varicella combined with hand-foot-mouth disease, as was proven by the serologic testing, Tzanck's test and the histopathologic examination. Varicella can be associated with a variety of diseases even in healthy persons. So clinicians must be aware of the atypical clinical manifestations of varicella and they must consider the involvement of concomitant disease such as a coinfection of virus or bacteria and blistering dermatitis3,4.
Figures and Tables
References
1. Straus SE, Oxman MN, Schmader KE. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Varicella and herpes zoster. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1885–1888.
2. Nagore E, Sanchez-Motilla JM, Julve N, Lecuona C, Oliver V. Atypical involvement of the palms and soles in a varicella infection. Acta Derm Venereol. 1999. 79:322.

3. Osawa M, Umemoto N, Tajima N, Sugawara H, Nishida J, Kakurai M, et al. Atypical varicella mimicking hand-foot-mouth disease in an adult patient with malignant lymphoma during chemotherapy. Br J Dermatol. 2004. 151:254–256.

4. Auvin S, Catteau B, Ganga-Zandzou PS, Ythier H. Atypical varicella with palm and sole involvement. Int J Dermatol. 2002. 41:903–905.

5. Dolin R. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Hand-foot-and-mouth disease. Fitzpatrick's dermatology in general medicine. 2008. 7th ed. New York: McGraw-Hill;1867–1869.
6. Mirza M, Zamilpa I, Wilson JM. Localized penile bullous pemphigoid of childhood. J Pediatr Urol. 2008. 4:395–397.

7. Oh YJ, Cho BK, Kim JW, Houh W, Lee YT. Hand, foot, and mouth disease: clinical and virological investigations. Korean J Dermatol. 1980. 18:409–416.
8. Scully C, Bagan J. Oral mucosal diseases: erythema multiforme. Br J Oral Maxillofac Surg. 2008. 46:90–95.

9. Legrand-Brogniart C, Auvin S, Catteau B, Dubos F, Vallee L. Bracelet localisation of chickenpox: a case of atypical varicella. Arch Pediatr. 2007. 14:259–261.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download