INTRODUCTION
Squamous cell carcinoma in situ on the mucosal or transitional surfaces is also referred to as erythroplasia of Queyrat (EQ). It is a premalignant dermatosis that usually occurs on the glans penis and appears as a well-marginated erythematous velvety patch or plaque. Analogous to Bowen's disease (BD), infiltration, nodularity or ulceration often suggest the possibility of conversion to an invasive squamous cell carcinoma. Although EQ resembles BD clinically and histologically, it may have a worse prognosis with a higher rate of malignant degeneration1. Removal of the cancer by partial or total penectomy is standard therapy, but radical procedures, such as penectomy may cause considerable mental distress, even to the point of suicide. Therefore, development of an alternative non-invasive treatment for EQ is essential. Topical imiquimod cream contains an immune-response modifier and has been known as an effective topical agent in the treatment of HPV-associated skin disorders and intraepithelial carcinoma. Here we report the case of a 56-year-old male suffering from erythroplasia involving the shaft of the penis and urinary meatus who had applied imiquimod 5% cream and had a good clinical result.
CASE REPORT
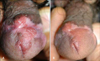
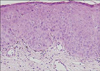
A 56-year-old circumcised man, with a 40-year history of psoriasis, visited our department for penile redness involving half of the urethral meatus without involvement of the urethral mucosa. He had been treated with a mid-potency corticosteroid cream and lotion for psoriatic skin lesions which were located on scalp, trunk and extremities. The patient did not receive PUVA or UVB phototherapy. On physical examination, an asymptomatic, relatively well defined, erythematous, shiny, slightly infiltrated area of plaque measuring 1.0×2.0 cm was observed on the glans penis and extended to the frenulum and the upper part of the penile shaft (Fig. 1A). The genital lesion first appeared several years prior and was considered to be psoriasis. He had applied topical vitamin D cream and topical tacrolimus ointment on the lesion for two months, but there was no clinical improvement. A skin biopsy was taken from the glans penis. Histopathologically, atypical keratinocytes at all levels of the epidermis with dyskeratosis, hyperchromatism and pleomorphism were noted. Intraepidermal dyskeratotic cells were observed as prematurely cornified individual keratinocytes and showed eosinophilic cytoplasm with a dense basophilic nucleus (Fig. 2). A small number of lymphocytes along the dermoepidermal junction were evident in the superficial dermis. Nested polymerase chain reaction and HPV DNA chip tests from the biopsy specimen was performed and HPV type 16 DNA was identified (Fig. 3). The patient was diagnosed as EQ, and imiquimod was applied to the lesion three times a week for 24 months. A month after initiation of treatment, the patient complained of a moderate burning sensation and erythema with watery discharge in the applied area. He had stopped applying imiquimod for a week and low-potency corticosteroid cream was used during the break interval. The treatment was well-tolerated overall and after 6-months of therapy, examination showed a marked clinical improvement, especially for the lesion near the urinary meatus, even though a follow-up biopsy and HPV identification were not done (Fig. 1B). However, a matchhead-sized erythematous nodule located on the lower part of the frenulum remained unchanged since the initiation of imiquimod treatment. Therefore, a complete excisional biopsy was done to rule out malignancy. The surgically excised penile lesion, which was unresponsive to topical Imiquimod, was confirmed to be squamous cell carcinoma in situ. At four months of follow-up (after the excision), the patient had continued to use topical imiquimod for two more months and had maintained a good clinical condition without recurrence.
DISCUSSION
EQ is a rare squamous cell carcinoma in situ of the penis. It was first described in 1911 by L. Queyrat as "erythroplasie du gland". It manifests itself as a red shiny patch or plaque limited to the glans, coronal sulcus, and prepuce. The surface resembles that of psoriasis or dermatitis, so the differential diagnosis for a plaque of psoriasis or dermatitis that gradually expands and never regresses must include precancerous dermatoses. Although EQ is histopathologically similar to BD, Graham and Helwig described EQ as a separate disease entity from BD1 and the differentiation between EQ and BD is a persistent source of arguments. We also presume that EQ is different from BD in various aspects. EQ presents as a shiny, velvety and bright erythematous plaque in gross appearance, but BD is usually described as a slightly pigmented area with scaly patches and plaques on the keratinized penis. Progression to an invasive SCC has been observed in up to 33% of cases of EQ, with metastases occurring in about 20% of patients with invasive carcinoma2. In contrast, progression to invasive SCC from BD was seen in approximately 3% for cutaneous3,4 and 10% for genital lesions3. It is suggested that EQ has a greater chance of becoming a malignancy than BD of the skin. The definitive etiology of EQ and BD is still unknown, but HPV 16 is probably responsible for a significant percentage of cases. In EQ, a strong association with HPV 16 was reported by previous studies and coinfection by HPV type 8 with types 16, 39 and 51 also have been identified. However, HPV type 8 was not detected in cervical or vulvar precancerous and cancerous lesions and in BD lesions5. Additionally, HPV DNA was found in 31% of extragenital Bowen's disease but no individual HPV type predominated in BD6. In terms of therapeutic effect, it was observed that EQ is less radiosensitive than BD1, and success rates of topical aminolevulinic acid photodynamic therapy for the treatment of EQ comparable to rates in BD have not been achieved7. The resistance of EQ to each treatment modality, in contrast to BD, may also represent a fundamental difference in tumor biology and pathogenesis between two disease entities.
Imiquimod, a heterocyclic imidazoquinolinamine, is a member of a new group of low molecular weight compounds and a topically active immunomodulatory agent that is formulated as a 5% cream8. However, its precise role as an immunomodulator at human skin sites has not been clearly determined. It is a chemical ligand for Toll-like receptor 7 and activates the host immune system by enhancing the release of endogenous cytokines such as IFN-alpha, IL-6, and tumor necrosis factor-alpha which are involved in innate immunity9. Moreover, imiquimod stimulates the acquired immunity system, which is important for control of viral infections and various tumors. This effect is triggered by IFN-alpha and IL-1210.
The treatment of EQ is often difficult and associated with significant recurrence rates, particularly in cases with urethral involvement. In patients with BD, clinical studies following treatment by imiquimod applied once daily 3 to 5 times per week for 8 to 16 weeks have been reported11. Recent reports suggest that topical imiquimod may also be effective in the treatment of EQ12. In our case, imiquimod treatment was chosen because surgical procedures including Mohs' micrographic surgery and partial penectomy often have cosmetic and functional results that make the patient miserable. We also used molecular methods to identify HPV DNA in the lesion. HPV type 16 was identified, which is a very high-risk oncogenic virus. In our case and in our patient, both antitumor and antiviral effects are considered to be the mechanism of action of imiquimod 5% cream (used 3 times a week for 24 weeks). The patient responded to imiquimod, but complete remission was not observed until 16 weeks after initiation of treatment. In a pilot study of patients with vulvar intraepithelial neoplasia, which is regarded as a counterpart of EQ, several patients showed clinical responses after 30 or 34 weeks of topical imiquimod treatment13. Therefore, we suggest that patients with EQ may get benefit from prolonged treatment over 16 weeks because of the differences between EQ and BD as we discussed above. To determine the optimal treatment regimen for patients with high-risk HPV positive EQ, further experiences and larger clinical trials are required.
In conclusion, topical imiquimod is recommended for EQ patients who are inappropriate candidates for total surgical excision. As in our case, a combination of prolonged application of imiquimod and subsequent excision of an imiquimod-resistant penile lesion can be considered as an appropriate treatment for EQ. However, the patients treated with imiquimod should be monitored with particular attention paid to the recurrence of disease.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download