Abstract
Syphilitic keratoderma is a rare cutaneous manifestation of secondary syphilis, characterized by symmetrical and diffuse hyperkeratosis of the palms and soles. In addition, no cases of syphilitic keratoderma and uveitis have been reported in the dermatologic literature. A 69-year-old woman presented with steroid-resistant hyperkeratotic patches on the palms and soles and uveitis for 4 months. As steroid-resistant uveitis must be evaluated for syphilis, viral infections, and autoimmune diseases, we ran several laboratory tests and the serologic test for VDRL was reactive (titer; 1:128). After treatment with penicillin G (4 MU, IV every 4 hours for 2 weeks), her skin lesions and visual disturbance were completely resolved. Therefore she was diagnosed as having syphilitic keratoderma and uveitis. Here, we report a rare case of syphilitic keratoderma concurrent with syphilitic uveitis and suggest that evaluation for syphilis may be required when skin lesions and ocular disturbance are resistant to long-term steroid therapy.
The cutaneous manifestations of secondary syphilis are variable, including macules, papules, nodules, annular and follicular eruptions, and commonly mimic those of other diseases. Syphilitic keratoderma is a rare form of cutaneous secondary syphilis. Ophthalmologic clinical findings of secondary syphilis are iritis, uveitis, and chorioretinitis. No cases of syphilitic keratoderma and uveitis in an immunocompetent patient have been reported in dermatologic literatures. Here we report a case of syphilitic keratoderma manifested as eczematous lesions associated with uveitis in an immunocompetent patient.
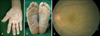
A 69-year-old woman presented for evaluation of hyperkeratotic scaly patches on her palms and soles. She also complained of progressive visual disturbance. Four months ago, asymptomatic scaly patches had developed on her palms and soles. Despite treatment with topical and systemic steroids for 4 months, the skin lesions were not improved. Two months ago, she developed visual blurring, and her visual acuity was not improved with systemic steroid and ophthalmic steroid suspension. Physical examination revealed symmetric erythematous hyperkeratotic scaly patches on palms and soles (Fig. 1A, B). KOH mount from the hyperkeratotic lesion was negative. Fundoscopic findings showed that optic disc was obscured by a dense vitreous haze, which suggested uveitis (Fig. 1C). She had divorced twenty years ago and could not recall her exact sexual contact history. As steroid-resistant uveitis must be evaluated for syphilis, viral infections, and autoimmune diseases, we ran VDRL, HIV antibody, HSV IgM, Toxoplasma IgG/IgM, CMV IgG/IgM, and rheumatic factor tests.
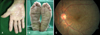
The VDRL titer was 1:128, and the FTA-ABS IgG/M test and TPHA were positive. Other laboratory findings were within normal limits. Skin biopsy was performed on the palm. Histological findings showed hyperkeratosis, parakeratosis, and dermal lichenoid infiltration with lymphocytes and sparse plasma cells (Fig. 2). Her CSF was also examined, because ocular syphilis tends to be associated with neurosyphilis. CSF study showed reactive FTA-ABS and lymphocytic pleocytosis. Upon diagnosis of syphilitic keratoderma with uveitis and asymptomatic neurosyphilis, she was treated with potassium penicillin G, 4 MU, IV every 4 hours for 2 weeks. After 2 weeks, her skin lesions and visual disturbance were completely resolved (Fig. 3A, B) and fundoscopic findings clearly showed the optic disc (Fig. 3C). There was no recurrence of skin lesions and the VDRL test titer decreased to 1:64 after 4 months of follow up.
Histopathological examination of the hypopigmented patch revealed hyperkeratosis, acanthosis in the epidermis, and perivascular inflammatory cells infiltration in the upper dermis (Fig. 2A). The dermal infiltrate consisted of lymphohistiocytes and sparse plasma cells (Fig. 2B). Although the patient was treated with topical steroid twice a day for 1 month, no regression of the lesions was observed.
Maculopapular and papulosquamous eruptions of the palms and soles, with or without a generalized rash, are distinctive and frequent features of secondary syphilis1. However, syphilis can also produce a unique volar skin change, called keratoderma, which is characterized by symmetrical and diffuse hyperkeratosis of the palms and soles2. Syphilitic keratoderma is clinically indistinguishable from other common dermatoses on volar aspects, such as keratoderma blenorrhagicum, hyperkeratotic eczema, and keratoderma associated with Unna-Thost syndrome or Howel-Evans syndrome3,4. It can be distinguished by laboratory findings, histological findings, and poor response to long-term steroid therapy. It can be treated with a single intramuscular injection of 2.4 MU of benzathine penicillin G.
This case was noteworthy because the patient displayed unusual manifestations of secondary syphilis, i.e., hyperkeratotic scaly patches on palms and soles. Due to a misdiagnosis of palmoplantar keratoderma, she had been treated with topical and systemic steroids for 4 months without improving. Her skin lesions were not typical manifestations of secondary syphilis, but reactivity in the serologic test for syphilis and the patient's excellent response to penicillin therapy established the correct diagnosis of syphilis.
Syphilitic uveitis can occur in all stages of syphilis, but frequently occurs during secondary and tertiary phases of the infection. In such cases, the patient presents with injected sclera and complains of pain, lacrimination, photophobia and visual impairment. Visual impairment can result from either focal macular involvement or opacifying inflammatory changes in the vitreous5. Ocular syphilis can be diagnosed after negative results from HSV PCR, CMV antibody, and toxoplasma antibody and positive specific treponemal serum antibody tests6. Patients with syphilitic uveitis are treated with high dose intravenous penicillin G therapy to resolve the ocular inflammation and improve their visual acuity.
During ocular syphilitic infection, spirochetes invade the meninges through CSF. So if a patient is diagnosed with ocular syphilis, he must undergo CSF evaluation. On CSF study, reactive VDRL or FTA, increased cell count, or increased protein suggest neurosyphilis. The recommended treatment for neurosyphilis is penicillin G crystalline, 3 to 4 MU intravenously every 4 hours for 10 to 14 days.
There are only two reported cases of syphilitic keratoderma, uveitis, and urethritis in HIV-positive patients2,7. Although our case is similar to those cases clinically, our patient was HIV-negative. To our knowledge, no cases of syphilitic keratoderma and uveitis in an immunocompetent patient have been reported. Therefore, we report this rare case and suggest that syphilis should be considered when skin lesions and visual blurring are resistant to long-term steroid therapy.
Figures and Tables
Fig. 1
Volar aspects of both hands (A) and both feet (B) show diffuse scaling and thickening. Fundoscopic findings showed that the optic disc was obscured by a dense vitreous haze, which suggested uveitis (C).
References
1. Dourmishev LA, Dourmishev AL. Syphilis: uncommon presentations in adults. Clin Dermatol. 2005. 23:555–564.

2. Radolf JD, Kaplan RP. Unusual manifestations of secondary syphilis and abnormal humoral immune response to Treponema pallidum antigens in a homosexual man with asymptomatic human immunodeficiency virus infection. J Am Acad Dermatol. 1988. 18:423–428.

4. Howel-Evans W, McConnell RB, Clarke CA, Sheppard PM. Carcinoma of the oesophagus with keratosis palmaris et plantaris (tylosis): a study of two families. Q J Med. 1958. 27:413–429.
5. Cubillan LD, Cubillan EA, Berger TG, Seiff SR, Crawford JB, Howes EL Jr, et al. Syphilitic uveitis and dermatitis. Arch Ophthalmol. 1998. 116:696–697.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download